Abstract
Objective
This study strived to evaluate the relationship between degree of pulmonary emphysema and cardiac ventricular function in chronic obstructive pulmonary disease (COPD) patients with pulmonary hypertension (PH) using electrocardiographic-gated multidetector computed tomography (CT).
Materials and Methods
Lung transplantation candidates with the diagnosis of COPD and PH were chosen for the study population, and a total of 15 patients were included. The extent of emphysema is defined as the percentage of voxels below -910 Hounsfield units in the lung windows in whole lung CT without intravenous contrast. Heart function parameters were measured by electrocardiographic-gated CT angiography. Linear regression analysis was conducted to examine the associations between percent emphysema and heart function indicators.
Results
Significant correlations were found between percent emphysema and right ventricular (RV) measurements, including RV end-diastolic volume (R2 = 0.340, p = 0.023), RV stroke volume (R2 = 0.406, p = 0.011), and RV cardiac output (R2 = 0.382, p = 0.014); the correlations between percent emphysema and left ventricular function indicators were not observed.
In patients with chronic obstructive pulmonary disease (COPD), cor pulmonale could occur, which is characterized by elevated pulmonary vascular resistance and right heart failure with an associated reduction of the left ventricular diastolic function (1). This disorder might occur as a result of various mechanisms including loss of pulmonary vascular capacity due to lung parenchymal destruction or hypoxic pulmonary arterial vasoconstriction (2). Prior studies revealed that decreased expression of vascular endothelial growth factor causes endothelial apoptosis, epithelial apoptosis, and emphysema (3), which implied the existence of a complicated pathogenesis between emphysema and impaired pulmonary vascular capacity. Hyperinflation could cause intrathoracic pressure to exceed venous pressure, with the reduction of the blood volume returning to both ventricles (4). The elevated intrinsic positive end-expiratory pressure redistributes intrapulmonary and intracardiac blood volumes in emphysema patients (5). However, the detailed pathophysiology of emphysema on hemodynamics and cardiac function remains debatable.
Computed tomography (CT) emphysema quantification has already demonstrated a good correlation between histopathology and pulmonary function (6). In addition, multidetector CT (MDCT) not only accurately quantify ventricular function, as compared with cardiac magnetic resonance (MR) (7), but also evaluate right ventricle (RV) function in patients with COPD and cor pulmonale (8).
Recent population-based cohort studies revealed that a greater extent of emphysema on CT was linearly related to impaired left ventricular (LV) filling, reduced stroke volume, and lower cardiac output. These were measured by cardiac magnetic resonance imaging (MRI) across a spectrum of normal lung structure and function to severe emphysema and airflow obstruction (9). Further population-based study also showed that percent emphysema was inversely associated with RV end-diastolic volume, stroke volume, cardiac output, and mass using cardiac MRI (10).
The measurements of RV dysfunction can predict future right-sided heart failure, clinical deterioration, and mortality in patients with pulmonary hypertension (PH) (11). However, use of echocardiogram to measure RV dysfunction is technically problematic particularly in patients with severe emphysema (12). The relationship of the ventricular heart function of COPD patients to PH and pulmonary emphysema obtained in one single CT study is lacking. Our study aimed to evaluate the relationship between degree of pulmonary emphysema and cardiac ventricular function in COPD patients with PH using electrocardiographic (ECG)-gated MDCT.
The study protocol was approved by the Research Ethics Committee of our hospital (201203004RIC). Lung transplantation candidates with the diagnosis of COPD and PH were included retrospectively. Between 2006 and 2012, a total of 15 patients received ECG-gated MDCT of the chest to evaluate the possibility of lung transplantation at our institution. These 15 patients met the international guidelines for the selection of lung transplant candidates (13). All patients had COPD as the cause of their primary disease. None of the patients had a history of coronary artery disease. All 15 patients had evidence of secondary pulmonary hypertension, based on the findings of conventional right heart catheterization (n = 7) with mean pulmonary arterial pressure of greater than 25 mm Hg and doppler echocardiography (n = 8) with an estimation of systolic pulmonary arterial pressure of greater than 50 mm Hg.
