Abstract
Objective
The current study retrospectively evaluated whether the percutaneous N-butyl cyanoacrylate (NBCA) seal-off technique is an effective treatment for controlling the angioplasty-related ruptures, which are irresponsive to prolonged balloon tamponade, during interventions for failed or failing hemodialysis vascular accesses.
Materials and Methods
We reviewed 1588 interventions performed during a 2-year period for dysfunction and/or failed hemodialysis vascular access sites in 1569 patients. For the angioplasty-related ruptures, which could not be controlled with repeated prolonged balloon tamponade, the rupture sites were sealed off with an injection of a glue mixture (NBCA and lipiodol), via a needle/needle sheath to the rupture site, under a sonographic guidance. Technical success rate, complications and clinical success rate were reported. The post-seal-off primary and secondary functional patency rates were calculated by a survival analysis with the Kaplan-Meier method.
Results
Twenty ruptures irresponsive to prolonged balloon tamponade occurred in 1588 interventions (1.3%). Two technical failures were noted; one was salvaged with a bailout stent-graft insertion and the other was lost after access embolization. Eighteen accesses (90.0%) were salvaged with the seal-off technique; of them, 16 ruptures were completely sealed off, and two lesions were controlled as acute pseudoaneurysms. Acute pseudoaneurysms were corrected with stentgraft insertion in one patient, and access ligation in the other. The most significant complication during the follow-up was delayed pseudoaneurysm, which occurred in 43.8% (7 of 16) of the completely sealed off accesses. Delayed pseudoaneurysms were treated with surgical revision (n = 2), access ligation (n = 2) and observation (n = 3). During the follow-up, despite the presence of pseudoaneurysms (acute = 1, delayed = 7), a high clinical success rate of 94.4% (17 of 18) was achieved, and they were utilized for hemodialysis at the mean of 411.0 days. The post-seal-off primary patency vs. secondary patency at 90, 180 and 360 days were 66.7 ± 11.1% vs. 94.4 ± 5.4%; 33.3 ± 11.1% vs. 83.3 ± 8.8%; and 13.3 ± 8.5% vs. 63.3 ± 12.1%, respectively.
Conclusion
Our results suggest that the NBCA seal-off technique is effective for immediate control of a venous rupture irresponsive to prolonged balloon tamponade, during interventions for hemodialysis accesses. Both high technical and clinical success rates can be achieved. However, the treatment is not durable, and about 40% of the completely sealed off accesses are associated with developed delayed pseudoaneurysms in a 2-month of follow-up. Further repair of the vascular tear site, with surgery or stent-graft insertion, is often necessary.
The most common complication that can occur during a percutaneous intervention is angioplasty-induced venous injury, which has been reported to occur at a rate ranging from 2.0% to 6.4% (1, 2). In most cases, manual compression or prolonged inflation of the angioplasty balloon, at the rupture site, is adequate for controlling extravasation and preserving the access function. However, for the rupture, which cannot be controlled by the repeated and prolonged balloon tamponade, a stent or stent-graft insertion is needed to salvage the access, and this procedure has been documented to be an effective bailout treatment (3-6). However, in situations in which the stents or stent-grafts are not considered as the treatment options (e.g., financial reasons or no stent of suitable size available), then intentional thrombosis of the access may be required to stop the bleeding. When such a rupture was encountered, it was our practice to perform the seal-off procedure, prior to the stent/stent-graft insertion, because the stent/stent-graft was expensive and not reimbursed in our country. We assessed the feasibility and safety of an alternative treatment to salvage the vascular accesses with such venous ruptures without using stent or stent-graft, which sealed off the rupture site with a percutaneous injection of n-butyl cyanoacrylate (NBCA). We, herein, report its technical success, complications, and clinical outcomes.
Institutional Review Board's approval, including a waiver of informed consent, was obtained for this study. The study was conducted retrospectively by reviewing an electronic patient database from the angiographic suite. We reviewed 1588 intervention procedures, performed in 1569 patients that occurred between September 2009 and May 2011, for dysfunctional and/or occluded vascular access sites. All procedures were performed by a vascular interventional radiologist and were part of the routine management of hemodialysis access failure with informed consent for the procedures.
