Abstract
Objective
We report magnetic resonance imaging (MRI) findings on focal anterior displacement of the thoracic spinal cord in asymptomatic patients without a spinal cord herniation or intradural mass.
Materials and Methods
We identified 12 patients (male:female = 6:6; mean age, 51.7; range, 15-83 years) between 2007 and 2011, with focal anterior displacement of the spinal cord and without evidence of an intradural mass or spinal cord herniation. Two radiologists retrospectively reviewed the MRI findings in consensus.
Results
An asymmetric spinal cord deformity with a focal dented appearance was seen on the posterior surface of the spinal cord in all patients, and it involved a length of 1 or 2 vertebral segments in the upper thoracic spine (thoracic vertebrae 1-6). Moreover, a focal widening of the posterior subarachnoid space was also observed in all cases. None of the patients had myelopathy symptoms, and they showed no focal T2-hyperintensity in the spinal cord with the exception of one patient. In addition, cerebrospinal fluid (CSF) flow artifacts were seen in the posterior subarachnoid space of the affected spinal cord level. Computed tomography myelography revealed preserved CSF flow in the two available patients.
Focal anterior displacement of the thoracic spinal cord on magnetic resonance imaging (MRI) is typically seen in patients with intradural arachnoid cysts or spinal cord herniation. Posterior intradural arachnoid cysts displace and compress the spinal cord by mass effect, whereas spinal cord herniation is a displacement of the spinal cord through a dural defect secondary to a traumatic, postoperative, or idiopathic etiology (1). Spinal cord herniation has been reported with increasing frequency in recent years, and it is an important differential diagnosis to consider with suspected intradural arachnoid cysts (2). Once a dural defect has occurred, cerebrospinal fluid (CSF) pulsation may push the cord through the defect, resulting in progressive myelopathy (3, 4).
We have collected rare cases of localized anterior displacement of the thoracic spinal cord without evidence of an intradural mass or spinal cord herniation on MRI. Most cases were found incidentally during lumbar spine MRI examinations, which routinely included whole spine T2 sagittal images as part of the scan protocol. No reports have described anterior displacement of the spinal cord without the above-mentioned conditions. Herein, we report spinal MRI findings in 12 patients who showed focal anterior displacement of the spinal cord without evidence of an intradural mass or spinal cord herniation.
We have had a special interest in cases of focal anterior displacement of the spinal cord without evidence of an intradural mass or spinal cord herniation since 2007 and have collected cases. Whole spine T2-weighted sagittal images are included in all spine MRI study protocols at our institution. In cases of focal anterior displacement of the spinal cord, additional T1- and T2-weighted sagittal and axial images were acquired at the same time. The inclusion criteria for this study were 1) localized anterior displacement of the spinal cord in the thoracic spine; 2) no evidence of an intradural mass, including cysts, adhesive bands, or spinal cord herniation; and 3) no history of trauma, surgery, or infection. One radiologist conducted a retrospective chart review, focusing on clinical history, symptoms at presentation, and follow-up assessment.
MRI studies were performed on a 1.5-T scanner (Gyroscan Intera; Philips, Best, the Netherlands), according to the standard protocol at our institution with modifications. T1- and T2-weighted images were obtained for both the sagittal and axial planes of the thoracic spine. The following scan parameters were used: 1) sagittal T1-weighted spin-echo (repetition time/echo time, 400/10 msec; section thickness, 4 mm; field of view, 556 × 349 mm), 2) sagittal T2-weighted spin-echo (3500/120; section thickness, 4 mm; field of view, 556 × 349 mm), 3) axial T1-weighted spin-echo (635/8; section thickness, 4 mm; field of view, 150 × 150 mm), and 4) axial T2-weighted spin-echo (3215/120; section thickness, 4 mm; field of view, 150 × 150 mm). Additional computed tomography (CT) myelography was performed in two patients in the supine and prone positions when physicians sought to exclude an intradural mass or dural defect in cases of diagnostic uncertainty.
Two radiologists analyzed the spinal MRI qualitatively in consensus in all cases, focusing on the level, pattern, segmental length of the spinal cord displacement, and cord signal change. The presence of a flow artifact was also evaluated at the affected spinal level. Four patients underwent a follow-up MRI study within 1-8 months of their first examination; in these patients, the initial and subsequent images were also assessed, focusing on interval changes.
