Abstract
Objective
We intended to calculate approximate fetal doses in pregnant women who underwent diagnostic radiology procedures and to evaluate the safety of their pregnancies.
Materials and Methods
We contacted hospitals in different cities in Turkey where requests for fetal dose calculation are usually sent. Fetal radiation exposure was calculated for 304 cases in 218 pregnant women with gestational ages ranging from 5 days to 19 weeks, 2 days. FetDose software (ver. 4.0) was used in fetal dose calculations for radiographic and computed tomography (CT) procedures. The body was divided into three zones according to distance from the fetus. The first zone consisted of the head area, the lower extremities below the knee, and the upper extremities; the second consisted of the cervicothoracic region and upper thighs; and the third consisted of the abdominopelvic area. Fetal doses from radiologic procedures between zones were compared using the Kruskal-Wallis test and a Bonferroni-corrected Mann-Whitney U-test.
Results
The average fetal doses from radiography and CT in the first zone were 0.05 ± 0.01 mGy and 0.81 ± 0.04 mGy, respectively; 0.21 ± 0.05 mGy and 1.77 ± 0.22 mGy, respectively, in the second zone; and 6.42 ± 0.82 mGy and 22.94 ± 1.28 mGy, respectively, in the third zone (p < 0.001). Our results showed that fetal radiation exposures in our group of pregnant women did not reach the level (50 mGy) that is known to increase risk for congenital anomalies.
Many diagnostic radiological examinations involve ionizing radiation, such as computed tomography (CT), angiography, fluoroscopy, mammography, intravenous pyelography, and plain radiographs. The biological effects of radiation can be classified into two main groups: deterministic and stochastic effects (1). Deterministic effects are radiation-induced effects that occur if exposure to radiation exceeds a certain threshold, such as skin injuries, cataracts, alopecia, and sterility. In contrast, teratogenic and carcinogenic effects, which may occur depending on the dose, are called stochastic effects. In diagnostic radiology, the stochastic effects of radiation are especially undesirable for fetuses. The duration of exposure and the dose are the most important parameters for determining fetal effects. The type of diagnostic imaging modality (e.g., CT, fluoroscopy, radiography), energy of the photons (kVp), amount of photons (mA), total filtration, distance between the fetus and the mother's skin, and the skin thickness are the main determinants used for estimating the fetal dose of radiation.
Much of the information on the adverse effects of ionizing radiation was obtained from studies that investigated survivors of the atomic bombs at Hiroshima and Nagasaki (23). These studies included human data from 500 of the 2800 surviving pregnant women who were exposed to ionizing radiation of more than 10 mGy. According to these studies, radiation doses of approximately 10 mGy increase the risk, and possible fetal effects of radiation exposure are prenatal death, microcephaly, reduced intelligence quotient, organ malformation, mental retardation, intrauterine growth retardation, and childhood cancers. A dose of 100 mGy is often mentioned as the dose to a developing fetus at which a therapeutic abortion should be considered. Radiation safety standards have been established by international and national radiation protection organizations, such as the International Commission on Radiological Protection and the National Council on Radiation Protection and Measurements, to limit potential harmful radiation effects (45). The annual radiation dose limit is 1 mSv for the general public. On this basis, the risk of fetal damage at doses lower than 1 mGy is negligible, similar in fact to the risk to a fetus that is exposed to no radiation.
Sensitivity to radiation during pregnancy depends on the developmental stage. Generally, the key periods in pregnancy are the third stage of pre-implantation or blastogenesis (0-2 weeks), organogenesis (3-8 weeks), and fetal development from the ninth week until birth. If the embryo is exposed to radiation during the pre-implantation stage, the all-or-nothing rule applies (67). Accordingly, radiation-related damage typically leads to spontaneous abortion. In other stages, doses that enable normal fetal development do not lead to any increased risk of associated fetal abnormalities. However, if the dose to the fetus exceeds 100 mGy, the risk of malformations may increase (3). The aim of this retrospective study was to calculate approximate fetal doses in pregnant women who underwent radiological procedures and to evaluate the safety of their pregnancies.