The seal-off procedure was initiated by prolonged balloon inflation with the same the size angioplasty balloon, as the previous inflation, to cease extravasation temporarily.
When the bleeding stopped temporarily, the next step was to find the rupture site. Under a sonogram, with axial scanning along the inflated balloon, the vascular tear site could be identified as a "quarter-note sign" (Fig. 1A); for the rupture with a short note-stem, it looked like a teardrop (Fig. 1B). The note-stem could be long in the rupture, caused by an inadvertent perforation of the vascular wall with a thrombo-aspiration catheter or vascular introducer sheath or could be short when the rupture occurred immediately after the dilatation of the stenosis. To confirm an identified quarter-note sign to be the true vascular tear site, we partially deflated the balloon, and a sudden expansion of the note-head and note-stem could be seen; after confirmation, the balloon was re-inflated rapidly. There might be more than one quarter-note sign along the culprit venous segment for a grade 3 rupture; therefore, more than one injection was sometimes needed.
After a rupture site was confirmed, an 18G needle/needle sheath was advanced toward the rupture site under a local anesthesia and ultrasound guidance until its tip entered the note-stem and reached the inflated balloon. If the rupture was superficially located, such as in the forearm veins, an 18G, 2-inch, sheathed, IV needle (Jelco I.V. catheter; Smith Medical, Rossendale, Lancashire, UK) was used; if a rupture was located deep in the axilla, such as in the axillary vein, an 18G part bevel tip needle (TOP Corporation, Tokyo, Japan) was used. When a needle was advanced toward the rupture site, care was taken not to pierce the inflated balloon. For superficial ruptures, the operator could always see the tip of a needle sheath in contact with the inflated balloon surface (Fig. 1C). However, for deep ruptures, once the needle tip entered into the note-stem, where it was considered close enough for a glue mixture delivery, an injection would be performed.
The glue mixture was prepared by mixing 0.5 mL NBCA (Histoacyl; B. Braun) with 1.5 mL lipiodol (NBCA/lipiodol = 1/3), which was loaded in a 5-mL Luer-lock syringe. The syringe was connected directly to the needle/needle sheath. The glue mixture was manually injected under fluoroscopic monitoring. Injection was stopped when: 1) an increased resistance was felt, 2) the mixture was used up, or 3) unwanted interstitial infiltration of glue occurred (Fig. 2). After an injection, we waited for 60 seconds, and then we deflated the balloon and assessed the completeness of the seal-off. If the extravasation was still expanding, or if an acute pseudoaneurysm was noted, the balloon was re-inflated and a new seal-off attempt was commenced. Efforts were made to find another rupture site along the inflated balloon. Because the needle/needle sheath becomes occluded after an injection of the glue mixture, a new needle/needle sheath was required to perform the second injection at the new puncture site. The seal-off procedure was repeated until the rupture was controlled or when the rupture site was severely obscured by the echo-shadowing glue cast. Usually, more than one injection was required to achieve a complete seal-off. However, as the number of attempted injection and as the amount of glue mixture used increases, identification of the rupture site becomes more difficult, or even impossible.
The completeness of the seal-off was assessed by: 1) inspection using the bare eyes to assess whether or not the extremity swelling ceased, and 2) the follow-up sonogram and venography. The seal-off attempt stopped when the rupture was completely sealed off or was controlled as a stable-sized acute pseudoaneurysm. If the result was a failed seal-off and the hematoma continued expanding, a balloon was inflated to temporarily control the extravasation, during the procedure. It was explained to the patient and his/her family that there would be a high probability of losing the vascular access if no stent/stent-graft insertion was performed. An immediate decision was made as to whether or not to salvage the vascular access. If stent-graft insertion was not considered, then the access was intentionally thrombosed by a coil embolization (Fig. 3).
All the needles/needle sheathes were left in place after the injections, and were removed at the end of the seal-off procedure. After the removal of the needles/needle sheaths, the needle wounds on the skin were sealed off with undiluted NBCA or the remaining glue mixture.
