Abstract
Objective
To evaluate the feasibility of percutaneous access via the recanalized paraumbilical vein for varix embolization.
Materials and Methods
Between July 2008 and Jan 2014, percutaneous access via the recanalized paraumbilical vein for varix embolization was attempted in seven patients with variceal bleeding. Paraumbilical vein puncture was performed under ultrasonographic guidance, followed by introduction of a 5-Fr sheath. We retrospectively evaluated the technical feasibility, procedure-related complications, and clinical outcomes of each patient.
Results
Recanalized paraumbilical vein catheterization was performed successfully in all patients. Gastroesophageal varix embolization was performed in six patients, and umbilical varix embolization was performed in one patient. Embolic materials used are N-butyl cyanoacrylate (n = 6) and coil with N-butyl cyanoacrylate (n = 1). There were no procedure-related complications. One patient underwent repeated variceal embolization 6 hours after initial procedure via recanalized paraumbilical vein, due to rebleeding from gastric varix.
Variceal bleeding is one of major complications in patients with portal hypertension. Various interventional procedures such as transjugular intrahepatic portosystemic shunt (TIPS), balloon-occluded retrograde transvenous obliteration (BRTO), and percutaneous embolization can be applied, depending on the location of the varix and the vascular anatomy (1, 2, 3, 4). Percutaneous embolization of the varix can be used in patients who are not candidates for TIPS or BRTO. As for access route of percutaneous embolization, most interventional radiologists are familiar with the transhepatic approach (3, 4, 5), and the transsplenic approach is occasionally performed without severe complications (6, 7).
The paraumbilical vein is one of the portosystemic collaterals in patients with portal hypertension. The prevalence of recanalized paraumbilical veins has been reported to be as high as 26% (8, 9). The paraumbilical vein occasionally leads to a varix around the umbilicus, a so-called caput medusa. Otherwise, a recanalized paraumbilical vein seldom attracts radiologists' attention.
Percutaneous access to the portal venous system through the recanalized paraumbilical vein has been described in a few literature reports (10, 11, 12, 13, 14), but it has not been widely used because of its lack of evidence on safety. The retrospective study described here aimed to evaluate the feasibility of percutaneous access via the recanalized paraumbilical vein, in patients with portal hypertension.
The Institutional Review Board approved this retrospective study, and informed consent was waived. Between July 2008 and Jan 2014, 7 patients underwent variceal embolization via recanalized paraumbilical veins. The patients included 5 males and 2 females, with an age range of 11-64 years (mean age, 45 years). Among them, 6 patients had gastroesophageal varices, 1 patient had an umbilical varix, 5 patients had a history of endoscopic variceal ligation (EVL) of esophageal varices, 6 patients had ascites on CT scan, and 1 patient had hepatocellular carcinoma and tumor thrombosis within the main portal vein (Table 1).
Contrast enhanced CT scans was performed to reveal vascular anatomy and varices in all patients prior to variceal embolization. In patients with gastroesophageal varices, the paraumbilical vein near the umbilicus was punctured in the cranial direction with a 21-G needle (Micropuncture introducer set, Cook, Bloomington, IN, USA) using ultrasound guidance. A 5-Fr sheath was introduced over the guidewire into the recanalized paraumbilical vein. A 4-Fr or 5-Fr catheter was advanced via the paraumbilical vein and main portal vein, and angiography was performed to demonstrate gastroesophageal varices. A microcatheter (Microferret, Cook, or Progreat, Terumo, Tokyo, Japan) was advanced into the left gastric vein, and varices were embolized by coil (Micronester, Cook) and/or a mixture of N-butyl cyanoacrylate (NBCA, Histoacryl; B. Braun, Melsungen, Germany) and iodized oil (Lipiodol; Andre Guerbet, Aulnay-Sous-Bois, France). In the patient with an umbilical varix, the paraumbilical vein 10 cm above the umbilicus was punctured in the caudal direction using ultrasound guidance. The umbilical varix was embolized using a mixture of NBCA and iodized oil.
We retrospectively evaluated the technical feasibility, procedure-related complications, and clinical outcomes of each patient. We defined technical success as a successful portal vein catheterization via recanalized paraumbilical vein, embolization of varices, and achievement of hemostasis of percutaneous access route. We defined clinical success as clinical improvement without evidence of bleeding for the next three days.
Using ultrasonography guidance, percutaneous access via the paraumbilical vein was performed successfully in all patients. Gastroesophageal variceal embolization was performed in six patients (Figs. 1, 2), and umbilical variceal embolization (Fig. 3) was performed in one patient. Embolic materials used for variceal embolization are NBCA (n = 6) and coil with NBCA (n = 1).
