Abstract
Objective
To evaluate the value of spinal and paraspinal anatomic markers in both the diagnosis of lumbosacral transitional vertebrae (LSTVs) and identification of vertebral levels on lumbar MRI.
Materials and Methods
Lumbar MRI from 1049 adult patients were studied. By comparing with the whole-spine localizer, the diagnostic errors in numbering vertebral segments on lumbar MRI were evaluated. The morphology of S1-2 disc, L5 and S1 body, and lumbar spinous processes (SPs) were evaluated by using sagittal MRI. The positions of right renal artery (RRA), superior mesenteric artery, aortic bifurcation (AB) and conus medullaris (CM) were described.
Results
The diagnostic error for evaluation of vertebral segmentation on lumbar MRI alone was 14.1%. In lumbarization, all patients revealed a well-formed S1-2 disc with squared S1 body. A rhombus-shaped L5 body in sacralization and a rectangular-shaped S1 body in lumbarization were found. The L3 had the longest SP. The most common sites of spinal and paraspinal structures were: RRA at L1 body (53.6%) and L1-2 disc (34.1%), superior mesenteric artery at L1 body (55.1%) and T12-L1 disc (31.6%), and AB at L4 body (71.1%). CM had variable locations, changing from the T12-L1 disc to L2 body. They were located at higher sacralization and lower lumbarization.
Lumbosacral transitional vertebrae (LSTVs) are common congenital anomalies, which are best evaluated on direct roentgenograms. The reported prevalence of this anomaly was between 3% and 30% (1-7). In LSTV, either the last lumbar vertebra (L5) with varying degrees of fusion to the sacrum, or the first sacral segment (S1) was separated from the sacrum with transition to lumbar configuration. The terminology of "LSTV" is used, because it is challenging of deciding whether a transitional vertebra is "sacralized L5" or "lumbalized S1" (1, 2).
Magnetic resonance images are commonly used for diagnosis of lumbosacral diseases. Identification of LSTVs on lumbar MRI is very important, because incorrect numbering of vertebral levels can cause wrong levels of surgery. In clinical practices, the radiologists often have to read lumbar MRI in isolation without the help of radiographs, and they usually try to define vertebral levels on the sagittal images according to the morphologic parameters, including the configurations of S1-2 disc, the vertebral body shape, and the lumbosacral angle (4, 8, 9). On the lumbar MRI alone, it is often difficult to recognize LSTVs, as these criteria are not reliable all the time.
In an effort to increase the diagnostic accuracy of LSTVs, various spinal and paraspinal structures, including the confluence of inferior vena cava, aortic bifurcation (AB), right renal artery (RRA), celiac trunk, root of superior mesenteric artery (RSMA), iliolumbar ligament, and conus medullaris (CM) have been used as anatomic landmarks, and are found to be helpful for the identification of LSTVs excluding CM (4-6).
Since Hahn et al. (10) used an additional sagittal cervicothoracic localizer images for objective determinations of the vertebral levels on lumbar MRI, many studies used a combination of cervicothoracic and lumbosacral localizers in numbering lumbar vertebrae (4, 6, 7).
The aim of our study was, in a larger patient group, to evaluate the values of spinal and paraspinal anatomic markers, such as RRA, RSMA, AB, and CM, in both the diagnosis of LSTVs and identification of vertebral levels on lumbar MRI.
The study was approved by our institutional review board. Lumbar MRI performed on 1265 patients between March 2011 and November 2011 were studied. The patients were referred for evaluations of low back pains or radiculopathy. After the reviews, 216 cases with extremely tortuous aorta, aortic aneurysm, multiple RRA, and the findings or history of spinal deformities, trauma, infection, tumor and previous spinal surgery were excluded. The final study group therefore involved 1049 adult patients (older than 16 years) with a mean age of 45.8 years (649 women, 400 men; age range, 17-86 years).