In this study, from January 2013 to February 2015, data on 218 pregnant women who were exposed to ionizing radiation were investigated retrospectively. The study was approved by the Institutional Review Board of the institution in which the research was conducted. Because some of the patients had undergone more than one diagnostic procedure, the total number of examinations was 304 in 218 pregnant women: 162 women had undergone medical examinations only once, 37 of them twice, 13 of them three times, 3 of them four times, 2 of them five times, and 1 patient, seven times. The gestational ages of the 218 fetuses ranged from 5 days to 19 weeks, 2 days. When the distribution of fetal doses was analyzed in terms of gestational age, it was seen that 103 pregnant women were in weeks 0-4 of their pregnancies, 89 were in weeks 5-8, 20 were in weeks 9-12, and 6 of them were in weeks 13-19. According to these results, 212 pregnant women (-97%) were in the first trimester of pregnancy, and 6 (-3%) were in the second trimester. Of these, 13 of the women who underwent examinations (24 cases) were aware of their pregnancies by the time they underwent the examinations. Some patients in the third zone were followed up by the medical genetic department at their request to investigate any adverse effects.
All diagnostic examinations were performed with various radiography, fluoroscopy, and CT (ranged from 16 to 128 slice) machines from different manufacturers. Abdominal areas were covered with lead shielding during the imaging under physician supervision. The body was divided into three zones according to distance from the fetus. The first zone consisted of the head area, the lower extremities below the knee, and the upper extremities; the second consisted of the cervicothoracic region and upper thighs; and third part consisted of the abdominopelvic area.
Statistical analysis was performed using a dedicated software tool (SPSS 21.0 for Windows, IBM, Armonk, NY, USA). Variables were expressed as mean values ± standard deviation and range. A p value of < 0.05 was considered to be statistically significant. Radiographic and CT values in the three zones were evaluated statistically. Whether there was a normal distribution of CT values in each zone was evaluated with the Shapiro-Wilk test; it was seen that distribution was not normal. Accordingly, a Kruskal-Wallis analysis was used, and statistically significant differences were seen between zones (p < 0.001). A Bonferroni-corrected Mann-Whitney U-test was used to assess the differences (p = 0.05/3 = 0.016).
Pregnant women were referred to the Department of Medical Physics to determine the fetal radiation dose. Fetal radiation exposure was calculated by an expert physicist in this department. All of the pregnant women who were referred to the department were asked for documents that contained detailed information about the medical examination type, details of the procedure, and exposure parameters. To calculate the fetal dose, specific values for the following parameters were obtained for the medical examinations that were performed: 1) projection view (anteroposterior, posteroanterior, lateral, oblique) for each exposure; 2) imaging modality; 3) size of the X-ray field and image receptor plane or skin surface; 4) beam quality (peak tube potential, generator type and filtration); and 5) source-to-image receptor distance. Gestational age used in calculating the fetal dose was obtained using prenatal ultrasound data.
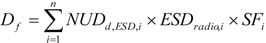
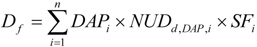
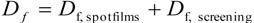
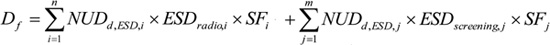
We used the FetDose V4 software to calculate fetal doses from the radiographic and CT examinations. FetDose is a widely used software program that was developed for estimating fetal radiation doses (8910). The fetal absorbed dose from a series of radiographic examinations (Df) when the quantity supplied was the entrance surface dose for each radiograph was calculated using the formula where n is the number of radiographs, NUDd, ESD is the uterine dose at a mean fetal depth d normalized to the entrance surface dose, and SFi is the fetal size factor (i.e., uterus-to-fetus dose conversion factor) for the field size used in the examination. If the quantity provided was the dose-area product per examination in Gy cm2, then the fetal absorbed dose from a series of radiographic examinations was calculated using the formula where NUDd, DAP is the uterine dose at mean fetal depth d normalized to the dose-area product, and DAPi is the dose-area product for each examination i. For examinations, that included fluoroscopy (e.g., barium enema, barium meal) and involved both spot films and screening procedures for different areas of the body, the total fetal dose was calculated by summing the contributions from both the spot films and the screening procedures: where n is the number of radiographic examinations or spot films and m is the number of screening procedures.
