We commend Kulkarni et al. (1) on their description of a rare case of aberrant splenic artery aneurysm treated with a combination of stent graft and coil embolization. Indeed, aneurysm of splenic artery is a protean disease as for the origin, location, size and clinical manifestations. Furthermore, what appears to be initially a splenic aneurysm can exceptionally turn out to be another vascular lesion as happened to us.
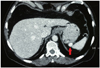
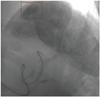
In fact, a 74-year-old man with a history of prostate cancer was recently diagnosed as having an aneurysm of 1.7 × 2 cm arising from a short gastric artery on a surveillance CT scan (Fig. 1). Superselective arteriography confirmed the aneurysmatic nature of the lesion (Fig. 2): transcatheter angiographic embolization was attempted twice but failed. At this point, the patient was referred for surgical repair: at laparoscopy, a brown, well-encapsulated, hypervascular lesion was observed in the greater omentum on the left side of the stomach and excised after ligation of its feeding pedicle. Histological and immunochemical features revealed benign hemangiopericytoma of the greater omentum (no mitosis or necrosis along with an immunoprofile positive for CD34 and bcl-2). At 14-month follow-up, the patient appears free from recurrent disease.
Hemangiopericytoma (HPC), also known as solitary fibrous tumor, is a rare form of vascular tumor arising from the pericytes of Zimmermann and may develop virtually anywhere in the whole body (2). Involvement of the greater omentum is outstandingly rare as only 30 cases have been reported in the world literature so far: tumor size ranges from 2 cm (as in our patient) to 28 cm and a malignant behavior was ascertained in 10 patients (3). Diagnosis prior to surgery appears impossible given that clinical and radiological findings are aspecific and biopsy is contraindicated for the risk of related bleeding (4). In fact, it is obtained, most of the time, in the course of emergency intervention performed for acute abdominal pain or hemoperitoneum; rarely, a solid, well-encapsulated hypervascular mass with a feeder vascular pedicle and centripetal opacification is seen early in the arterial phase on CT scan and it is more suggestive of stromal tumors or arteriovenous malformations (3, 4). Selective arteriography has been employed in only one previous case of omental HPC, while preoperative embolization, even if advocated, has never been described (3). Our case represents the first instance of omental HPC resembling aneurysm on CT scan and arteriography being initially managed with attempted angiographic embolizations. Surgical excision is the sole curative treatment for omental HPC; laparotomic resection is the most frequently performed intervention, while laparoscopic removal has been conducted only in three cases including ours (3, 4).
Figures and Tables
References
1. Kulkarni CB, Moorthy S, Pullara SK, Kannan RR. Endovascular treatment of aneurysm of splenic artery arising from splenomesentric trunk using stent graft. Korean J Radiol. 2013; 14:931–934.
2. Goldberger RE, Schein CJ. Hemangiopericytoma of the omentum. Report of a case with a unique presentation and review of the literature. Am Surg. 1968; 34:291–229.
3. Morris-Stiff G, Falk GA, Joyce D, Rubin B, Chalikonda S. Primary omental haemangiopericytoma. BMJ Case Rep. 2011; doi: 10.1136/bcr.03.2011.4041.
4. Crusco F, Chiodi M, Pugliese F, Mosca S, Fischer MJ, Lupattelli L. Benign omental hemangiopericytoma presenting with hemoperitoneum: radiologic findings. AJR Am J Roentgenol. 2005; 184:3 Suppl. S67–S69.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download