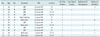
Twelve patients (male:female = 6:6) from 2007 to 2011 were included in this study. Mean age was 51.7 years (standard deviation ± 17.9 years, range 15-83 years). Table 1 summarizes the initial MRI findings for the 12 patients. The focal anterior displacement of the spinal cord was associated with a widening of the dorsal subarachnoid space and was located in the upper thoracic spine level (T1-T6) in all patients. Intriguingly, an asymmetric dented appearance deformity along the posterior surface of the spinal cord was noted, which involved a length of 1 or 2 vertebral segments in all patients (Fig. 1). In nine patients, the anterior spinal cord displacement was centered at the vertebral body level, while in the other three cases the anterior spinal cord displacement was at the intervertebral disc level without evidence of disc herniation. Axial T2-weighted images showed focal ventral displacement of the cord without focal spinal cord herniation and a relatively preserved anterior subarachnoid space. None of the patients showed cord signal changes at the level of cord displacement, with the exception of one patient with focal T2 signal hyperintensity. In all patients, prominent CSF flow artifacts were also seen in the posterior subarachnoid space at the involved level. However, additional CT myelography in two patients showed a dilated posterior CSF space without any dorsal intradural filling defect or blockade. Furthermore, there were no findings of spinal cord herniation (Fig. 2).
All patients were asymptomatic, and the anterior displacement of the spinal cord was an incidental finding on spine MRI. Follow-up MRI obtained in four patients at 1 and 8 months showed no interval change in the upper thoracic spinal cord deformity (Fig. 3). None of the patients showed symptoms of myelopathy during the follow-up period.
In this study, we report asymptomatic patients with focal anterior displacement of the spinal cord at the upper thoracic level without an intradural mass or cord herniation. In all cases, an asymmetric dented appearance deformity along the posterior surface of the spinal cord was noted. Such thoracic spinal cord indentations have not been previously reported.
We hypothesized that the focal anterior displacement of the thoracic spinal cord might result from a CSF pulsation pressure effect, as the asymmetric dented appearance deformity along the posterior surface of the spinal cord was situated in the upper thoracic level where the posterior subarachnoid CSF space is the widest. The thoracic spine has normal kyphosis, and the spinal cord is normally situated in the ventral aspect of the spinal canal at the upper to mid-thoracic spine, which could be a potential predisposition to such lesions. Another potential mechanism is that the negative pressure in the thoracic extradural space and the proximity of the heart may amplify the effects of CSF pulsation, resulting in these thoracic lesions. Furthermore, respiration and flexion and extension movements of the spine might be involved in the etiology of the thoracic lesions.
Reardon et al. (5) described the presence of an arachnoid web in the dorsal subarachnoid space that caused focal indentation of the upper thoracic spinal cord without an intradural mass or spinal cord herniation. They reported 14 patients who showed focal dorsal indentation in the upper thoracic spinal cord, and seven of the patients underwent surgery following their imaging studies. Five cases were surgically confirmed as arachnoid webs without evidence of an arachnoid cyst or ventral spinal cord herniation. T2 cord signal changes were demonstrated in 10 patients, and seven of these patients showed syringomyelia at the level of the cord indentation. However, no T2 signal change at the level of cord displacement was observed in our study, with the exception of one patient with a focal change. In addition, our patients with focal T2 signal changes showed no myelopathy symptoms, indicating that the possibility of an arachnoid web was low in our cases.
Focal anterior displacements of the spinal cord with enlargement of the dorsal subarachnoid space on MRI are characteristic findings of spinal cord herniation and intradural arachnoid cysts. Anterior spinal cord herniation is a rare disorder that does not have a clearly identified pathogenesis in most cases (6). Various mechanisms have been postulated to explain the initial dural defect and subsequent cord herniation (7). Most spinal cord herniations occur in the thoracic spine, predominantly at the third to seventh thoracic vertebra (T3-T7) levels (80% of all patients) (8, 9). Spinal cord herniation can be diagnosed using axial MRI or CT myelography by demonstrating anterior herniation of the spinal cord outside the margins of the dura. However, in our cases, no evidence of anterior herniation of the spinal cord was observed on axial MRI or axial CT myelography images.