Whole lung CT without intravenous contrast was performed with a 64-section CT scanner (LightSpeed VCT; GE Healthcare, Milwaukee, WI, USA). All patients were imaged in the supine position while holding their breath at full inspiration. The following standard acquisition parameters were used: 120 mA, 120 kVp, 1.3 pitch, and 0.7-second rotation time. CT scans were reconstructed at section widths of 0.625 mm. ECG-gated CT angiography was performed afterward, with 90 mL of intravenous non-ionic contrast agent (Iopromide, Ultravist 300; Bayer Healthcare, Berlin, Germany) injected biphasically at 4-5 mL/sec (Stellant D injector; Medrad Inc., Warrendale, PA, USA); timing bolus was used to trigger CT acquisition. The average estimated radiation dose ranged from 6 to 16 mSv.
CT angiography has been proven to accurately quantify RV function (14). We measured left and right ventricular structures and functions by utilizing the techniques of multiphase reconstruction and cardiac segmentation from CT angiography, using a dedicated commercially available workstation (CT Comprehensive Cardiac Analysis IntelliSpace Portal, Philips Extended Brilliance™ Workspace V4.5.2.40007; Philips Healthcare, Eindhoven, the Netherlands). Endocardial contours were traced on the diastolic and systolic images. The ventricular volume (diastolic or systolic) equaled to the sum of all the endocardial areas (of the diastolic or systolic images, respectively) multiplied by the slice thickness. The CT imaging was reviewed by two radiologists who had more than 5 years of related cardiac CT experience, in order to establish a consensus. All axial, coronal, and sagittal slices were reviewed after being processed and adjusted manually for the precise segmented area of each cardiac structure (Fig. 1).
Computed tomography scans were reconstructed at section widths of 0.625 mm with standard filter algorithm (GE Healthcare, Milwaukee, WI, USA). Densitometric measures of emphysema of the whole lung were performed by using a dedicated commercially available workstation (CT lung density software program, IntelliSpace Portal, Philips Extended Brilliance™ Workspace V4.5.2.40007). The extent of emphysema, expressed as "percent emphysema", was defined as the percentage of voxels below -910 Hounsfield units in the lung on non-contrast CT scans using 1 mm collimation at full inspiration (Fig. 2). This threshold was chosen on the basis of quantitative histological comparison (15).
Statistical analysis was performed using the R 2.14.1 software (R Foundation for Statistical Computing, Vienna, Austria) and the Statistical Package for Social Sciences for Windows, version 17.0 (SPSS Inc., Chicago, IL, USA). Regarding statistical testing, a two-sided p value of ≤ 0.05 was considered to be statistically significant. A simple linear regression model was used to assess the association between percent emphysema derived from CT scan and each of the heart function indicators. The goal of regression analysis was to find one or a few parsimonious regression models that fit the observed data well for an effective estimation. To ensure the quality of analysis results, the basic model-fitting techniques for variable selection, goodness-of-fit (GOF) assessment, or regression diagnostics were used in our regression analyses. Specifically, a stepwise variable selection procedure (with iterations between the forward and backward steps) was applied to obtain the candidate's final linear regression model. The coefficient of determination (R2) was examined to assess the GOF of the linear regression model.
The demographic and clinical characteristics of the 15 patients are shown in Table 1. The median age of the study patients was 55 years (range, 30-75 years); 60% were men, and 80% were global initiative for chronic obstructive lung disease stage IV patients. The mean value for percent predicted forced vital capacity and percent predicted forced expiratory volume in one second was 44.8% (range, 24.5-65.1%) and 29.3% (range, 12.6-46.6%), respectively. The mean value for percent emphysema was 36.1% (range, 18.4-62.4%). Two patients eventually received lung transplantation surgery.
The image assessment is demonstrated in Figure 3 and 4. According to the protocol, whole lung CT without intravenous contrast demonstrated severe emphysema in the lung window (Fig. 3), and contrast-enhanced CT short-axis image in end-systole phase demonstrated RV dysfunction by straightening of interventricular septum to LV (Fig. 4).