The fetal dose from CT series was calculated with the formula
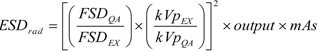
where CTDIsoft tissue (mGy / 100 mAs) is the CTDIair to the ICRU muscle (CTDIsoft tissue = CTDIair × 1.07) used as approximations for the dose to soft tissue within the body and NUDV is the sum of the normalized doses for all 5 mm slabs lying within the scan volume.
The average fetal doses from radiography and CT in the first zone were 0.05 mGy and 0.81 mGy; 0.21 mGy and 1.77 mGy in the second zone; and 6.42 mGy and 22.94 mGy in the third zone, all respectively. Fetal dose values are presented in Table 1 for the first zone, Table 2 for the second zone, and Table 3 for the third zone. Reference levels for CT protocols were presented in Table 4. Radiographic and CT values in the three zones were evaluated statistically, and all groups of CT dose values were significantly different from each other (p < 0.001). All of these statistics were applied to radiographic procedures in all zones, and statistically significant differences were noted in radiographic dose values (p < 0.001). Fetal doses from abdominal, pelvis, and lumbar CT scans were calculated for 13% of all examinations. The calculated fetal doses in 41 cases in 29 pregnant women who underwent abdominal and/or pelvic CT for trauma and appendicitis during the first trimester ranged from 9.1 to 41.6 mGy, with an average of 23.57 mGy. The calculated fetal doses in extracorporeal shock wave lithotripsy (ESWL) under fluoroscopy ranged from 12.20 to 25.90 at 2 to 10 weeks of gestation. No pregnant women underwent abdominal and/or pelvic CT during the second trimester. As a result, fetal radiation exposures did not reach the level (50 mGy) of increased risk for congenital anomalies in any zones, and no adverse effects were observed in the infants from the patients in the third zone.
It has also been reported that fetal doses below 100 mGy should not be considered a reason for terminating a pregnancy (34). The American College of Obstetricians and Gynecologists (11) published the following policy statement: "Women should be counseled that X-ray exposure from a single diagnostic procedure does not result in harmful fetal effects. Specifically, exposure to less than 50 mGy has not been associated with an increase in fetal anomalies or pregnancy loss." However, according to another study (12), fetal radiation doses in the area of 10 mGy produce a subsequent increase in the risk of childhood cancer. Most importantly, it should be appreciated that risks such as abortion (15%), congenital anomalies (3-5%), intrauterine growth retardation (4%), and mental retardation (1%) are always present in the pregnancy of every healthy woman (13).
The teratogenic effects of radiation are most serious between 2 and 20 weeks of gestation. Before the 2nd week and after the 20th week, the probability of ionizing radiation-related abnormalities in the baby is low. It is not known which anomalies emerge at which doses. In the fetus and areas close to the fetus (e.g., abdominal, pelvic), radiation exposure from a CT scan is important. The main indications for abdominal CT evaluations are major abdominal trauma, cancer staging, kidney stones, appendicitis, intestinal obstruction, and abscesses. In our study, the main indications for abdominal CT were trauma and appendicitis. Fetal radiation exposure at 0 and 3 months gestation was calculated with abdominal CT for renal stones and appendicitis by Hurwitz et al. (14). In that study, fetal doses at 0 month ranged from 15.2 mGy to 16.88 mGy for appendicitis and from 4 mGy to 7.2 mGy for renal stones. Fetal doses at 3 months were 19.9-32.2 mGy for appendicitis and 8.5-11.7 mGy for renal stones. In our study, the fetal doses in 41 cases in 29 pregnant women who underwent abdominal and/or pelvic CT during the first trimester ranged from 9.1 to 41.6 mGy, with an average of 23.57 mGy. The average and maximum fetal CT doses encountered in the literature are 8 and 49 mGy, respectively (5). For abdominal CT examinations, the mean fetal dose was 3 times higher and the maximum fetal dose was slightly lower in our study than in the literature. More recently, Parmaksız et al. (15) reported that fetal equivalent dose for CT ranged from 7.3 to 98.0 mSv, with an average of 28 mSv, slightly higher than in our study. In that study, fetal equivalent mean dose for abdominal X-ray examination was 7.6 mSv, whereas in our study, fetal equivalent mean dose for abdominal X-ray examination was 2.44 mSv. We think that these differences could be attributable to differences in imaging protocols and the different devices from different manufacturers. In abdominal CT, if imaging parameters can be optimized (decreasing mAs, modulating the z-axis, increasing the pitch), the fetal radiation exposure can be reduced (161718). CT, which uses high radiation doses, constitutes 40% of all radiation doses that are received in medical diagnostic examinations per year (1419). Radiographic, fluoroscopic, and CT examinations in areas of the body other than the abdomen and pelvis deliver minimal radiation doses to the fetus. The resulting fetal dose from radiographs of the chest, skull, and sinuses in the first zone were nearly zero and led to no abnormalities in the fetus, but the risks of childhood cancer and small head size caused by radiographs of the abdomen, lumbar spine, and pelvis areas in the third zone are debatable (2021).
