Abstract
Objective
To investigate the interobserver reproducibility and diagnostic feasibility of a visual grading system for assessing atrophy of the supraspinatus muscle on magnetic resonance imaging (MRI).
Materials and Methods
Three independent radiologists retrospectively evaluated the occupying ratio of the supraspinatus muscle in the supraspinatus fossa on 192 shoulder MRI examinations in 188 patients using a 3-point visual grading system (1, ≥ 60%; 2, 30-59%; 3, < 30%) on oblique sagittal T1-weighted images. The inter-reader agreement and the agreement with the reference standard (3-point grades according to absolute occupying ratio values quantitatively measured by directly contouring the muscles on MRI) were analyzed using weighted kappa. The visual grading was applied by a single reader to a group of 100 consecutive patients who had undergone rotator cuff repair to retrospectively determine the association between the visual grades at preoperative state and postsurgical occurrences of retear.
Results
The inter-reader weighted kappa value for the visual grading was 0.74 when averaged across three reader pairs (0.70-0.77 for individual reader pairs). The weighted kappa value between the visual grading and the reference standard ranged from 0.75 to 0.83. There was a significant difference in retear rates of the rotator cuff between the 3 visual grades of supraspinatus muscle atrophy on MRI in univariable analysis (p < 0.001), but not in multivariable analysis (p = 0.026).
Rotator cuff tears, which are among the most common injuries of the shoulder (1, 2), induce muscle atrophy and fatty degeneration of the muscle. These two muscle abnormalities are different: fatty degeneration means intramuscular fatty accumulation, whereas muscle atrophy means a decrease in the volume of the muscle belly (3, 4, 5, 6). These structural changes are important negative prognostic factors influencing the result after repair (7, 8, 9, 10, 11, 12, 13). An evaluation of the quality of rotator cuff muscles is crucial for appropriate decision making and predicting the prognosis.
The classification of fatty degeneration established by Goutallier et al. has been widely used and validated for its reliability (4, 8, 10, 11). However, there are a few grading systems for supraspinatus muscle atrophy. Though some previous studies have introduced a classification for muscle atrophy, their use is somewhat limited. The tangent sign is frequently used due to its intuitive and quick qualitative assessment (5); however, it only considers the upper part of the supraspinatus muscle, regardless of the volume of the lower part. Another quantitative magnetic resonance imaging (MRI) assessment of muscle atrophy, which calculates the occupation ratio, is demanding and time-consuming; thus, it is rarely used in daily practice (6).
Our study aimed to develop a practical visual grading system to assess atrophy of the supraspinatus muscle on MRI and to investigate the interobserver reproducibility and diagnostic feasibility of the grading system.
Our Institutional Review Board approved this retrospective study and waived the patient informed consent, as all MRIs were obtained following our clinical protocol and patient confidentiality was maintained.
As the study coordinator, one musculoskeletal radiologist with 6 years of musculoskeletal image interpretation experience collected the MRIs and reviewed clinical history. The study initially included 212 consecutive shoulder MRI examinations in our institution between December 2010 and July 2011; they were performed in the setting of routine clinical care. Twenty shoulder MRI examinations were regarded as inappropriate for analysis due to irrelevant imaging plane, artifacts or underlying diseases such as trauma or tumor. The remaining 192 shoulder MRI examinations, which were taken on 128 right and 64 left shoulders, were finally included. The supraspinatus tendon tears were identified on 126 shoulder MRI examinations. As four patients underwent shoulder MRI examinations for bilateral shoulders, there were 188 patients (age range, 22-82; 61.1 ± 10.7 years) in this study: 83 men (23-80; 60.1 ± 10.8 years) and 105 women (22-82; 61.8 ± 10.7 years).
All shoulder MRI examinations were performed at our institution: 137 examinations on 1.5-T (Signa HDxt 1.5-T, GE Healthcare, Milwaukee, WI, USA) scanner and 55 examinations on 3.0-T (MAGNETOM Trio/Verio, Siemens Medical Solutions, Erlangen, Germany) MRI scanners. The patients were placed in the supine position with forearm orgturned to the semi-pronation (neutral) position. The MRI protocol included oblique sagittal T1-weighted fast spin-echo images obtained on a plane perpendicular to the scapular body (repetition time/echo time, 400-800/10-15 ms; slice thickness, 4 mm; slice gap, 0.4 mm; field of view, 16 cm; matrix, 320 × 192; flip angle, 90°; and echo train length, 4).