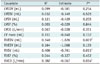
The ventricular function parameters of the 15 patients are shown in Table 2. The mean values for RV end-diastolic volume (RVEDV), RV end-systolic volume, and RV stroke volume (RVSV) were 144.9 mL (range, 85.7-261.7 mL), 87.7 mL (range, 47.2-211.7 mL), and 57.3 mL (range, 22.6-92.7 mL), respectively. The mean value for RV ejection fraction was 39.9% (range, 19.1-54.2%). The mean value for RV cardiac output (RVCO) was 5.07 L/min (range, 2.44-8.43 L/min).
The associations between percent emphysema and heart function indicators in the linear regression analysis are shown in Table 3. In COPD patients with PH, significant correlations were found between percent emphysema and three RV measures (Fig. 5). A 1% increase of percent emphysema would lead to a 1.8 mL decrement in the mean value of RVEDV (R2 = 0.340, p = 0.023), a 0.8 mL decrement in RVSV (R2 = 0.406, p = 0.011), and a 0.07 L decrement in RVCO (R2 = 0.382, p = 0.014); the correlations between percent emphysema and LV function indicators were not observed.
The current study is presently the first study that uses MDCT to evaluate the association between percent emphysema and parameters of the heart function. This study demonstrated the significant correlations between percent emphysema and RVEDV, RVSV, and RVCO in COPD patients with PH.
Catheterization of the right heart for functional assessment is invasive and increases the risk for patients. Measurement of the transverse/radial function by cardiac ultrasound does not directly reflect the major component of RV function (12). Compared to cardiac MRI, MDCT provide information on the extent of pulmonary emphysema and bilateral ventricular function simultaneously, indicating the advantages of time saving and insensitivity to movements in patients with critical illness. CT is more suitable for dyspneic patients who cannot tolerate breath hold in the time-consuming MR study. In this study, we used an ECG-gated MDCT protocol to evaluate both cardiac ventricular function and pulmonary parenchyma for lung transplantation candidates with PH. A greater extent of emphysematous change on CT scanning was linearly related to impaired RV diastolic function in COPD patients with PH. These results suggest that greater percent emphysema may lead to reduced filling of the right ventricle and reduced pulmonary blood flow.
Right heart has been known to be a lower pressure system. The pulmonary temponade effect compromises the right heart and systemic venous return more apparently than the left heart (16). It is reasonable to hypothesize that emphysema primarily impair RV diastolic function and indirectly affect the LV function via the decreased RV stroke volume. More potential confounder affecting the LV end-diastolic volume has been recognized, including compensation of the impaired LV diastolic function by the left atrium contraction. Hence, our results showed that percent emphysema had no relation between percent emphysema and LV function in patients with COPD and PH.
Barr et al. (9) demonstrated that percent emphysema was linearly related to impaired LV functions in patients with COPD. However, the study excluded patients with severe lung disease, clinical cardiovascular manifestations, or lung disease with restrictive patterns. In contrast, our study included lung transplant candidates who had more severe clinical conditions. Our results did not demonstrate any association between percent emphysema and LV diastolic function in COPD patients with PH, while percent emphysema was correlated with RVEDV, RVSV, and RVCO. Several possibilities might be relevant to the different results from our study, including small sample size and different study cohort in clinical manifestations of both pulmonary emphysema and PH in our patients. Therefore, a prospective study with larger cohort and different degrees of pulmonary emphysema and PH might be needed.
Right ventricular function was significantly decreased in patients with severe COPD than in mild or moderate COPD (8, 17). The correlation was observed between RV ejection fraction and pulmonary function tests including forced expiratory volume in one second and forced vital capacity (17). Moreover, population-based study showed that percent emphysema was inversely associated with RV parameters using cardiac MRI (10). Hyperinflation and gas trapping might impair right heart function by reducing venous return to the thorax, increasing end-diastolic stiffness of the right ventricle, or increasing pulmonary arteriovenous pressure gradients (4, 18). To summarize recent studies and our result, deteriorating RV function is correlated with percent emphysema or functional pulmonary parameters in COPD patients.