In our study, calculated fetal doses in 6 patients in ESWL under fluoroscopy ranged from 12.20 to 25.90 at 2 to 10 weeks of gestation; these were not included in the statistical calculations. There have been reports of ESWL treatment in young women with unrecognized early pregnancies who went on to have uncomplicated pregnancies and healthy babies (2223). Obviously, it would be difficult to define prospectively whether it is safe to administer ESWL to pregnant women, and we do not encourage lithotripsy as a treatment for renal calculi in pregnancy, but unintentional lithotripsy in a pregnant woman is not a cause for concern.
The small number of patients and inhomogeneous distribution in each zone are the main limitation of this study. Additionally, we did not consider patient size or weight differences, even though radiation doses vary depending on the size of the individual. No pregnant woman had undergone an abdominal and/or pelvic CT during the second trimester in this study. Additional work in evaluating fetal radiation exposure in the second and third trimesters has yet to be accurately performed. In light of data from this study, health care providers can conduct more informed and informative dialogues with both patients and other providers (such as surgeons, obstetricians, emergency physicians, and nurses) concerning the potential risks of radiation in early pregnancy. These results also showed a need for education and increased awareness for radiology workers about simple patient protection procedures including optimizing the imaging protocols such as lowering the tube current, limiting coverage in the z-axis, and increasing the helical pitch.
In our study, based on statistical calculations, a protocol is recommended for radiologic procedures that have significant doses depending on the different parts of the body. Doses for any radiological procedures in the first zone were below 1 mGy and were considered to pose no risk to the fetus. Doses for all radiological procedures in the second zone were between 1 mGy and 5 mGy, and the risk was considered negligible. Although the doses for any radiological procedures in the third zone were well below the abortion threshold, follow-up of the pregnancy and the baby are recommended.
In conclusions, our results are consistent with the current literature with regard to the calculated fetal doses. In terms of calculated doses and their means for different radiologic procedures, the body was divided into three zones according to distance from the fetus. It was determined that in diagnostic radiology procedures, fetal radiation exposure did not reach risk levels that indicated abortion.
Figures and Tables
Table 1
Fetal Dose Arising from Diagnostic Radiology Procedures in Zone 1

Table 2
Fetal Dose Arising from Diagnostic Radiology Procedures in Second Zone

Table 3
Fetal Dose Arising from Diagnostic Radiology Procedures in Third Zone

Table 4
Reference Levels for CT Protocols

References
1. Hall EJ, Giaccia AJ. Radiobiology for the radiologist. 6th ed. Philadelphia: Lippincott;2006.
2. Valetin J. Biological effects after prenatal irradiation (embryo and fetus). ICRP Publication 90. Ann ICRP. 2003; 33:9–200.
3. Busby C, Lengfelder E, Pflugbeil S, Schmitz-Feuerhake I. The evidence of radiation effects in embryos and fetuses exposed to Chernobyl fallout and the question of dose response. Med Confl Surviv. 2009; 25:20–40.