After the seal-off, all patients were told to avoid glue cast dehiscence and re-bleeding by not doing any hand-arm exercises for at least 2 weeks, and keeping the seal-off site free of mechanical manipulation (e.g., local massage using heparinoid ointment for swelling and ecchymosis). Patients with complete seal-off were told to return for an outpatient visit 2 weeks later, and once a month, thereafter, for at least 3 visits. In the outpatient clinic, physical examinations and sonograms of the vascular access were performed. Complications were prospectively recorded on the chart. If the seal-off result was a stable-sized acute pseudoaneurysm after a 1-hour observation, the patients could go home. These patients and their family were informed of the risk of pseudoaneurysm rupture, and that a decision to insert a stent-graft or undergo a surgical revision/ligation should be made, as soon as possible (i.e., within 72 hours). Endoprosthesis was not an insurable procedure and it costs 3-5 times the average monthly household income in our country, but the surgical procedures were all insurable. Therefore, if the patient could not afford a stent/stent-graft, they could choose to have a regular monthly follow-up, surgical ligation or surgical revision, including aneurysmorrhaphy and graft interposition surgery.
During the follow-up, the vascular access team nurses referred patients for re-intervention according to the following criteria: 1) decreased intra-access flow during hemodialysis that could not support the prescribed hemodialysis dose, 2) abnormal physical examination findings suggesting anatomic lesions, 3) increased dynamic intra-access pressure (> 200 mm Hg) during hemodialysis, 4) vascular access-site thrombosis, and 5) immature vascular access.
A rupture irresponsive to prolonged balloon tamponade was termed in short here as a "grade 3 rupture", which was equivalent to the "grade 3 hematoma" defined by Beathard (7), and the "grade 3 lesions" by Dale et al. (5). A grade 3 rupture was defined clinically as a rupture that remained as a rapidly expanding hematoma, despite the repeated and prolonged balloon inflations at the rupture site (7), and in the venography, as an expanding hematoma with marked limitation of flow in the vascular access (5). In this study, prolonged balloon inflation was performed by inflating a balloon catheter for 1 minute initially, then deflating the balloon, and if ineffective, this procedure was followed by 2 cycles of 5-minute tamponade, as necessary. If the rupture remained uncontrolled, it was considered as a grade 3 rupture.
Under a sonogram, if the rupture site can be reached by an 18G, 2-inch IV needle, it was defined as a "superficial rupture" and if the rupture site can only be reached by using a longer needle, it was defined as a "deep rupture".
Technical success was defined when the rupture stopped expanding and was controlled after the seal-off. Technical success was classified as either 1) a complete seal-off (Fig. 4) with no extravasation or acute pseudoaneurysm in the completed venography, or 2) a stable-sized acute pseudoaneurysm (Fig. 2), which was defined as an acute pseudoaneurysm, showing no size enlargement for 30 minutes after the final injection of the glue mixture. During the 30-minute observation, a follow-up venography was performed every 5 minutes, or when there was evidence suggesting pseudoaneurysm rupture, including: 1) sudden increase in the intensity of pain over the rupture site, and 2) sudden enlargement of the swelling.
Failed seal-off was defined when the hematoma continued expanding and kept enlarging in size after the seal-off procedure (Fig. 3).
Clinical success was defined when a salvaged access could be cannulated for at least one successful hemodialysis session after the seal-off procedure (8).
Patency rates were reported, according to the published reporting standards (8, 9) with modifications.
1) Post-seal-off functional primary patency was defined as the interval from the time when an access was cannulated for hemodialysis after the seal-off treatment to any re-intervention (endovascular or surgical revision) designed to maintain or reestablish patency, access thrombosis, or the time of measurement of patency. The time of the measurement of patency is the point in time when the observation or censoring of an access is performed. Elective revision procedures, such as aneurysmorrhaphy or endoprosthesis, performed for the treatment of delayed pseudoaneurysm was considered events in a survival analysis.