MRI was performed by using a 3.0 tesla unit (Magnetom Verio; Siemens, Erlangen, Germany) with a phased array spine matrix coil. On lumbar MRI, the T2-weighted (T2W) turbo spin echo (TSE) (repetition time [TR]/echo time [TE], 4000/103) and T1-weighted (T1W) spin echo (500/9.7) sequences were obtained in the sagittal plane with the following parameters: number of excitation (NEX), 3; slice thickness/interslice gap, 4/1 mm; field of view (FOV), 280 × 280 mm; matrix, 269 × 384 for T2W and 288 × 384 for T1W imaging. Axial T2W TSE (3000/112) images acquired parallel to the intervertebral discs were obtained with the following parameters: NEX, 3; slice thickness/interslice gap, 4/0.6 mm; FOV, 220 × 220 mm; matrix, 288 × 384.
Additional sagittal whole spine localizer (WSL) beginning from C2 to coccygeal levels was acquired with a combination of head, neurovascular, and spine matrix coils (Fig. 1). WSL was made from 12 sagittal images of half-Fourier acquisition single shot turbo spin-echo (TR/TE, 1000/92; NEX, 1; slice thickness/inter slice gap, 4/0.8 mm; FOV, 320 × 320 mm; matrix, 218 × 320), which is a high speed T2W sequence. The total acquisition time was 36 seconds. Commercially available composing software was used to create a composite image with twelve sagittal slices of the whole spine.
Sagittal WSL was used as a golden standard in identification of vertebral levels and the diagnosis of LSTVs. The vertebrae were counted down from C2, assuming that there were seven cervical and twelve thoracic vertebrae. On sagittal WSL, a patient was defined as having normal lumbosacral segmentation when the last squared vertebra was L5, and it was separated from the sacrum by a well-formed disc material with a sharp angulation at the lumbosacral junction.
To evaluate the diagnostic errors in the identification of vertebral levels on routine lumbar MRI, the presence of LSTV and the level of L5 were defined on sagittal images in the consensus of two radiologists blinded to the findings on WSL. These radiologists had 10 and 14 years of experiences in musculoskeletal imaging, respectively. There was no imaging method for verifying the numbers of vertebral segments. We tried to define the vertebral levels on sagittal MRI, according to the morphologic parameters, including the last squared vertebra which belonged to L5. There was a well-formed disc between L5 and S1 vertebral body, and there was a sharp angle at the level of L5-S1.
All morphologic evaluations were performed by following the identification of vertebral levels on sagittal WSL. The morphology of the first sacral intervertebral disc (S1-2) was characterized according to O'Driscoll et al. (11) into one of four types (Table 1). We evaluated the shapes of L5 and S1 body by measuring the end-plate ratios of each vertebra on sagittal MRI. The ratio of each vertebral body was calculated by dividing the length of superior end-plate to the inferior end-plate. We accepted the end-plate ratios closer to 1.0 as "rectangular shaped", and the ratios more than 1.1 as a "rhombus shaped" (4). We also defined the levels of the longest lumbar spinous process (SP) on the sagittal lumbar MRI.
According to vertebral levels of sagittal WSL, the locations of proximal RRA, RSMA, AB and CM were described as the levels of vertebral body or intervertebral disc. The locations of proximal RRA and RSMA were determined on sagittal T1W and T2W images by drawing vertical lines from these structures to the neighboring vertebral segments. The position of AB was defined at the levels where the abdominal aorta bifurcates into the right and left common iliac arteries on axial T2W images. The CM was defined as the most distal point of the spinal cord and located on sagittal images. Axial T2W images were used for confirmation of this location.
Statistical analyses were performed by using PASW Statistics software (version 18; SPSS Inc., Chicago, IL, USA). The variables were investigated using visual (histogram, probability plots) and analytical methods (Kolgomorov-Smirnov/Shapiro-Wilk's test) to determine whether they were normally distributed. Descriptive analyses were presented by using means, standard deviations and percentages for normally distributed RRA, RSMA, AB, and CM variables in each group. Comparisons among the normal, sacralization, and lumbarization groups were performed by using the t test for continuous variables, and chi-square test or Fisher exact test, where appropriate, for ordinal variables. An overall p value of less than 0.05 was considered to display statistically significant results.