4. 1990 recommendations of the International Commission on Radiogical Protection. Ann ICRP. 1991; 21:1–201.
5. International Commission on Radiological Protection. Pregnancy and medical radiation. ICRP Publication 84. Ann ICRP. 2000; 30(1):iii–viii. 1–43.
6. Brent RL. Saving lives and changing family histories: appropriate counseling of pregnant women and men and women of reproductive age, concerning the risk of diagnostic radiation exposures during and before pregnancy. Am J Obstet Gynecol. 2009; 200:4–24.
7. Roux C, Horvath C, Dupuis R. Effects of pre-implantation low-dose radiation on rat embryos. Health Phys. 1983; 45:993–999.
8. Osei EK, Faulkner K. Fetal doses from radiological examinations. Br J Radiol. 1999; 72:773–780.
9. Osei EK, Darko JB, Faulkner K, Kotre CJ. Software for the estimation of foetal radiation dose to patients and staff in diagnostic radiology. J Radiol Prot. 2003; 23:183–194.
10. Osei EK, Darko J. Foetal radiation dose and risk from diagnostic radiology procedures: a multinational study. ISRN Radiol. 2012; 2013:318425.
11. ACOG Committee on Obstetric Practice. ACOG Committee Opinion. Number 299, September 2004 (replaces No. 158, September 1995). Guidelines for diagnostic imaging during pregnancy. Obstet Gynecol. 2004. 104:p. 647–651.
12. Doll R, Wakeford R. Risk of childhood cancer from fetal irradiation. Br J Radiol. 1997; 70:130–139.
13. Wang PI, Chong ST, Kielar AZ, Kelly AM, Knoepp UD, Mazza MB, et al. Imaging of pregnant and lactating patients: part 1, evidence-based review and recommendations. AJR Am J Roentgenol. 2012; 198:778–784.
14. Hurwitz LM, Yoshizumi T, Reiman RE, Goodman PC, Paulson EK, Frush DP, et al. Radiation dose to the fetus from body MDCT during early gestation. AJR Am J Roentgenol. 2006; 186:871–876.
15. Parmaksız A, Ataç GK, Bulgurlu F, Bulur E, Öncü T, İnal T. Unintentional irradiation of conceptus by diagnostic imaging examinations in Turkey. Radiat Prot Dosimetry. 2014; 162:322–328.
16. Karabulut N, Ariyürek M. Low dose CT: practices and strategies of radiologists in university hospitals. Diagn Interv Radiol. 2006; 12:3–8.
17. Goo HW. CT radiation dose optimization and estimation: an update for radiologists. Korean J Radiol. 2012; 13:1–11.
18. Shin HJ, Chung YE, Lee YH, Choi JY, Park MS, Kim MJ, et al. Radiation dose reduction via sinogram affirmed iterative reconstruction and automatic tube voltage modulation (CARE kV) in abdominal CT. Korean J Radiol. 2013; 14:886–893.
19. Crawley MT, Booth A, Wainwright A. A practical approach to the first iteration in the optimization of radiation dose and image quality in CT: estimates of the collective dose savings achieved. Br J Radiol. 2001; 74:607–614.
20. McCollough CH, Schueler BA, Atwell TD, Braun NN, Regner DM, Brown DL, et al. Radiation exposure and pregnancy: when should we be concerned? Radiographics. 2007; 27:909–917. discussion 917-918
21. Chaparian A, Aghabagheri M. Fetal radiation doses and subsequent risks from X-ray examinations: should we be concerned? Iran J Reprod Med. 2013; 11:899–904.
22. Asgari MA, Safarinejad MR, Hosseini SY, Dadkhah F. Extracorporeal shock wave lithotripsy of renal calculi during early pregnancy. BJU Int. 1999; 84:615–617.
23. Deliveliotis CH, Argyropoulos B, Chrisofos M, Dimopoulos CA. Shockwave lithotripsy in unrecognized pregnancy: interruption or continuation? J Endourol. 2001; 15:787–788.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download