Abstract
Happle-Tinschert syndrome is a disorder causing unilateral segmentally arranged basaloid follicular hamartomas of the skin associated with ipsilateral osseous, dental and cerebral abnormalities including tumors. Although a case with hemimegalencephaly was previously described, this is the first report of Happle-Tinschert syndrome with discrepant short left leg, ipsilateral skin lesions, hemimegalencephaly and frontal polymicrogyria.
In 2008, Happle and Tinschert (1) described a case with unilateral segmentally arranged basaloid follicular hamartomas of the skin associated with extracutaneous manifestations such as short leg, polydactyly and hypoplastic teeth. The authors also reviewed the literature and found eight similar cases under various definitions with additional findings of the bones, teeth and brain. They stated this disease as a distinct syndrome which has been confused with Gorlin syndrome in the past. Shortly after this article, Itin (2) reported a new case with similar features. He described the disease as 'segmentally arranged basaloid follicular hamartomas, linear atrophoderma with hypo- and hyperpigmentation, enamel defects, ipsilateral hypertrichosis, and skeletal and cerebral anomalies' and proposed the name 'Happle-Tinschert syndrome'. Recently, a patient with microphtalmia and hemimegalencephaly was presented by Boccaletti et al. (3) as the 11th case, all of which were reported in the dermatology literature.
Herein we present a case of Happle-Tinschert syndrome with hemimegalencephaly and discuss this neurocutaneous disorder with particular emphasis on imaging findings. This is the first report of Happle-Tinschert syndrome in the radiology literature and the first case with abnormal gyral pattern.
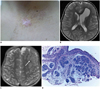
A 9-year-old boy presented with a discrepant short left leg and ipsilateral skin lesions to our institution. His family history was unremarkable. The skin lesions were present since his age of 3 years. The dermatological examination revealed multiple whitish papules on the left lower and the upper eyelids. Skin-coloured or brownish papules were present segmentally located on the left side of the presternal area and on the left shoulder with a localized hypertrichosis (Fig. 1A). Similar papular lesions were also detected over the left thigh in a systematized pattern following the lines of Blaschko. An epidermal nevus syndrome was suspected based on the unilateral manifestations of the clinical findings. The orthoroentgenogram revealed a discrepant shortening by 14 mm of the left lower extremity. A cerebral magnetic resonance imaging (MRI) was performed to investigate a possible neurocutaneous syndrome although the subject had no neurological symptoms such as epilepsia or mental retardation.
This MRI demonstrated a mild enlargement of the left hemisphere with minimal displacement of the midline and moderate enlargement of the ipsilateral ventricle especially in the frontal horn (Fig. 1B). The frontal horn of the left lateral ventricle was anteriorly and superiorly extending. An abnormal gyral pattern with slightly flat and thick cortex consistent with coarse polymicrogyria was also present in the left frontal lobe (Fig. 1C). No signal abnormality was detected in the white matter. Bilateral small temporal arachnoid cysts were observed. Extraparenchymal abnormalities such as olfactory nerve enlargement or abnormal dilated venous channels were not seen. No asymmetric enlargement was noted in the cerebellum or in the brainstem. The cerebellar folia were normal.
The histopathological examination of a papule on the left presternal area showed features consistent with a basaloid follicular hamartoma (Fig. 1D). Finally, Happle-Tinschert syndrome was diagnosis based on clinical, histopathological and imaging findings.
Happle-Tinschert syndrome is a recently defined multisystem disease characterized by unilateral cutaneous and extracutaneous manifestations including skeletal, dental and cerebral anomalies (1). The main cutaneous finding of this disease is the presence of unilateral segmentally arranged basaloid follicular hamartomas. Associated abnormalities reported so far in Happle-Tinschert syndrome are skeletal findings (disproportionate overgrowth or deficient growth of limb bones, scoliosis, widening of ribs, rudimentary ribs, polidactyly, syndactyly, malformed thumb, socket-type or saddle nose, frontal bossing, abnormal bone mineralization, ipsilateral premature closure of epiphyses), dental pathologies (anodontia, hypodontia, enamel defects), cerebral anomalies (mental retardation, unsteady gait, enlarged ventricle, ipsilateral hemiplegia, mild hemimegalencephaly) and other disorders such as microphtalmia, coloboma of optic nerve, cataract or an imperforate anus (1, 2, 3). In addition, ipsilateral tumors appear to have an increased incidence; medulloblastoma, optic glioma, menengioma, ameloblastoma of the mandible and colonic adenocarcinoma have been reported in patients with Happle-Tinschert syndrome (1, 2, 3).
Hemimegalencephaly is a congenital malformation of the brain causing hamartomatous overgrowth of the involved cerebral hemisphere. It may be classified as isolated or syndromic. Associated findings such as cutaneous abnormalities, hemihypertrophy and systemic involvement seen in neurocutaneous syndromes are present in a syndromic hemimegalencephaly. No clinical or imaging differences have been found between isolated and syndromic types (4). There are three grades of severity of hemimegalencephaly (4). Features of grade 1 were as follows: mild enlargement of the affected hemisphere, slight ventricular asymmetry with straightening of the frontal horn, abnormal signal changes in the white matter, straight midline or minimal displacement of midline and the absence of cortical dysplasia. In grade 2 are seen following features: moderate hemispheric enlargement, slight or moderate displacement of midline, moderate dilation or reduction of the lateral ventricle size, colpocephaly and focal cortical dysplasia. And grade 3 hemimegalencephaly is indicated by following features: abnormalities including severe hemispheric enlargement with marked dilation of the lateral ventricle, colpocephaly and extensive cortical dysplasia. However, despite this schema, the classification of hemimegalencephaly may be problematic due to overlapping of different grades (4). Before our case, Boccaletti et al. (3) reported a case with a mild (grade 1) form of hemimegalencephaly. No apparent cortical anomaly was detected in their patient. However, in our patient were the neuroimaging findings evaluated as grade 2 hemimegalencephaly due to the presence of a moderate dilation of the lateral ventricle and abnormal gyral pattern. The morphological appearance of the cortex was consistent with the coarse polymicrogyria described by Barkovich (5). The hemimegalencephaly associated with clinical findings suggested a neurocutaneous syndrome in these two patients who were finally diagnosed with the Happle-Tinschert syndrome.