Except for the drawback of radiation exposure, CT is a convenient modality to evaluate the structures of lung, vasculature, and heart, as well as providing a non-invasive evaluation of cardiac function. Compared with echocardiography, CT has less inter-observer bias and is more objective and precise in evaluating the right heart function (19). The current state-of-the-art CT technology with the use of adaptive statistical iterative reconstruction further decreases the radiation exposure dose (20). Therefore, more reasonable CT radiation exposure can be expected in the near future.
Our study has several limitations. The sample size was relatively small. Our findings should be interpreted with caution given the possible uncertainty introduced by CT-measured heart and lung functions. CT-measured pulmonary or cardiac parameters were not correlated with pulmonary function tests, cardiac catheterization, or cardiac echocardiography. More detailed validation strategies are still required between CT-measured values and real-time clinical condition.
In conclusion, the present study revealed that CT-measured percent emphysema had a significant correlation with RVEDV, RVSV, and RVCO in COPD patients with PH. The pathophysiologic mechanism of emphysematous change to deteriorate cardiac function was complicated, but impaired RV function was an important contributor. Once COPD is observed as the primary etiology, CT-measured percent emphysema can be utilized as a convenient predictor for the severity of RV dysfunction, which might help to indicate prognosis of future right-sided heart failure and mortality.
Figures and Tables
Fig. 1
Snap shot of successful segmentation of each of cardiac chambers after semiautomatic processing and manual adjustment during different cardiac phases. Ventricular volume equals sum of all endocardial areas multiplied by slice thickness.

Fig. 2
Coronal reformatted lung window image in 57-year-old man with severe chronic obstructive pulmonary disease amenable to lung transplantation. Red areas indicate voxels below -910 Hounsfield units in lung parenchyma, which represent emphysematous change.
Fig. 3
Axial image of whole lung CT without intravenous contrast, in 60-year-old man with severe chronic obstructive pulmonary disease, demonstrates severe emphysema in lung window.

Fig. 4
Coronal short-axis image of contrast-enhanced CT in end-systole phase, in 67-year-old woman with severe chronic obstructive pulmonary disease, demonstrates straightening of interventricular septum (arrow) to left ventricle (LV) which indicates right ventricle (RV) dysfunction.

Fig. 5
Relationship of pulmonary percent emphysema and right ventricle parameters in chronic obstructive pulmonary disease patients with pulmonary hypertension.
A. Right ventricular end-diastolic volume (R2 = 0.340, p = 0.023). B. Right ventricular stroke volume (R2 = 0.406, p = 0.011). C. Right ventricular cardiac output (R2 = 0.382, p = 0.014).

Table 1
Pulmonary Function in Chronic Obstructive Pulmonary Disease Patients with Pulmonary Hypertension

Table 2
Ventricular Functions in Chronic Obstructive Pulmonary Disease Patients with Pulmonary Hypertension
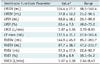
Table 3
Linear Regression Analysis of Associations between Percent Emphysema and Heart Function Indicators in Chronic Obstructive Pulmonary Disease Patients with Pulmonary Hypertension
References
1. MacNee W. Pathophysiology of cor pulmonale in chronic obstructive pulmonary disease. Part One. Am J Respir Crit Care Med. 1994; 150:833–852.
2. Barberà JA, Peinado VI, Santos S. Pulmonary hypertension in chronic obstructive pulmonary disease. Eur Respir J. 2003; 21:892–905.
3. Kasahara Y, Tuder RM, Cool CD, Lynch DA, Flores SC, Voelkel NF. Endothelial cell death and decreased expression of vascular endothelial growth factor and vascular endothelial growth factor receptor 2 in emphysema. Am J Respir Crit Care Med. 2001; 163(3 Pt 1):737–744.
4. Jörgensen K, Müller MF, Nel J, Upton RN, Houltz E, Ricksten SE. Reduced intrathoracic blood volume and left and right ventricular dimensions in patients with severe emphysema: an MRI study. Chest. 2007; 131:1050–1057.