On WSL, 864 patients (82.4%) had normal segmentations and 185 (17.6%) had LSTVs. We found sacralization and lumbarization in 105 (10.0%) and 80 (7.6%) cases, respectively.
On sagittal lumbar MRI, the LSTVs were diagnosed correctly in 120 out of 185 patients (64.9%), and misdiagnosed as having normal segmentation in 65 out of 185 cases (35.1%). From a total of 120 correctly diagnosed LSTVs, the L5 was defined incorrectly in 72 patients (60%). In the normal group, 11 out of 864 patients (1.3%) were misdiagnosed as having LSTVs. As a result, there were diagnostic errors in 148 out of 1049 patients (14.1%). Table 2 summarizes these findings.
In the normal group, there were only eight cases (0.9%) with type 3 and four cases with type 4 (0.5%) of S1-2 disc configuration. In sacralization, there were no type 3 or 4 configurations. All 80 cases with lumbarization revealed a type 4 disc morphology (Fig. 2).
The average end-plate ratios of L5 were statistically different in the normal and sacralization groups, which were 1.02 ± 0.05 vs. 1.29 ± 0.25, respectively. There were also statistically different average end-plate ratios of S1 in the normal and lumbalization groups, which were 1.65 ± 0.21 and 1.05 ± 0.06, respectively. The L5 body showed a rhombus shape in sacralization group, and S1 body showed a rectangular shape in lumbarization group (Figs. 2, 3).
L3 had the longest SP in the normal, lumbarization and sacralization groups, in 84.3%, 97.5%, and 58.1% of the patients, respectively. There were statistical differences between these groups.
In the normal group, the proximal RRA was most prevalent at L1 body and L1-2 disc, in 53.6% and 34.1% of the cases, respectively (Fig. 4A). The RSMA was most commonly found at L1 body and T12-L1 disc, in 55.1% and 31.6%, respectively (Fig. 4B). The AB was most prevalent at L4 body in 71.1% of the patients (Fig. 4C). The CM was variably located at L1 body, L1-2 disc, L2 body, T12-L1 disc, and T12 body, in 44.8%, 23.6%, 17.7%, 8.7%, and 3.5% of the cases, respectively (Fig. 5).
In lumbarization; the proximal RRA was most commonly located at L1-2 disc and L2 body, in 43.8% and 35.0% of the cases, respectively. The RSMA was most prevalent at L1 body and L1-2 disc, in 58.8% and 28.8% of the cases, respectively. The AB was located at the L4 body, L4-5 disc, and L5 body in 42.5%, 32.5%, and 20% of the cases, respectively. The CM was found to be at the L2 body, L1-2 disc, L2-3 disc, and L1 body, in 37.5%, 21.3%, 21.3%, and 17.5% of the cases, respectively.
In sacralization, the proximal RRA was most prevalent at the L1 body and T12-L1 disc, in 55.2% and 29.5% of the patients, respectively. The RSMA was located at the T12 body, T12-L1 disc, and L1 body, in 42.9%, 35.2%, and 20% of the cases, respectively. The AB was located primarily at the L3 body and L3-4 disc, in 51.4% and 32.4% of the cases, respectively. The CM was most prevalent at the L1 body in 55.2% of the cases. Thus, it was at T12-L1 disc, L1-2 disc, and T12 body, with 18.1%, 12.4%, and 9.5% of the cases, respectively.
Comparing with the normal group, the proximal RRA, RSMA, AB, and CM were found to be located higher in the sacralization and lower in the lumbarization group. Figure 6 shows the comparison of locational distributions of these structures in the study groups.
The locational distributions of spinal and paraspinal anatomic markers showed statistically significant differences within and between these study (normal, sacralization, and lumbalization) groups (p < 0.001).