2) Post-seal-off functional secondary patency was defined as the interval from the time when the access was cannulated for hemodialysis after the seal-off treatment to the access abandonment or time of measurement of the patency.
Patency rates estimates were calculated with the Kaplan-Meier analysis. We tested the frequency of failed seal-off procedures and the occurrence of acute pseudoaneurysms for the superficial and deep ruptures, using the Fisher's exact test. Statistical analyses were performed using commercially available statistical software (version 15.0; SPSS, Chicago, IL, USA).
Table 1 lists a summary of the results from this study.
There were 20 grade 3 ruptures (20/1588 = 1.3%), which occurred in 20 patients (5 male and 15 female; mean age 73.0 ± 2.3 years). These vascular accesses included 16 autogenous fistulas (radiocephalic, n = 12; brachiocephalic, n = 4) and 4 prosthetic grafts (forearm loop, n = 1; upper arm straight, n = 3). The accesses were referred for treatment because of 1) immature access with or without thrombosis, n = 6; 2) acute access thrombosis, n = 4; 3) resurrection of mummy accesses (10), n = 2; and 4) access dysfunction with 1) low intra-access flow, n = 3; 2) high intra-access pressure, n = 3; or 3) difficult cannulation, n = 2. The causes of the grade 3 rupture were: 1) balloon dilatation related, n = 18; 2) thrombo-aspiration related, n = 1; or 3) sheath insertion related, n = 1. The number of attempts to inject the NBCA mixture ranged from 1-4 injections with the following rates: one injection = 40.0%, two injections = 40.0%, three injections = 15.0% and four injections = 5.0%. The average amount of NBCA mixture used was 3.71 ± 0.73 mL (range: 2.0 mL to 6.0 mL).
The rupture sites were further divided into 1) superficial ruptures and 2) deep ruptures. The superficial ruptures included those in a) the swing segment of the forearm fistula, n = 9; b) the arterial cannulation segment of the forearm fistula, n = 3; and c) the arteriovenous anastomosis, n = 1. The deep ruptures included those in a) the graft-axillary venous anastomosis, n = 2; b) the cephalic arch, n = 3; and c) the axillary vein, n = 2. Failed seal-offs and acute pseudoaneurysms occurred significantly more frequently in deep ruptures than in the superficial lesions (p = 0.032 < 0.05). A quarter-note sign was identified in all grade 3 ruptures, in this study.
The technical success was 90.0% (18/20). Technical failure occurred in two patients (no. 5 and no. 7), one was salvaged with a bailout stent-graft insertion, and the other access was abandoned by coils embolization at the arteriovenous anastomosis (Fig. 3). No glue mixture-catheter adhesion was noticed during deflation and withdrawal of the balloon catheter immediately after the seal-off procedure. Two acute pseudoaneurysms (no. 8 and no. 15) were noted immediately after the seal-off procedures: one pseudoaneurysm remained stable in size after the seal-off for 3 days. Because the patient was afraid of pseudoaneurysm rupture, the lesion was electively corrected by insertion of a stent-graft. The other access was lost because the patient could not afford a stent-graft, and the vascular surgeon in another hospital recommended an access ligation procedure, which was performed 12 days after the seal-off. A breakdown diagram for the grade 3 ruptures is shown in Figure 5. The clinical success was 94.4% (17/18). Of the 18 salvaged vascular accesses, 7 accesses (7/18 = 38.9%) were not cannulated for hemodialysis in the following session of hemodialysis because there was swelling of the cannulation sites (n = 6) and immature access (n = 1). These seven patients were dialyzed via double lumen catheters, which were indwelled for the mean of 17.3 ± 6.7 days (ranged from 7-29 days). The other eleven accesses (11/18 = 61.1%) were available for hemodialysis soon after the seal-off, and no temporary catheterization was needed. The case no. 10 failed to achieve clinical success because a pseudoaneurysm developed in one week and the access was ligated before the double lumen catheter being able to be removed.