Supraspinatus muscle atrophy was analyzed on the most lateral image of the scapular spine at the junction with the scapular body on the oblique sagittal T1-weighted image (6). An imaginary line along the inferior border of the trapezius, distal clavicle, and scapula delineated the supraspinatus fossa (Fig. 1). The occupation ratio of the cross-sectional area of the supraspinatus muscle to the supraspinatus fossa was evaluated by visual assessment, and the severity of supraspinatus muscle atrophy was graded on a 3-point scale: grade 1, defined as minimal to mild atrophy of the supraspinatus muscle, occupation ratio ≥ 60%; grade 2, defined as moderate atrophy, 30-59%; grade 3, defined as severe atrophy, < 30% (Fig. 2).
Three fellowship-trained radiologists, with 18, 6, and 6 years of experience in musculoskeletal MRI interpretation, respectively, participated independently in the visual assessment using a picture archiving and communication system (PACS) workstation according to the method described above. One of the two 6-year-experienced radiologists was the study coordinator. Before the individual review, they trained themselves together by measuring the cross-sectional areas of the supraspinatus muscle and the supraspinatus fossa in a training dataset of 20 cases. The dataset was prepared by the study coordinator from consecutive shoulder MRI examinations performed in November 2010. The muscle atrophy of the supraspinatus muscle was supplementarily evaluated using the 2-grade tangent sign and the 3-grade modified tangent sign by the study coordinator. A line (tangent) was drawn through the superior borders of the scapular spine and the superior margin of the coracoid process. The tangent sign was defined as positive when the supraspinatus muscle did not cross the tangent (5). The modified the tangent sign was categorized as follows: grade 1, the muscle was superior to the tangent line; grade 2, the muscle just touched the tangent; grade 3, the muscle was clearly below the tangent (10).
After all visual analyses had been completed, the study coordinator measured all cross-sectional areas of the supraspinatus muscle and the supraspinatus fossa by manual contouring of the structures on the PACS workstation to calculate the absolute quantitative values of the occupation ratio to be used as the reference standard.
Another group of 100 consecutive patients, including 40 men (35-74; 56.7 ± 7.7 years) and 60 women (47-80; 61.5 ± 7.4 years), who had undergone rotator cuff repair surgery between December 2010 and April 2012 as well as both preoperative and postoperative MRI examinations of the shoulders, were also retrospectively indentified. Thirty-five patients were also included in the 188-patient cohort.
To determine retrospectively the association between the visual grades of supraspinatus atrophy (as described above) on preoperative MRI and occurrences of retear after rotator cuff repair as assessed with postsurgical MRI, the visual grading was applied to the group of 100 consecutive patients by the 18-year-experienced musculoskeletal radiologist. Other preoperative parameters including the patient's age, tendon tear size and grade of fatty degeneration of the supraspinatus were obtained (4). Postoperative MRI examinations were performed 8 to 21 (mean 12.3) months after the surgery. The repair integrity on postoperative MRI was classified into 3 types modifying Sugaya's system (14): type 1, repaired cuff of sufficient thickness; type 2, marked thinning or minor discontinuity; type 3, complete discontinuity. Type 2 and 3 were considered as a retear. The analysis of the 100-patient group was done 4 weeks after that of the 188-patient group.
The weighted kappa value with linear weights was used to assess the interobserver agreement of the visual grading system and the agreement between the visual grading and the reference standard grades. The weighted kappa value was interpreted as follows: slight (0-0.20), fair (0.21-0.40), moderate (0.41-0.60), substantial (0.61-0.80), and almost perfect (0.81-1.00) (15). Mann-Whitney U test was performed to compare the occupation ratio between tangent sign positive and negative groups. Chi-square test was used to compare the reference standard grades between tangent sign positive and negative groups. The linearly-weighted kappa value was also used to assess the agreement between the modified tangent sign and the reference standard grade. Association between the visual grades of supraspinatus atrophy on MRI at preoperative state and the postsurgical occurrences of retear was analyzed using the chi-square test and the multiple logistic regression. A p value < 0.05 was considered significant. The statistical analyses were performed using SPSS version 19.0 (SPSS Inc., Chicago, IL, USA) and MedCalc version 12.7.7 (MedCalc Software, Ostend, Belgium).