Lumbosacral transitional vertebrae are common spinal anomalies which have a wide range of variability in degrees of morphologic features. This variability of morphology changes from broadened elongated transverse processes to either the formation of an anomalous articulation or the complete fusion of the transitional vertebrae (3). In 1984, Castellvi et al. (8) proposed a classification system and defined four subgroups according to the radiographic appearances. Type I has dysplastic transverse process (unilateral, Ia; bilateral, Ib); type II has pseudoarthrosis of LSTV with the adjacent sacral ala (unilateral, IIa; bilateral, IIb); type III has fusion of LSTV with the adjacent sacral ala (unilateral, IIIa; bilateral, IIIb); and type IV is mixed form with type IIa on one side and type IIIa on the other.
Magnetic resonance image is commonly indicated for the lumbosacral diseases. In clinical practices, the lumbar MRI is usually reported without the help of radiographs for the definition of vertebral levels, either because they have not yet been obtained or they are not available at the time of reporting MRI. Therefore, the diagnosis of LSTVs can be difficult for lumbar MRI alone. Even if the LSTV is suspected on MRI, the differential diagnosis between the sacralised L5 and lumbarised S1 can also be difficult.
The association of low back pains with LSTV, referred to as "Bertolotti's syndrome", is controversial. However, there may be symptoms originating from the degeneration of the anomalous articulation, facet joint arthrosis and nerve root compression between the broadened transverse process of the last lumbar segment and the sacral ala (3, 12, 13). Additionally, there are studies which reported increased incidences of disc degeneration and disc herniation above the LSTV (2, 8-10, 13, 14). As most surgical errors occur in patients with LSTVs, the radiologists should diagnose this anomaly and define the vertebral segments in order to avoid wrong levels of spinal surgery or interventional procedures (14, 15). On routine lumbar MRI, the radiologists usually try to define the vertebral levels on sagittal views, according to the morphology of S1-2 disc, vertebral body shapes and lumbosacral angle (4). However, as reported in many studies, these morphologic criteria may lead to misidentification of vertebral segments and misdiagnosis of LSTV (3-5, 11). Our study also revealed that according to these criteria, 1.3% of the patients with normal segmentation were misdiagnosed as having LSTV, 35.1% of the patients with LSTV were misdiagnosed as having normal segmentation, and 60% of the patients with correctly diagnosed LSTV had incorrect number of vertebral levels.
O'Driscoll et al. (11) described four types of S1-2 disc morphology on MRI according to the appearance of the disc between the uppermost sacral segment and the remainder of the sacrum (S1-2). They correlated this classification system with the subtypes of LSTVs according to Castellvi et al. (8). In their study, there was type 4 S1-2 disc morphology in 12 out of 100 (12%) patients. The study showed a good correlation between a type 4 S1-2 disc morphology and the presence of LSTVs with the radiographic findings of fused LSTVs in 11 out of these 12 patients. Carrino et al. (5) also reported that from a total of twenty-two LSTVs cases, 36% had type 3 and 23% had type 4 morphology. Our study with a larger patient group revealed that all 80 patients with lumbarization showed type 4 morphology. Therefore, especially for lumbarization, the S1-2 disc morphology can cause misdiagnosis in definition of vertebral segments on lumbar MRI. As reported in the study by Carrino et al. (5), we found type 3 and 4 S1-2 disc configurations in patients with normal segmentation. On lumbar MRI, the S1-2 disc morphology can also lead to a misdiagnosis of LSTV in normal patients.
In general, the last vertebral body with a squared appearance is numbered as L5, and the first vertebral body with a rhombus shape is defined as S1 vertebra (6, 8). However, it has been reported in many studies that for patients with LSTVs, the S1 vertebra shows "squared" appearance in complete lumbarization, and the L5 vertebra has a "rhombus" shape in complete sacralization (4, 15-17). We also found similar findings with the literature. Accordingly, the shapes of vertebral bodies in lumbosacral junctions can cause misdiagnosis in vertebral numbering and diagnosis of LSTVs.