Happle-Tinschert syndrome has been misdiagnosed as Gorlin syndrome (nevoid basal cell carcinoma syndrome) in the past (1). The presence of multiple basal cell carcinomas is one of the major diagnostic criteria in Gorlin syndrome. The term 'basal cell nevus' has been used as a synonym for 'nevoid basal cell carcinoma' in the past and the misdiagnosis of Gorlin syndrome was caused by this confusion (1). The main differential point from Gorlin syndrome is the segmental distribution of basaloid follicular hamartomas in Happle-Tinschert syndrome. Therefore, it is critical to histopathologically distinguish the basaloid follicular hamartoma from the basal cell carcinoma for the correct diagnosis. Also the imaging findings are different in these distinct syndromes. Keratocystic odontogenic tumors and dural calcifications are the most common manifestations of Gorlin syndrome; however, those findings have not been established in Happle-Tinschert syndrome so far (6). On the other hand, the herein described hemimegalencephaly is an unknown feature of Gorlin syndrome. Although a case with medulloblastoma was presented in a patient with Happle-Tinschert syndrome (2), an increased incidence of medulloblastoma is actually a feature of Gorlin syndrome. These tumors usually occur within the first 2 years of life in Gorlin syndrome (6). However, the patient with Happle-Tinschert syndrome developed a medulloblastom at the age of 5 years similar to those seen in the general population.
Happle-Tinschert syndrome has also been evaluated as a variant of epidermal nevus syndrome in the literature (7). An epidermal nevus syndrome is a neurocutaneous overgrowth disorder characterized by an epidermal nevus in association with central nervous system, eye or skeletal abnormalities (6). The term 'epidermal nevus syndrome' includes several different syndromes, which all have different histological types of epidermal nevus. There may be some clinical overlapping between Happle-Tinschert syndrome and epidermal nevus syndrome. However, a histopathological diagnosis (basaloid follicular hamartoma versus epidermal nevus) of the cutaneous lesion enables a proper diagnosis of the disease. A hemimegalencephaly with or without cortical anomaly is the most striking imaging feature of an epidermal nevus syndrome (6). Other neuroimaging findings of epidermal nevus syndrome including isolated gyral malformations, gliomatosis, hemiatrophy, vascular malformations, intracranial lipomas, porencephaly and infarctions have not been reported in Happle-Tinschert syndrome yet (6). However, a detailed evaluation of clinical and histopathological findings may be required in patients with hemimegalencephaly to reach a definitive diagnosis.
In conclusion, Happle-Tinschert syndrome is a recently defined disorder affecting bones, teeth and brain. This multisystem disease should be taken into consideration in the differential diagnosis of neurocutaneous syndromes. Hemimegalencephaly may be a part of this syndrome and neuroimaging should be done in suspected cases to investigate cerebral findings including hemimegalencephaly.
Figures and Tables
Fig. 1
Hemimegalencephaly with polymicrogyria in 9-year-old boy with Happle-Tinschert syndrome.
A. Segmentally arranged skin-coloured or brownish papules on left side of presternal area with localized hypertrichosis. B. Axial T2-weighted image shows mildly enlarged left hemisphere with moderate dilation of ipsilateral ventricle. C. Axial T2-weighted image shows polymicrogyria (arrow) in left frontal lobe. D. Anastomosing strands of basaloid cells with peripheral palisading in papillary dermis (hematoxylin and eosin, × 20).
Acknowledgments
The authors wish to acknowledge Dr. Mehmet Gamsızkan and Dr. Duygu Düşmez Apa for their contributions to the diagnostic assessment.
References
1. Happle R, Tinschert S. Segmentally arranged basaloid follicular hamartomas with osseous, dental and cerebral anomalies: a distinct syndrome. Acta Derm Venereol. 2008; 88:382–387.
2. Itin PH. Happle-Tinschert syndrome. Segmentally arranged basaloid follicular hamartomas, linear atrophoderma with hypo- and hyperpigmentation, enamel defects, ipsilateral hypertrichosis, and skeletal and cerebral anomalies. Dermatology. 2009; 218:221–222.
3. Boccaletti V, Accorsi P, Pinelli L, Ungari M, Giordano L, Neri I, et al. Congenital systematized basaloid follicular hamartoma with microphthalmia and hemimegalencephaly. Pediatr Dermatol. 2011; 28:555–560.
4. Flores-Sarnat L. Hemimegalencephaly: part 1. Genetic, clinical, and imaging aspects. J Child Neurol. 2002; 17:373–384. discussion 384.
5. Barkovich AJ. MRI analysis of sulcation morphology in polymicrogyria. Epilepsia. 2010; 51:Suppl 1. 17–22.
6. Vezina G, Barkovich AJ. The phakomatoses. In : Barkovich AJ, Raybaud C, editors. Pediatric neuroimaging. 5th ed. Philadelphia: Lippincott Williams & Wilkins;2012. p. 619–625.
7. Burck U, Held KR. Unilateral skin lesions, cataracts, optic glioma and retardation--a variant of the epidermal nevus syndrome? Dermatologica. 1982; 165:208–214.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download