5. Jörgensen K, Houltz E, Westfelt U, Nilsson F, Scherstén H, Ricksten SE. Effects of lung volume reduction surgery on left ventricular diastolic filling and dimensions in patients with severe emphysema. Chest. 2003; 124:1863–1870.
6. Shin KE, Chung MJ, Jung MP, Choe BK, Lee KS. Quantitative computed tomographic indexes in diffuse interstitial lung disease: correlation with physiologic tests and computed tomography visual scores. J Comput Assist Tomogr. 2011; 35:266–271.
7. Raman SV, Shah M, McCarthy B, Garcia A, Ferketich AK. Multi-detector row cardiac computed tomography accurately quantifies right and left ventricular size and function compared with cardiac magnetic resonance. Am Heart J. 2006; 151:736–744.
8. Gao Y, Du X, Liang L, Cao L, Yang Q, Li K. Evaluation of right ventricular function by 64-row CT in patients with chronic obstructive pulmonary disease and cor pulmonale. Eur J Radiol. 2012; 81:345–353.
9. Barr RG, Bluemke DA, Ahmed FS, Carr JJ, Enright PL, Hoffman EA, et al. Percent emphysema, airflow obstruction, and impaired left ventricular filling. N Engl J Med. 2010; 362:217–227.
10. Grau M, Barr RG, Lima JA, Hoffman EA, Bluemke DA, Carr JJ, et al. Percent emphysema and right ventricular structure and function: the Multi-Ethnic Study of Atherosclerosis-Lung and Multi-Ethnic Study of Atherosclerosis-Right Ventricle Studies. Chest. 2013; 144:136–144.
11. Sachdev A, Villarraga HR, Frantz RP, McGoon MD, Hsiao JF, Maalouf JF, et al. Right ventricular strain for prediction of survival in patients with pulmonary arterial hypertension. Chest. 2011; 139:1299–1309.
12. Fisher MR, Criner GJ, Fishman AP, Hassoun PM, Minai OA, Scharf SM, et al. Estimating pulmonary artery pressures by echocardiography in patients with emphysema. Eur Respir J. 2007; 30:914–921.
13. Orens JB, Estenne M, Arcasoy S, Conte JV, Corris P, Egan JJ, et al. International guidelines for the selection of lung transplant candidates: 2006 update--a consensus report from the Pulmonary Scientific Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2006; 25:745–755.
14. Remy-Jardin M, Delhaye D, Teisseire A, Hossein-Foucher C, Duhamel A, Remy J. MDCT of right ventricular function: impact of methodologic approach in estimation of right ventricular ejection fraction, part 2. AJR Am J Roentgenol. 2006; 187:1605–1609.
15. Coxson HO, Mayo JR, Behzad H, Moore BJ, Verburgt LM, Staples CA, et al. Measurement of lung expansion with computed tomography and comparison with quantitative histology. J Appl Physiol (1985). 1995; 79:1525–1530.
16. Boussuges A, Pinet C, Molenat F, Burnet H, Ambrosi P, Badier M, et al. Left atrial and ventricular filling in chronic obstructive pulmonary disease. An echocardiographic and Doppler study. Am J Respir Crit Care Med. 2000; 162(2 Pt 1):670–675.
17. Hur J, Kim TH, Kim SJ, Ryu YH, Kim HJ. Assessment of the right ventricular function and mass using cardiac multi-detector computed tomography in patients with chronic obstructive pulmonary disease. Korean J Radiol. 2007; 8:15–21.
18. Watz H, Waschki B, Meyer T, Kretschmar G, Kirsten A, Claussen M, et al. Decreasing cardiac chamber sizes and associated heart dysfunction in COPD: role of hyperinflation. Chest. 2010; 138:32–38.
19. Berger HJ, Matthay RA. Noninvasive radiographic assessment of cardiovascular function in acute and chronic respiratory failure. Am J Cardiol. 1981; 47:950–962.
20. Hara AK, Paden RG, Silva AC, Kujak JL, Lawder HJ, Pavlicek W. Iterative reconstruction technique for reducing body radiation dose at CT: feasibility study. AJR Am J Roentgenol. 2009; 193:764–771.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download