To the editors,
We read with great interest the article titled "Diffusion-Weighted Magnetic Resonance Imaging for the Evaluation of Prostate Cancer: Optimal B Value at 3T" by Ji Hyun Koo et al. (1), published in the Korean Journal of Radiology (DOI: 10.3348/kjr.2013.14.1.61). This article will be a useful diffusion weighted imaging (DWI) guide for radiologists in assessing prostatic cancer. In the paper, the authors compared 4 different b values and suggested them for predicting prostate cancer; the optimal b value for 3T DWI was found to be 1000 s/mm2.
However, even with high b values, the overlap of the apparent diffusion coefficient (ADC) limits the accuracy of DWI in cancer detection, particularly in the transitional zone tissue, due to its lower ADC compared to the peripheral zone tissue (2). Therefore, we aimed to mention that, with any b value, the assessment of the diffusion restriction should only be performed as a part routine multiparametric radiologic evaluation of the prostate gland. In addition, in lesions with small diameters, we suggest evaluating the diffusion restriction by a visual assessment of ADC maps instead of measuring ADC values, which can be challenging.
The authors also mentioned that they used T1 weighted images for lymph node detection. In our practice, we simply use DWIs in the detection of metastatic lymph nodes. In high b values, such as 1000 s/mm2, all lymph nodes appear to be hyperintense in contrast to the adjacent vessels. DWIs can also provide additional information in bone metastases and invasion of the adjacent tissues (3-5).
References
1. Koo JH, Kim CK, Choi D, Park BK, Kwon GY, Kim B. Diffusion-weighted magnetic resonance imaging for the evaluation of prostate cancer: optimal B value at 3T. Korean J Radiol. 2013; 14:61–69.
2. Kim JK, Jang YJ, Cho G. Multidisciplinary functional MR imaging for prostate cancer. Korean J Radiol. 2009; 10:535–551.
3. Battal B, Akgün V, Kocaoğlu M. Diffusion-weighted MRI beyond the central nervous system in children. Diagn Interv Radiol. 2012; 18:288–297.
4. Battal B, Kocaoglu M, Akgun V, Karademir I, Deveci S, Guvenc I, et al. Diffusion-weighted imaging in the characterization of focal liver lesions: efficacy of visual assessment. J Comput Assist Tomogr. 2011; 35:326–331.
5. Kocaoglu M, Bulakbasi N, Sanal HT, Kismet E, Caliskan B, Akgun V, et al. Pediatric abdominal masses: diagnostic accuracy of diffusion weighted MRI. Magn Reson Imaging. 2010; 28:629–636.
As a routine prostate MR imaging protocol, diffusion-weighted imaging (DWI) has several advantages for improving tumor detection and staging, conducting post-treatment follow-up, monitoring therapeutic effects after hormonal or radiation therapy and guiding targeted biopsy in patients with previous negative biopsy results. In addition, it can provide useful information for predicting tumor aggressiveness (1).
For optimal DWI, it is crucially important to determine the optimal values for factors in DWI, especially the b value, which is essential for developing high-quality apparent diffusion coefficient (ADC) maps that affect the accuracy of ADC measurements and visual imaging interpretations (2). For ADC analysis, by using two-point b-values (0 and each b value of 300, 700, 1000 and 2000 s/mm2) in predicting the cancer location, our results suggested that the optimal b value at 3T DWI was 1000 s/mm2. However, considering the performance of different MR scanners in clinical practice, we recommend the use of higher b values with 800-1000 s/mm2 instead of the use of any b values as you mentioned. If radiologists want to use multi-point b-values on DWI, b-values of 0, 100 and 800-1000 s/mm2 can be used as the minimal requirements (3). In addition, a careful selection of several DWI parameters is also recommended in order to obtain high-quality ADC maps: single-shot versus multi-shot EPI technique, adequate size of field of view to acquire better signal-to-noise ratio, fat-saturation techniques (spectral presaturation inversion recovery, short T1 inversion recovery, or spectral presaturation attenuated inversion recovery), mono-exponential versus bi-exponential model to fit the data, etc.
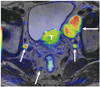
For evaluating nodal or bone metastasis, we agree that the DWI or diffusion-weighted whole-body imaging with background body signal suppression (DWIBS) can be a powerful tool (4). DWI or DWIBS can be used in conjunction with anatomical MR images (Figs. 1, 2). Metastatic nodes may have increased the cellular density or necrotic areas, which can further restrict or increase diffusion, respectively (5). Compared with soft tissue tumors, metastatic bone disease can be detected as an area of increased diffusivity relative to the restricted diffusion of normal fatty marrow (6). Thus, DWI or DWIBS has the potential to decrease the number of imaging studies required (from plain radiography to PET/CT).
Figures and Tables
References
1. Kim CK, Park BK, Kim B. Diffusion-weighted MRI at 3 T for the evaluation of prostate cancer. AJR Am J Roentgenol. 2010; 194:1461–1469.
2. Saritas EU, Lee JH, Nishimura DG. SNR dependence of optimal parameters for apparent diffusion coefficient measurements. IEEE Trans Med Imaging. 2011; 30:424–437.
3. Barentsz JO, Richenberg J, Clements R, Choyke P, Verma S, Villeirs G, et al. ESUR prostate MR guidelines 2012. Eur Radiol. 2012; 22:746–757.
4. Kwee TC, Takahara T, Ochiai R, Nievelstein RA, Luijten PR. Diffusion-weighted whole-body imaging with background body signal suppression (DWIBS): features and potential applications in oncology. Eur Radiol. 2008; 18:1937–1952.
5. Lin G, Ho KC, Wang JJ, Ng KK, Wai YY, Chen YT, et al. Detection of lymph node metastasis in cervical and uterine cancers by diffusion-weighted magnetic resonance imaging at 3T. J Magn Reson Imaging. 2008; 28:128–135.
6. Luboldt W, Küfer R, Blumstein N, Toussaint TL, Kluge A, Seemann MD, et al. Prostate carcinoma: diffusion-weighted imaging as potential alternative to conventional MR and 11C-choline PET/CT for detection of bone metastases. Radiology. 2008; 249:1017–1025.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download