The post seal-off functional primary patency was 77.8 ± 9.8% at 30 days, 66.7 ± 11.1% at 90 days, 33.3 ± 11.1% at 180 days, and 13.3 ± 8.5% at 360 days. The secondary functional patency was 94.4 ± 5.4% at 90 days, and 83.3 ± 8.8% at 180, 63.3 ± 12.1% at 360, and 50.6.0 ± 14.9% at 720 days. The mean post seal-off functional primary and secondary patency rates were 168.0 ± 41.6 days and 566.2 ± 77.8 days, respectively. A total of 37 interventions, including 4 surgical revisions and 33 angioplasties were required in 12 patients to maintain the access sites' patency.
Most of the complications were considered minor and required only conservative treatment. Extremity swelling, pain, ecchymosis, focal hump of varying sizes at the seal-off site occurred in all patients. Four patients (4 / 20 = 20.0%) reported local heat sensation over the seal-off sites. Discharge of old blood, mixed with fragments of glue cast from the needle wounds, were noted in three patients (3 / 20 = 15.0%), and all of these patients developed pseudoaneurysms during the follow-up. One complication was categorized as major (11) in a patient (case no. 6) who required a blood transfusion after the access-salvage procedure. In this patient, a grade 3 rupture occurred at the cephalic arch, which was successfully sealed-off and the access was salvaged. The patient stayed in the emergency department for one night and was then discharged. However, the major complication was not imputable to the seal-off technique, but to the access salvage procedure. Delayed pseudoaneurysms developed in seven of the salvaged accesses (7 / 18 = 38.9%) during the follow-up. For the eight pseudoaneurysms (one acute and seven delayed ones) during the follow-up, three were managed by observation only, three had surgical ligation of access at another hospital, and two had surgical revisions (aneurysmorrhaphy or graft interposition).
The incidence of venous rupture was 2.0% to 6.4% in access-related angioplasty procedures. Typically, for a patent vascular access, the rupture was initially managed by prolonged balloon tamponade with the same size angioplasty balloon used before the rupture occurred. Although the balloon tamponade is commonly used to manage angioplasty-induced venous injuries, there are no published descriptions of this technique or its results (6). Despite the lack of clinical data, balloon tamponade is generally considered to be more effective than the manual compression.
When an extravasation cannot be stopped by repeated and prolonged balloon tamponade, it is considered as a grade 3 rupture. Currently, no reports have examined the sonographic findings of the grade 3 ruptures. Beathard (7) classified grade 3 hematomas as having a complete or nearly complete dehiscence of the vascular wall. We identified a vascular wall "quarter note sign" in the axial sonographic scans of all a grade 3 rupture we examined. Each wall defect was continuous with a fistulous tract (note-stem), and eventually, to a localized hematoma (note-head). These wall defects represent a complete dehiscence of the vascular wall, confirming the Beathard's postulation.
In the study, based on our definition, we calculated the grade 3 rupture rates, which was estimated in the published literature to be approximately 1.4 ± 0.5%, ranging from 0.8-2% (4, 5, 12-14). The grade 3 rupture rate in our study was 1.3%, which was comparable to the reported series.
Beathard (7) recommended that as soon as a grade 3 hematoma was recognized, the access should be occluded. However, Turmel-Rodrigues et al. (15) stated that a loss of vascular access, following the uncontrolled vessel rupture, has become extremely rare with the availability of stents. Kornfield reported 22 failed treatments for the access ruptures. Of them, if the access continued bleeding, despite all efforts (manual compression, balloon tamponade and bare metal stent insertion), except stent-grafting, they allowed deliberate access occlusion in 9 cases and access re-thrombose in 2 cases. Turmel-Rodrigues et al. (14) reported a case with a major rupture, which failed to be controlled by three 10-minute cycles of low-pressure balloon tamponade. They inserted an 8-mm covered stent in a 5-mm vein because there was no appropriately sized stent available at that time. We encountered a similar situation in one case (case no. 15), but instead of inserting a stent of an inappropriate size, we controlled the expanding hematoma to an acute pseudoaneurysm with the seal-off procedure and inserted a stent-graft 3 days later, when a suitably sized stent-graft was available. Dale et al. (5) successfully treated 21 angioplasty-related ruptures with expanded polytetrafluoroethylene covered stents, of which, 2 were the grade 3 ruptures. No delayed bleeding or pseudoaneurysm was noted during the follow-up. The covered stent seems to be a reliable treatment for the grade 3 ruptures. However, the covered/uncovered stents are expensive and is not insurable in our country. Therefore, endoprosthesis is usually not a treatment option for the grade 3 ruptures because most of our patients cannot afford it. The other reason for not inserting a stent occurs when there is no stent of a proper size available during the procedure.