In three patients, the paraumbilical vein was embolized using a coil or a mixture of NBCA and iodized oil. In four patients, the puncture tract between the skin and the paraumbilical vein was embolized using a mixture of NBCA and iodized oil. In three patients (patients 5, 6, and 7), light manual compression for 5 minutes was applied to achieve hemostasis (Table 2).
There were no procedure-related complications such as bleeding from the paraumbilical vein. In one patient (patient 5), because rebleeding from the gastroesophageal varix was highly suspected by the clinician, the paraumbilical vein was punctured again 6 hours after the initial procedure. Splenic venography demonstrated a residual gastric varix, which was embolized using a mixture of NBCA and iodized oil.
Technical success was achieved in all 7 patients (100%). During the follow-up period (mean, 103 days; range: 2-340 days), 5 patients (71%) showed clinical success. Two patients (patients 3 and 5) died 2 days after the procedures, due to disseminated intravascular coagulopathy and massive gastrointestinal bleeding, respectively. Four patients underwent follow-up CT scans 25-41 days after the procedure. CT scan was undertaken for liver transplantation work-up (patients 1 and 2), evaluation of hepatocellular carcinoma (patient 4), and evaluation of retroperitoneal bleeding (patient 6). Gastric varices were obliterated on follow-up CT scans in these four patients. The remaining one patient (patient 7) did not undergo follow-up CT scans. Two patients (patients 1 and 7) underwent prophylactic EVL of esophageal varices during follow-up. Five patients with clinical success did not suffer from variceal bleeding during follow-up, but three patients died due to sepsis, hepatocellular carcinoma progression, and intracranial and retroperitoneal bleeding during follow-up (Table 1).
Several access techniques are available for catheterization in the portal venous system. First, the percutaneous transhepatic approach is the most popular approach and has been used for portal vein embolization and portal vein stenting, as well as variceal embolization (3, 4, 5, 15, 16). This approach can be difficult in patients with main portal vein occlusion or a large amount of ascites. Second, a transjugular intrahepatic portosystemic shunt is another well-known method for accessing the portal venous system (2). The creation of this access may take a longer time than other methods, and the relatively long route to the portal vein may cause difficulty in manipulating vascular catheters. Third, direct catheterization of a mesenteric vein aided by minilaparotomy is more invasive than the percutaneous technique (17). Fourth, transsplenic access can provide a straight pathway into the portal vein. However, bleeding complications have been reported in up to 13% of the procedures (7). Fifth, the recanalized paraumbilical vein can also provide vascular access to the portal venous system. Paraumbilical vein cannulation after skin incision for esophageal varix embolization was reported more than three decades ago (10, 11). In addition, complete chemoembolization of hepatocellular carcinoma fed by the portal vein via a percutaneous transumbilical approach has also been reported (14). This study showed that percutaneous access via the recanalized paraumbilical vein is feasible for variceal embolization. Although a patent paraumbilical vein is not observed in all patients, if present, it can be used as an easy access to the portal vein system.
In patients presenting with gastrointestinal bleeding, endoscopy has been considered as the first diagnostic and therapeutic treatment option. In this study, six patients with gastroesophageal varix underwent endoscopy prior to interventional management, and gastric varix as well as esophageal varix was confirmed. The endoscopists in our institute are reluctant to treat gastric varix, so these patients were referred to angiography suite for the treatment of gastric varix. Since percutaneous embolization of varix has higher recurrent variceal bleeding (18), TIPS or BRTO was preferred by the interventional radiologists. In this study, however, six patients with gastroesophageal varix had decompensated liver cirrhosis (i.e., Child-Pugh class C). Child-Pugh class C disease is a contraindication of TIPS because of the high mortality rate. Also, BRTO was not a practicable option because gastrorenal shunt was absent in these patients. Thus, percutaneous embolization of varix was planned to be used to treat varices in these patients. However, five patients had ascites on CT scan and two patients had hypoplastic portal vein or tumor thrombus in the portal vein. These findings could result in bleeding complication or difficulty in access to varix, if transhepatic approach or transsplenic approach had been adopted. Fortunately, because the recanalized paraumbilical vein was present in these patients, variceal embolization was performed through the paraumbilical vein without bleeding complication. When endoscopic management, TIPS, and BRTO are not applicable or relatively contraindicated in patients with gastroesophageal varix, percutaneous variceal embolization may be the last treatment option. When the paraumbilical vein is present, percutaneous access via the paraumbilical vein can be chosen prior to transhepatic or transplenic approach.