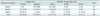
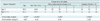
The cross-sectional areas of the supraspinatus muscle and the supraspinatus fossa are presented in Table 1. By quantitative analysis, 85 cases were classified as grade 1, 88 as grade 2, and 19 as grade 3. The mean weighted kappa value for the interobserver agreement of the visual MRI grading system was 0.74 with the following weighted kappa values (95% confidence interval [CI]) in three pairs: 0.70 (0.618-0.786); 0.77 (0.691-0.848); 0.75 (0.664-0.827).
Based on the quantitative measurement as a standard reference, the weighted kappa values showed good-to-excellent accuracy of the visual MRI grading method in all three readers (weighted kappa value and p value: 0.83, p < 0.001; 0.75, p < 0.001; 0.81, p < 0.001) (Table 2). The weighted kappa value for the agreement between the modified tangent sign and standard reference grade was 0.489 (95% CI, 0.389-0.589), which was quite smaller than the weighted kappa value of the visual MRI grading. The results of tangent sign and the modified tangent sign across the reference standard grades of the supraspinatus muscle atrophy are shown in Table 3. All grade 1 cases showed a negative tangent sign, and all grade 3 cases, except for one, showed a positive tangent sign. The majority (67 of 88, 76.1%) of patients with grade 2 muscle atrophy on the reference standard grades showed a negative tangent sign. As for the 3-grade modified tangent sign, substantial cases (57 of 88, 64.8%) of grade 2 (moderate) muscle atrophy on the reference standard grades also showed grade 1 on the modified tangent sign. Eight cases of grade 3 (severe) muscle atrophy on the reference standard grades showed grade 1 and grade 2 on the modified tangent sign.
The occupation ratio and the reference standard grades were significantly different between tangent sign positive and negative groups (p < 0.001). Figure 3 depicts a substantial overlap in grade 2 muscle atrophy between the two groups of tangent sign, although both groups were significantly different. Median values (interquartile range) were 32.7 (27.0-41.3) and 61.3 (53.5-67.7) in tangent sign negative and positive groups, respectively.
Table 4 shows a significant difference in the retear rates between the 3 grades of supraspinatus muscle atrophy in the univariable analysis (p < 0.001), i.e., the severer muscle atrophy, the higher retear rate. Among other preoperative variables, the tendon tear size and the grade of muscle fatty degeneration were also significantly related to postoperative tendon integrity in the univariable analysis. However, these were not significantly and independently associated with the postsurgical occurrence of retear according to the multivariable analysis.
Rotator cuff tears induce structural changes in the muscle such as atrophy and fatty degeneration. Fat accumulation appears both within and around the muscle only after 4 weeks following a tendon tear (3). Intramuscular fat accumulation is considered as fatty degeneration of the rotator cuff muscle, whereas extramuscular fat accumulation forms a fatty environment that compensates for muscle atrophy (3). The dominant theories on the pathogenesis of muscle atrophy in rotator cuff tendon tears are muscle disuse and traction injury of the suprascapular nerve (16). Muscle atrophy and fatty degeneration, which are considered to be possibly linked, are important negative prognostic factors for clinical and structural outcome after repair (3, 7, 8, 9, 10, 11, 12, 13). As these structural changes are progressive and irreversible and the repair of a torn rotator cuff tendon prevents further fat accumulation, it is important to repair rotator cuff tears before the irreversible changes advance (7, 9, 17).
Magnetic resonance imaging, which is the standard of reference for assessing the rotator cuff, allows accurate evaluation of the pathology and the quality of the rotator cuff muscles, which are crucial for appropriate decision making and predicting the prognosis (1, 3, 18). Goutallier et al. (4) established the classification of fatty degeneration on the basis of fatty steaks within the muscle belly on computed tomography. This classification has been widely used in the clinical setting and validated by MRI (10, 11).