According to Taylor et al. (10), thoracic anterior spinal cord adhesion syndrome (TASCAS) represents two pathologies and includes anterior cord adhesion and anterior cord herniation within a single spectrum, with cord herniation considered at one end of the spectrum. In their study, four cases showed no spinal cord herniation but did show anterior spinal cord adhesion. TASCAS with cord adhesion is conceptually different from our cases, in that Taylor et al. (10) postulated spinal cord adhesion as a predisposing factor in spinal cord herniation and regarded these within one spectrum. In their study, most of the cases showed a cord abnormality adjacent to the intervertebral disc or upper margin of the disc with associated degenerative disc abnormality. In contrast, our cases showed different MRI features: 1) most cases showed anterior cord displacement at the vertebral body level, not at the intervertebral disc level; and 2) no case showed evidence of cord adhesion to the anterior dura, a visible CSF cleft in the anterior arachnoid space, or herniation of the spinal cord on prone CT myelography (Fig. 2). All of our cases showed an asymmetric dented appearance deformity on the posterior surface of the spinal cord. We consider some cases of TASCAS to be within the spectrum of spinal cord herniation; however, some cases with features similar to TASCAS may be included within our suggested new entity.
Intradural arachnoid cysts are also considered in the differential diagnoses of our imaging findings. The most common location for an intradural arachnoid cyst is the dorsal subarachnoid space of the thoracic spine; symptomatic patients present with various symptoms, including motor weakness, numbness, and pain (11, 12, 13). Intradural arachnoid cysts can be diagnosed based on their typical MR findings. Posterior intradural cysts compress and displace the spinal cord anteriorly by the mass effect. As such, an intradural arachnoid cyst is expected to show wide, smooth symmetric spinal cord displacement rather than a dented appearance asymmetric deformity, as seen in our cases. The absence of the normal CSF pulsation artifact is an important clue in diagnosing intradural arachnoid cysts, as it implies CSF blockage by the cyst. In contrast, a preserved normal CSF pulsation artifact was noted in our series. In previous reports, additional CT or MR myelography was used to confirm the diagnosis (to demonstrate the absence of intervening CSF and a posterior subarachnoid lesion), as well as phase-contrast MRI (to demonstrate normal pulsatile CSF flow dorsally; thus, excluding a cyst) (4, 14). Additional CT myelography was performed in two of our cases, which revealed a dilated CSF space without a dorsal intradural filling defect or blockade, such as those caused by arachnoid cysts.
Despite the retrospective nature of the study and the rarity of this entity, we collected 12 consecutive patients. The mechanism of the previously unreported thoracic spinal cord indentation still needs to be clarified. Because we hypothesized that the lesions could have resulted from pressure effects of CSF flow pulsation, further study is warranted to describe the pathophysiology of this condition.
In conclusion, anterior displacement of the thoracic spinal cord can be found in the MRI of asymptomatic patients without serious spinal lesions. The characteristic MRI findings of an asymmetric dented appearance with anterior spinal cord displacement will be helpful for differential diagnoses of surgical diseases such as a spinal cord herniation or intradural mass.
Figures and Tables
 | Fig. 1Whole-spine sagittal T2-weighted images show incidental findings of focal anterior displacement of thoracic spinal cord in two patients.
A, B. Asymmetric dented appearance with ventral angulation of cord and widening of dorsal cerebrospinal fluid (CSF) space are present without intradural mass or spinal cord herniation in upper thoracic spine. Prominent CSF flow artifacts are present in posterior subarachnoid space at involved spine level. Arrow indicates spinal cord.
|
 | Fig. 2Cervical spine magnetic resonance imaging (A-D) and additional computed tomography (CT) myelography (E, F) of 38-year-old woman who presented with neck pain.