To evaluate the diagnostic importance of the longest lumbar SP in the identification of vertebral levels, we defined the level according to the sagittal lumbar MRI. There are only a few studies which regard the quantitative anatomy of the lumbar SP (18, 19). In our study, we had similar findings with reported studies which claimed that L3 had the longest SP in most of the patients from the study groups. We assumed that the tip of the longest lumbar SP, such as that of L3, could be used as a preoperative anatomic landmark in order to avoid wrong level surgery.
There are several studies which evaluate various spinal and paraspinal structures as anatomic landmarks for numbering vertebral levels and identification of LSTVs (4-6). In our study, we assessed the proximal RRA, RSMA, AB, and CM, as they can be evaluated on routine lumbar MRI.
Lee et al. (6) found that, in the normal group, the ostia of RRA was sited between the lower half of L1 and the upper half of L2 body in 92% of the patients when focusing on the L1-2 disc. Other studies also reported that RRA are usually located near the L1-2 disc on lumbar MRI, and recommended as a useful anatomic marker for numbering vertebral levels (1, 20). Although they could not have seen RRA in some patients, we did not have any difficulties for evaluations of RRA, and found that it was the most prevalent at L1 body or L1-2 disc in 87.7% of the cases.
We found that, in the normal group, the RSMA was most prevalent at L1 body and T12-L1 disc in 86.7% of the cases. Lee et al. (4) also reported that, in the normal group, the RSMA was concentrated in the area between T12-L1 disc and the upper half of L1 in 73.5% of the cases.
According to Gray's Anatomy (21), AB is located at L4 body. In MRI studies by Lee et al. (6) and Chithriki et al. (22), AB was found at L4 body in 83% and 67% of the cases, respectively. Another study by Lee et al. (4) revealed that in the normal group, the AB was most prevalent between the upper half of L4 body and L4-5 disc in 94.8% of the cases. Our study demonstrated that, in the normal group, the AB was most commonly located at L4 body in 71.1% of the patients.
In the literature, paraspinal structures; such as RRA, superior mesenteric artery, and AB, have been proposed as useful anatomic landmarks in definition of vertebral levels on lumbar MRI (4-6). On the other hand, as these structures are prone to substantial errors, the findings of their locations are found to be unsatisfactory (1, 23).
According to literature, the termination of CM showed a great variation which may be as high as T12 vertebra or as low as L2-3 disc (6, 24). We also had similar findings that CM had variable locations, which change from T12-L1 disc to the L2 body. Therefore, the CM cannot be used as a reliable anatomic landmark for numbering lumbar vertebrae.
In our study, we found the levels of the RRA, RSMA, AB, and CM higher in sacralization and lower in lumbarization. It was also reported by other studies (4, 6, 22) and they suggested that if these structures were located outside of the frequent sites, the presence of LSTV should be suspected. However, when using the lumbar MRI alone, we defined vertebral levels incorrectly in 14.1% of the patients. In LSTV, although these anatomic structures are expected to be located differently from the frequent sites, this finding was helpful in patients with misnumbered vertebral levels.
Hahn et al. (10) used an additional sagittal cervicothoracic localizer in lumbar MRI for accurate identifications of LSTVs and disease location. Some other studies also used cervicothoracic localizers as a gold standard for numbering vertebral levels (4, 6, 7). They counted the vertebrae down from C2 rather than up from L5. Peh et al. (7) found that by using the sagittal and coronal lumbosacral localizer MRI alone, the lumbar vertebral levels could be defined correctly in 80.2% and 82.2% of the patients, respectively. We also found that when not using the sagittal WSL, there was 14.1% diagnostic error in definition of LSTVs or numbering of vertebral levels on lumbar MRI. As reported by Hahn et al. (10), WSL ensures consistently accurate numbering of the vertebrae and does not require excessive additional imaging time. During their study, an additional 2 minutes was required for WSL images. With the advantages of phase-array coils and a high speed T2W sequence, it only took 36 seconds in our study, and we also suggested the use of additional sagittal WSL for reporting routine lumbar MRI.