Efforts have been made to assess muscle atrophy as distinct from fatty degeneration. Thomazeau et al. (5) introduced a measurement of supraspinatus muscle atrophy by calculating the occupation ratio of the supraspinatus muscle to the supraspinatus fossa on the Y-shaped view and proposed a three-stage classification method: a normal or slightly atrophied muscle with a ratio between 1.00 and 0.60 is stage 1; moderate atrophy between 0.60 and 0.40 is stage 2; and severe atrophy below 0.40 is stage 3. The severity of supraspinatus muscle atrophy has relation to the aggravation of tendinopathy and the limit of successful direct repair. They suggested a three stage turning point of supraspinatus muscle according to the supraspinatus tear and extension to subscapularis or infraspinatus, and explained that Grades 1 and 2 might predict a reliable direct repair. Grade 3 supraspinatus with a questionable elasticity and viability indicates surgical difficulties and unreliability of direct sutures (5). Liem et al. (10) modified the tangent sign and suggested qualitative three-stage system corresponding to Thomazeau et al. (5). As their results, the retear group had significant greater preoperative atrophy of supraspinatus tendon than intact-repair group, and the retear rate was higher in Grade 2 atrophy than in Grade 1 atrophy. The concept of our grading system is similar to the Thomazeau staging system, but we use 0.30 instead of 0.40 as the cut-off value of severe atrophy in consensus with our shoulder surgeon.
According to our results, the visual MRI grading system showed sufficient interobserver agreement and accuracy to explain the degree of supraspinatus muscle atrophy in a practical way. Despite being based on the occupation ratio, our grading system is different from Thomazeau's method in that we intended to develop a visual grading system to assess supraspinatus muscle atrophy without manual drawing of the boundaries of the muscle and surrounding anatomical structures. Region-of-interest tools can be used in the PACS era to measure areas of the supraspinatus muscle and fossa. Our experience is that such measurements are helpful to accustom ourselves to grading supraspinatus muscle atrophy at the initial stage of evaluation. Since then, we have accomplished visual grading of supraspinatus atrophy with a high level of accuracy and much more rapidly than the quantitative grading method. We are currently trying to use our visual grading system for the other rotator cuff muscles to which Thomazeau's method cannot be applied.
Zanetti et al. (6) suggested the tangent sign to assess the presence or the absence of supraspinatus muscle atrophy, and this method allows for a quick qualitative assessment of supraspinatus muscle atrophy. The tangent sign is widely used to assess supraspinatus muscle volume due to its feasibility and repeatability. Our results showed that the tangent sign could be useful to distinguish severe muscle atrophy from minimal or mild atrophy. However, the use of the tangent sign was limited for moderate muscle atrophy; a considerable number of cases (23.9%) with moderate atrophy had a positive tangent sign, so that they could be regarded as contraindicated for rotator cuff repair. From a surgical point of view, we believe the three-grade evaluation for supraspinatus muscle atrophy is more practical than the two-point tangent sign classification.
Liem et al. (10) modified the tangent sign and suggested qualitative three-stage system. This method is not frequently used in practice though it allows for a quick assessment of supraspinatus muscle atrophy. Our results also showed that the modified tangent sign tended to underestimate the grade of supraspinatus muscle atrophy. A substantial number of cases (64.8%) with moderate atrophy had Grade 1 on modified tangent sign. A considerable number of cases with severe atrophy showed Grade 1 (5.3%) and Grade 2 (36.8%) modified tangent sign; this results from the fact that the sole area of concern is the upper part of the supraspinatus muscle. Finally, we demonstrated increasing retear rate of rotator cuff with increasing the severity of supraspinatus muscle atrophy and suggested the potential usefulness of this visual MRI grading system in daily interpretation of shoulder MRI. Although the multivariable logistic regression model did not reveal a significantly independent association between the visual grading of muscle atrophy and retear, this is likely since supraspinatus atrophy is often observed concomitantly with other preoperative findings (i.e., multicollinearity). As shown by the univariable analysis, we believe that three-point visual MRI grading of supraspinatus muscle atrophy as well as staging of fatty degeneration would help surgeons determine the indications for surgery.
Our study had limitations. First, we did not correlate visual MRI grading with clinical symptoms and function. As our study was retrospective, it was difficult to obtain precise clinical information. Second, the occupation ratio at the level of the scapular spine in contact with the scapular body may have been influenced by the retraction of the myotendinous junction and not be representative of the total muscle volume (1, 6). Third, we analyzed the relationship between repair integrity and supraspinatus muscle atrophy, however, there are multiple factors associated with surgical outcome after rotator cuff repair.
Our study demonstrated that a visual MRI grading system is a reliable qualitative assessment method for atrophy of the supraspinatus muscle. This grading system for supraspinatus muscle atrophy would allow precise communication between physicians and help surgeons make decisions.