Patients with liver cirrhosis have bleeding tendencies including increased prothrombin time and thrombocytopenia. Therefore, to prevent hemorrhage from the puncture tract in the transhepatic or transsplenic approach, embolization or plugging of the puncture tract is mandatory; coils, gelatin sponge particles, and NBCA have been used in the literature (4, 5, 6, 7). In the earlier study period, we embolized the paraumbilical vein using coils or NBCA, under the presumption that intraperitoneal hemorrhages might develop after sheath removal. In the later study period, we speculated that intraperitoneal hemorrhages would not occur after sheath removal, because the paraumbilical vein is located in the extraperitoneal space, provided that the anterior wall of the paraumbilical vein was punctured. Thus, gentle manual compression was applied to achieve hemostasis at the puncture site, which resulted in successful hemostasis. In patient 5, manual compression was applied for hemostasis and the repeated access via the paraumbilical vein was possible for embolization of a residual varix.
In the early 1980', Sparks et al. (10) and Spigos et al. (11) reported of successful umbilical venous cannulation after skin incision in three and seven patients, respectively. Ibukuro et al. (12) identified the paraumbilical vein under the linea alba after making a small midline incision, and then punctured the paraumbilical vein. Whereas cannulation of the paraumbilical vein was made after skin incision in these previous reports (10, 11, 12), recent articles described percutaneous catheterization of the paraumbilical vein under ultrasound guidance (13, 14). In this study, percutaneous catheterization of the paraumbilical vein was performed without skin incision in all patients. Kim et al. (14) reported that the paraumbilical vein was embolized by coils to achieve hemostasis of puncture tract. In this study, gentle manual compression was enough to control hemostasis of puncture tract, which allowed repeated access to the portal venous system.
This study has some limitations. First, the study population was too small. Further study with a larger population is needed to confirm the safety of percutaneous access via the paraumbilical vein. Second, the study lacked a comparison with other access methods such as the transsplenic and transhepatic approaches. However, the paraumbilical vein is superficially located in the abdominal wall, and we believe that access via the paraumbilical vein is much easier for inexperienced operators.
In conclusion, percutaneous access via the paraumbilical vein for varix embolization is a simple alternative for patients with portal hypertension.
Figures and Tables
Fig. 1
52-year-old man presented with melena.
A. Transverse CT scan shows tumor thrombus in right portal vein (black arrowhead), gastric varix (white arrowhead), and recanalized paraumbilical vein (arrow). B. Maximum intensity projection image of left anterior oblique view shows gastroesophageal varix (arrowhead) and recanalized paraumbilical vein (arrow). C. Splenic venography shows gastroesophageal varix (white arrowhead) and filling defect caused by tumor thrombus (black arrowhead). Note that catheter was advanced via paraumbilical vein (arrow). D. Splenic venography after variceal embolization shows subtraction artifact (arrowhead) caused by embolic materials (coils and mixture of N-butyl cyanoacrylate and iodized oil) in gastric varix.
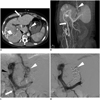
Fig. 2
49-year-old man presented with melena.
A. Transverse CT scan shows extravasation of contrast media (arrow) and blood clot (star) within stomach. B. Transverse CT scan shows recanalized paraumbilical vein (arrowhead). C. Left gastric venography shows gastroesophageal varix (arrowhead). D. Splenic venography after variceal embolization shows subtraction artifact (arrowhead) caused by embolic materials (mixture of N-butyl cyanoacrylate and iodized oil).
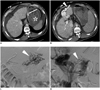
Fig. 3
11-year-old boy presented with umbilical varix bleeding.
A. Volume-rendering image of CT scan shows recanalized paraumbilical vein (arrowhead), umbilical varix (arrow), and draining systemic veins (open arrowheads). B. Spot image after embolization shows embolic materials within umbilical varix (arrow) and 5-Fr sheath (arrowhead) which was inserted in paraumbilical vein.
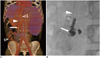
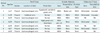
Table 1
Summary of Clinical Findings
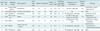
Note.- *Packed RBCs which were transfused between 24 hours before procedure and 24 hours after procedure were counted. DIC = disseminated intravascular coagulopathy, EVL = endoscopic varix ligation, GI = gastrointestinal, HBV = hepatitis B virus, HCC = hepatocellular carcinoma, HCV = hepatitis C virus, INR = international normalized ratio, LC = liver cirrhosis, PT = prothrombin time, RBC = red blood cell, TPL = transplantation
References
1. Yamagami T, Yoshimatsu R, Miura H, Matsumoto T, Hasebe T. The role of divided injections of a sclerotic agent over two days in balloon-occluded retrograde transvenous obliteration for large gastric varices. Korean J Radiol. 2013; 14:439–445.