Our study had the advantages of using WSL from all patients. We used a phased array spine coil which allowed the whole spine to be imaged without the need for movement of the coil or the patient. Involvement of 185 cases with LSTVs is another advantage of our study. To the best of our knowledge, this is the largest patient group to be studied in the literature. Our study had some limitations. We used WSL as a golden standard for numbering the vertebrae, assuming that there were seven cervical and twelve thoracic vertebrae. Although cervical spine has a fixed vertebral number of seven, various segmentation anomalies at thoracolumbar junction can change the thoracic and lumbar vertebrae numbers (3, 5). As we did not have the patients' radiographs including thoracolumbar junctions, we could not identify the lowest rib-bearing vertebra as the last thoracic vertebra, and compare the results with that of WSL. It was a retrospective study which involved the routine lumbar MRI. As the routine lumbar MRI did not include coronal imaging and we did not have the patients' lumbosacral roentgenograms, we could not evaluate the lumbar transvers processes and define the LSTV subgroups. Therefore, the spinal morphologic parameters could not have been compared between LSTV subgroups. Another limitation was that the axial images were obtained through intervertebral discs on routine lumbar MRI, where in some cases we had difficulties for defining locations of AB and CM. We tried to solve this problem with the help of evaluating both sagittal and axial images.
In conclusion, we can have errors for identifying correct vertebral level on sagittal lumbar spine MRI, especially in population with LSTVs. Additionally, the spinal morphologic features and locations of the spinal and paraspinal anatomic structures on lumbar MRI are not completely reliable for diagnosis of LSTVs and definition of vertebral levels.
Figures and Tables
Fig. 1
Example of sagittal whole-spine localizer image with half-Fourier acquisition single shot turbo spin-echo sequence for numbering lumbar vertebrae.
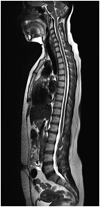
Fig. 2
Sagittal T2-weighted MRI of man with lumbarization of S1 vertebra (thick arrow). There is well-formed S1-2 disc (thin arrow) with squaring of S1 vertebral body (thick arrow).

Fig. 3
Sagittal T2-weighted MRI of woman demonstrates sacralization of L5 vertebra (arrow). L5 body shows rhombus shape similar to S1 vertebra.

Fig. 4
Sagittal T2-weighted images (A-C) of man with normal lumbar segmentation.
A. Proximal right renal artery (arrow) is located at L1-2 disc space. B. Root of superior mesenteric artery (arrow) is positioned at L1 body. C. Aortic bifurcation (arrow) is located at L4 body.
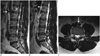
Fig. 5
Sagittal T2-weighted MRI of woman with normal lumbar segmentation shows that conus medullaris (arrow) is located at L1 body.

Fig. 6
Comparison on locational distributions of spinal and paraspinal structures in study groups. RRA = right renal artery, RSMA = root of superior mesenteric artery, CM = conus medullaris, AB = aortic bifurcation

Table 1
Classification of First Sacral Intervertebral Disc (S1-2) According to O'Driscoll et al. (11)

Acknowledgments
We highly appreciate the technical support by Ercan Carmikli, who works as MRI technician in Gazi University Department of Radiology.
References
1. Hughes RJ, Saifuddin A. Numbering of lumbosacral transitional vertebrae on MRI: role of the iliolumbar ligaments. AJR Am J Roentgenol. 2006; 187:W59–W65.
2. Hughes RJ, Saifuddin A. Imaging of lumbosacral transitional vertebrae. Clin Radiol. 2004; 59:984–991.
3. Konin GP, Walz DM. Lumbosacral transitional vertebrae: classification, imaging findings, and clinical relevance. AJNR Am J Neuroradiol. 2010; 31:1778–1786.
4. Lee CH, Park CM, Kim KA, Hong SJ, Seol HY, Kim BH, et al. Identification and prediction of transitional vertebrae on imaging studies: anatomical significance of paraspinal structures. Clin Anat. 2007; 20:905–914.