Figures and Tables
Fig. 1
MRI assessment of supraspinatus muscle volume.
Supraspinatus atrophy was analyzed on most lateral image of scapular spine (arrowheads) in contact with scapular body (arrows) on oblique sagittal T1-weighted image. Imaginary line along inferior border of trapezius (T), distal clavicle (C), and scapula delineated supraspinatus fossa (dashed line). Occupation ratio of supraspinatus muscle in supraspinatus fossa was evaluated visually.
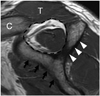
Fig. 2
Grading of supraspinatus muscle atrophy.
A. Grade 1, minimal to mild atrophy of supraspinatus muscle, occupation ratio ≥ 60%. B. Grade 2, moderate atrophy of supraspinatus, occupation ratio 30-59%. C. Grade 3, severe atrophy of supraspinatus, occupation ratio < 30%.

Fig. 3
Boxplot showing distribution of occupation ratio in both tangent sign positive and negative groups. Considerable overlap was observed in grade 2 muscle atrophy between two tangent sign groups. Boxes indicate first to third quartiles, each midline indicates median (second quartile), and whiskers represent maximum and minimum values within interquartile range.
Table 1
Cross-Sectional Areas of Supraspinatus Muscle and Supraspinatus Fossa for Each Reference Standard Grade of Muscular Atrophy

Table 2
Distribution of Supraspinatus Muscle Atrophy by Reference Standard Grade and Visual Grading System in Three Readers
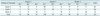
Table 3
Tangent Sign and Modified Tangent Sign Across Reference Standard Grades of Supraspinatus Muscle Atrophy
References
1. Tingart MJ, Apreleva M, Lehtinen JT, Capell B, Palmer WE, Warner JJ. Magnetic resonance imaging in quantitative analysis of rotator cuff muscle volume. Clin Orthop Relat Res. 2003; (415):104–110.
2. Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995; 77:10–15.
3. Trudel G, Ryan SE, Rakhra K, Uhthoff HK. Extra- and intramuscular fat accumulation early after rabbit supraspinatus tendon division: depiction with CT. Radiology. 2010; 255:434–441.
4. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994; (304):78–83.
5. Thomazeau H, Rolland Y, Lucas C, Duval JM, Langlais F. Atrophy of the supraspinatus belly. Assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand. 1996; 67:264–268.
6. Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Invest Radiol. 1998; 33:163–170.
7. Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007; 35:719–728.
8. Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003; 12:550–554.
9. Goutallier D, Postel JM, Lavau L, Bernageau J. [Impact of fatty degeneration of the suparspinatus and infraspinatus msucles on the prognosis of surgical repair of the rotator cuff]. Rev Chir Orthop Reparatrice Appar Mot. 1999; 85:668–676.
10. Liem D, Lichtenberg S, Magosch P, Habermeyer P. Magnetic resonance imaging of arthroscopic supraspinatus tendon repair. J Bone Joint Surg Am. 2007; 89:1770–1776.
11. Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999; 8:599–605.
12. Pfirrmann CW, Schmid MR, Zanetti M, Jost B, Gerber C, Hodler J. Assessment of fat content in supraspinatus muscle with proton MR spectroscopy in asymptomatic volunteers and patients with supraspinatus tendon lesions. Radiology. 2004; 232:709–715.
13. Khoury V, Cardinal E, Brassard P. Atrophy and fatty infiltration of the supraspinatus muscle: sonography versus MRI. AJR Am J Roentgenol. 2008; 190:1105–1111.
14. Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am. 2007; 89:953–960.
15. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174.
16. Resnick D, Kang HS. Internal derangements of joints: Emphasis on MR imaging. 1st ed. Philadelphia: W.B. Saunders Company;1997. p. 165–309.
17. Melis B, DeFranco MJ, Chuinard C, Walch G. Natural history of fatty infiltration and atrophy of the supraspinatus muscle in rotator cuff tears. Clin Orthop Relat Res. 2010; 468:1498–1505.
18. Strobel K, Hodler J, Meyer DC, Pfirrmann CW, Pirkl C, Zanetti M. Fatty atrophy of supraspinatus and infraspinatus muscles: accuracy of US. Radiology. 2005; 237:584–589.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download