2. Gaba RC, Omene BO, Podczerwinski ES, Knuttinen MG, Cotler SJ, Kallwitz ER, et al. TIPS for treatment of variceal hemorrhage: clinical outcomes in 128 patients at a single institution over a 12-year period. J Vasc Interv Radiol. 2012; 23:227–235.
3. Kwak HS, Han YM. Percutaneous transportal sclerotherapy with N-butyl-2-cyanoacrylate for gastric varices: technique and clinical efficacy. Korean J Radiol. 2008; 9:526–533.
4. Lim DH, Kim DH, Kim MS, Kim CS. Balloon-occluded percutaneous transhepatic obliteration of isolated vesical varices causing gross hematuria. Korean J Radiol. 2013; 14:94–96.
5. Tian X, Wang Q, Zhang C, Liu F, Cui Y, Liu F, et al. Modified percutaneous transhepatic variceal embolization with 2-octylcyanoacrylate for bleeding gastric varices: long-term follow-up outcomes. AJR Am J Roentgenol. 2011; 197:502–509.
6. Chu HH, Kim HC, Jae HJ, Yi NJ, Lee KW, Suh KS, et al. Percutaneous transsplenic access to the portal vein for management of vascular complication in patients with chronic liver disease. Cardiovasc Intervent Radiol. 2012; 35:1388–1395.
7. Zhu K, Meng X, Zhou B, Qian J, Huang W, Deng M, et al. Percutaneous transsplenic portal vein catheterization: technical procedures, safety, and clinical applications. J Vasc Interv Radiol. 2013; 24:518–527.
8. Lafortune M, Constantin A, Breton G, Légaré AG, Lavoie P. The recanalized umbilical vein in portal hypertension: a myth. AJR Am J Roentgenol. 1985; 144:549–553.
9. Aagaard J, Jensen LI, Sørensen TI, Christensen U, Burcharth F. Recanalized umbilical vein in portal hypertension. AJR Am J Roentgenol. 1982; 139:1107–1110.
10. Sparks FC, Maitem A, Glickman MG, Tilson MD. Embolization of bleeding esophageal varices via umbilical vein. An alternative approach. Arch Surg. 1982; 117:354–358.
11. Spigos DG, Tauber JW, Tan WS, Mulligan BD, Espinoza GA. Work in progress: umbilical venous cannulation: a new approach for embolization of esophageal varices. Radiology. 1983; 146:53–56.
12. Ibukuro K, Kojima K, Kigawa I, Tanaka R, Fukuda H, Abe S, et al. Embolization of rectal varices via a paraumbilical vein with an abdominal wall approach in a patient with massive ascites. J Vasc Interv Radiol. 2009; 20:1259–1261.
13. Lim LG, Lee YM, Tan L, Chang S, Lim SG. Percutaneous paraumbilical embolization as an unconventional and successful treatment for bleeding jejunal varices. World J Gastroenterol. 2009; 15:3823–3826.
14. Kim SC, Kim HC, Chung JW, Jae HJ, Park JH. Percutaneous transumbilical portal vein embolization in a patient with a ruptured hepatocellular carcinoma supplied by the portal vein. Cardiovasc Intervent Radiol. 2011; 34:Suppl 2. S214–S217.
15. Lee YJ, Shin BS, Lee IH, Ohm JY, Lee BS, Ahn M, et al. Intrahepatic portosystemic venous shunt: successful embolization using the Amplatzer Vascular Plug II. Korean J Radiol. 2012; 13:827–831.
16. Park KB, Choo SW, Do YS, Shin SW, Cho SG, Choo IW. Percutaneous angioplasty of portal vein stenosis that complicates liver transplantation: the mid-term therapeutic results. Korean J Radiol. 2005; 6:161–166.
17. Durham JD, Kumpe DA, Van Stiegmann G, Goff JS, Subber SW, Rothbarth LJ. Direct catheterization of the mesenteric vein: combined surgical and radiologic approach to the treatment of variceal hemorrhage. Radiology. 1990; 177:229–233.
18. Terabayashi H, Ohnishi K, Tsunoda T, Nakata H, Saito M, Tanaka H, et al. Prospective controlled trial of elective endoscopic sclerotherapy in comparison with percutaneous transhepatic obliteration of esophageal varices in patients with nonalcoholic cirrhosis. Gastroenterology. 1987; 93:1205–1209.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download