5. Carrino JA, Campbell PD Jr, Lin DC, Morrison WB, Schweitzer ME, Flanders AE, et al. Effect of spinal segment variants on numbering vertebral levels at lumbar MR imaging. Radiology. 2011; 259:196–202.
6. Lee CH, Seo BK, Choi YC, Shin HJ, Park JH, Jeon HJ, et al. Using MRI to evaluate anatomic significance of aortic bifurcation, right renal artery, and conus medullaris when locating lumbar vertebral segments. AJR Am J Roentgenol. 2004; 182:1295–1300.
7. Peh WC, Siu TH, Chan JH. Determining the lumbar vertebral segments on magnetic resonance imaging. Spine (Phila Pa 1976). 1999; 24:1852–1855.
8. Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976). 1984; 9:493–495.
9. MacGibbon B, Farfan HF. A radiologic survey of various configurations of the lumbar spine. Spine (Phila Pa 1976). 1979; 4:258–266.
10. Hahn PY, Strobel JJ, Hahn FJ. Verification of lumbosacral segments on MR images: identification of transitional vertebrae. Radiology. 1992; 182:580–581.
11. O'Driscoll CM, Irwin A, Saifuddin A. Variations in morphology of the lumbosacral junction on sagittal MRI: correlation with plain radiography. Skeletal Radiol. 1996; 25:225–230.
12. Byun WM, Kim JW, Lee JK. Differentiation between symptomatic and asymptomatic extraforaminal stenosis in lumbosacral transitional vertebra: role of three-dimensional magnetic resonance lumbosacral radiculography. Korean J Radiol. 2012; 13:403–411.
13. Bron JL, van Royen BJ, Wuisman PI. The clinical significance of lumbosacral transitional anomalies. Acta Orthop Belg. 2007; 73:687–695.
14. Malanga GA, Cooke PM. Segmental anomaly leading to wrong level disc surgery in cauda equina syndrome. Pain Physician. 2004; 7:107–110.
15. Wigh RE. The thoracolumbar and lumbosacral transitional junctions. Spine (Phila Pa 1976). 1980; 5:215–222.
16. Wigh RE. Phylogeny and the herniated disc. South Med J. 1979; 72:1138–1143.
17. Wigh RE, Anthony HF Jr. Transitional lumbosacral discs. probability of herniation. Spine (Phila Pa 1976). 1981; 6:168–171.
18. Sobottke R, Koy T, Röllinghoff M, Siewe J, Kreitz T, Müller D, et al. Computed tomography measurements of the lumbar spinous processes and interspinous space. Surg Radiol Anat. 2010; 32:731–738.
19. Tan SH, Teo EC, Chua H. Quantitative three-dimensional anatomy of lumbar vertebrae in Singaporean Asians. Eur Spine J. 2002; 11:152–158.
20. Ralston MD, Dykes TA, Applebaum BI. Verification of lumbar vertebral bodies. Radiology. 1992; 185:615–616.
21. Healy JC, Borley NR, Mundy AR, Collins P, Wigley C. True pelvis, pelvic floor and perineum. In : Standring S, editor. Gray's anatomy: the anatomical basis of clinical practice. 39th ed. New York: Elsevier Churchill Livingstone;2005. p. 1360.
22. Chithriki M, Jaibaji M, Steele RD. The anatomical relationship of the aortic bifurcation to the lumbar vertebrae: a MRI study. Surg Radiol Anat. 2002; 24:308–312.
23. Kumar S, Neyaz Z, Gupta A. The utility of 64 channel multidetector CT angiography for evaluating the renal vascular anatomy and possible variations: a pictorial essay. Korean J Radiol. 2010; 11:346–354.
24. Williams A, Newell RLM, Collins P. Macroscopic anatomy of the spinal cord and spinal nerves. In : Standring S, editor. Gray's anatomy: the anatomical basis of clinical practice. 39th ed. New York: Elsevier Churchill Livingstone;2005. p. 775.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download