For the grade 3 ruptures, all accesses will be lost if endoprosthesis is not performed. Our data demonstrate that 90.0% of vascular accesses were salvaged, using the technique. However, there were eight pseudoaneurysms noted during the follow-up, including one untreated acute pseudoaneurysms and seven delayed ones. Only one clinical failure was noted; the rest of seven vascular accesses remained functioning for hemodialysis, at an average of 411.0 days (ranged from 12-844 days). However, the seal-off technique seemed to be not as durable a treatment as endoprosthesis, and delayed pseudoaneurysms appeared 100% in 6 weeks and 71.4% in 4 weeks. For three of the eight pseudoaneurysms, vascular surgeons decided to treat with the access ligations; however, we thought they would have been salvageable if a stent/stent-graft had been inserted or a revision surgery had been done at that time. Our results suggest that the seal-off technique is effective to control the grade 3 ruptures on the scene, but its effectiveness is only durable for one to two months. Nevertheless, once pseudoaneurysms were noted, depending on the patients' affordability and the availability of the stent/stent-graft, they could be electively corrected with endoprosthesis or the revision surgery.
In this study, the post seal-off functional primary patency was 33.3 ± 1% at 180 days and 13.3 ± 8.5% at 360 days, and the post seal-off functional secondary patency was 83.3 ± 8.8% at 180 days and 63.3 ± 12.1% at 360 days. The follow-up interval ranged from 12 to 844 days. For salvage of acutely thrombosed fistulas, the reported post-intervention primary and secondary patency rates could be as high as 28% to 81% and 44% to 84%, respectively, at 180 days, and as high as 50 to 70% and 70 to 80%, respectively, at 360 days (16, 17). In the current study, at 360 days, the primary patency was much inferior and the secondary patency was slightly inferior to the reported data, which were probably due to a high incidence of post-procedural pseudoaneurysms, requiring subsequent endovascular/surgical revisions or vascular access ligation.
The effectiveness of NBCA, as a tissue adhesive is dependent on the proper application technique. Unlike the previously reported surgical cases (18) or animal studies (19), we could not directly visualize the rupture site and examine its extent, nor could we hold the torn vascular edges together with a proper apposition, while the NBCA was being applied. Therefore, our technical success was not 100%. This finding was not surprising because for deeper ruptures in the axillary region, it was more difficult to identify the rupture site, and precisely insert the needle into the "note-stem" than for the superficial ruptures. Moreover, when advancing a needle in the axillary region, care should be taken to avoid inadvertent injury of the brachial plexus and vessels. Therefore, the needle entry site and its trajectory tract were limited. If the glue mixture could not be applied thoroughly over the rupture site, an acute pseudoaneurysm or even an expanding hematoma would occur.
The implications of this study are as follows: 1) without endoprosthesis, vascular access loss can be avoided by performing the glue seal-off procedure, which is effective for the grade 3 ruptures and preservation of access function; 2) even though an acute or delayed pseudoaneurysm can occur, after the seal-off, most of the treated vascular accesses could resume their function after extremity swelling or pain subsided; and finally, 3) the seal-off technique allows the interventionalist to give patients and their family time to make a decision on how to treat the pseudoaneurysm with access ligation, endoprosthesis, or surgical revision. The limitations of this study are as follows: 1) the retrospective design of the study; 2) the operator's skill for ultrasound-guided needle intervention is the key for high technical success, and the variance it would pose with different operators, 3) the technique was not performed for arterial rupture because no such case was noted in the current series; and 4) the study only evaluated a NBCA mixture with a lipiodol/NBCA ratio = 1/3. No NBCA mixture with other lipiodol/NBCA ratios was evaluated.