Sagittal T2-weighted image (A) and axial T2-weighted image (B) show anteriorly displaced spinal cord at T2/3 level with hypointense elongated flow artifact in extended dorsal space at same level. Sagittal (C) and axial (D) CT myelography in supine position show widening of posterior space without intradural filling defect or blockade (such as those caused by arachnoid cyst). Sagittal (E) and axial (F) CT myelography in prone position show preservation of anterior subarachnoid space and intact cerebrospinal fluid flow. There was no finding of spinal cord herniation or spinal cord adhesion. All axial images (B, D, F) were obtained at T2 level. Arrow indicates spinal cord.
|
 | Fig. 3Lumbosacral spine magnetic resonance imaging (MRI) of 48-year-old woman who presented with low back pain.
A. Sagittal T2-weighted image shows asymmetric dented appearance and anteriorly displaced spinal cord at T4 level. B, C. Follow-up cervical spine MRI study 4 months after first examination. Sagittal T2-weighted image (B) shows no interval change in cord deformity. Axial T2-weighted image (C) shows ventral displacement of cord without focal spinal cord herniation and relatively preserved anterior subarachnoid space at T4 level. Arrow indicates spinal cord.
|
Table 1
Focal Anterior Deviation of Spinal Cord with Widening of Dorsal Subarachnoid Space
References
1. Parmar H, Park P, Brahma B, Gandhi D. Imaging of idiopathic spinal cord herniation. Radiographics. 2008; 28:511–518.
2. Groen RJ, Coppes MH. Operative treatment of posterior spinal arachnoid cysts: do not refrain from checking on an anterior transdural spinal cord herniation. Acta Neurochir (Wien). 2011; 153:601–602. author reply 603.
3. van den Hauwe L, Van Goethem JW, Goedseels K, Merlevede K, Degryse H, Parizel PM. Thoracic spinal cord herniation and arachnoid cyst. JBR-BTR. 2006; 89:150–115.
4. Dix JE, Griffitt W, Yates C, Johnson B. Spontaneous thoracic spinal cord herniation through an anterior dural defect. AJNR Am J Neuroradiol. 1998; 19:1345–1348.
5. Reardon MA, Raghavan P, Carpenter-Bailey K, Mukherjee S, Smith JS, Matsumoto JA, et al. Dorsal thoracic arachnoid web and the "scalpel sign": a distinct clinical-radiologic entity. AJNR Am J Neuroradiol. 2013; 34:1104–1110.
6. Brus-Ramer M, Dillon WP. Idiopathic thoracic spinal cord herniation: retrospective analysis supporting a mechanism of diskogenic dural injury and subsequent tamponade. AJNR Am J Neuroradiol. 2012; 33:52–56.
7. Tekkök IH. Spontaneous spinal cord herniation: case report and review of the literature. Neurosurgery. 2000; 46:485–491. discussion 491-492.
8. Sasani M, Ozer AF, Vural M, Sarioglu AC. Idiopathic spinal cord herniation: case report and review of the literature. J Spinal Cord Med. 2009; 32:86–94.
9. Groen RJ, Middel B, Meilof JF, de Vos-van de Biezenbos JB, Enting RH, Coppes MH, et al. Operative treatment of anterior thoracic spinal cord herniation: three new cases and an individual patient data meta-analysis of 126 case reports. Neurosurgery. 2009; 64:3 Suppl. ons145–ons159. discussion ons159-ons160.
10. Taylor TR, Dineen R, White B, Jaspan T. The thoracic anterior spinal cord adhesion syndrome. Br J Radiol. 2012; 85:e123–e129.
11. Abou-Fakhr FS, Kanaan SV, Youness FM, Hourani MH, Haddad MC. Thoracic spinal intradural arachnoid cyst: report of two cases and review of literature. Eur Radiol. 2002; 12:877–882.
12. Kumar K, Malik S, Schulte PA. Symptomatic spinal arachnoid cysts: report of two cases with review of the literature. Spine (Phila Pa 1976). 2003; 28:E25–E29.
13. Wang MY, Levi AD, Green BA. Intradural spinal arachnoid cysts in adults. Surg Neurol. 2003; 60:49–55. discussion 55-56.
14. Najjar MW, Baeesa SS, Lingawi SS. Idiopathic spinal cord herniation: a new theory of pathogenesis. Surg Neurol. 2004; 62:161–170. discussion 170-171.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download