The NBCA seal-off technique is effective to control the grade 3 ruptures on the scene with both high technical and clinical success rates. However, the treatment is not as durable as endoprosthesis and about 40% of the completely sealed off accesses developed delayed pseudoaneurysms in 2-month of the follow-up.
Figures and Tables
Fig. 1
Sonographic appearances of grade 3 ruptues.
A. Axial sonographic scan of rupture site in case no. 14, demonstrating typical quarter-note sign. Grade 3 rupture occurred inadvertently during declotting procedure when 8 Fr guiding catheter perforated vascular wall at swing segment of autogenous radiocephalic fistula. Balloon (white arrow) was inflated to tamponade rupture site (white arrowhead), and from this location, long fistulous tract (note-stem, white arrowheads) was noted to be continuous with focal hematoma (asterisk, note-head). B. Axial sonographic scan of rupture site in case no. 12, demonstrating quarter-note sign with short note-stem (white arrow) and focal hematoma (asterisk) mimicking teardrop. C. Immediately after 18G needle sheath (arrowheads) was advanced into rupture site, axial sonographic scan was obtained in case no. 14. Tip of needle sheath was positioned abutting inflated balloon (asterisk).

Fig. 2
Digital subtraction venography obtained immediately after seal-off procedure in case no. 15. Three injections with three 18G percutaneous transhepatic cholangiography needles (arrows) were attempted, and grade 3 rupture was controlled as acute pseudoaneurysm (arrowheads). Unwanted glue mixture infiltration along interstitial planes in adjacent soft tissue was noted (asterisks), and rupture site was severely obscured by glue cast under sonogram. We, therefore, stopped seal-off procedure. Patient came back three days later and decided to insert stent-graft for acute pseudoaneurysm. Access was followed-up for 174 days and was uneventful until end of this study.

Fig. 3
Fistulography obtained immediately after failed seal-off procedure in case no. 5. Glue cast was noted abutting swing segment of autogenous radiocephalic fistula. Extensive contrast medium extravasation (asterisk) and soft tissue swelling (arrowheads) were noted after seal-off procedure. Access was intentionally thrombosed by placing colis at arteriovenous anastomosis (white arrow). Because there were no available veins for further vascular access placement, patient was referred for peritoneal dialysis.
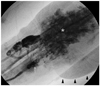
Fig. 4
Roadmap image obtained immediately after seal-off procedure in case no. 18. Single injection with 18G needle sheath (arrowheads) was performed to achieve complete seal-off. Glue cast (asterisk) was noted abutting swing segment of autogenous radiocephalic fistula. No residual extravasation or acute pseudoaneurysm was noted at rupture site (arrowhead). Access was followed-up for 42 days and was uneventful until end of this study.

References
1. Pappas JN, Vesely TM. Vascular rupture during angioplasty of hemodialysis raft-related stenoses. J Vasc Access. 2002. 3:120–126.
2. Kim DH, Goo DE, Yang SB, Moon C, Choi DL. Endovascular management of immediate procedure-related complications of failed hemodialysis access recanalization. Korean J Radiol. 2005. 6:185–195.
3. Funaki B, Szymski GX, Leef JA, Rosenblum JD, Burke R, Hackworth CA. Wallstent deployment to salvage dialysis graft thrombolysis complicated by venous rupture: early and intermediate results. AJR Am J Roentgenol. 1997. 169:1435–1437.
4. Rundback JH, Leonardo RF, Poplausky MR, Rozenblit G. Venous rupture complicating hemodialysis access angioplasty: percutaneous treatment and outcomes in seven patients. AJR Am J Roentgenol. 1998. 171:1081–1084.
5. Dale JD, Dolmatch BL, Duch JM, Winder R, Davidson IJ. Expanded polytetrafluoroethylene-covered stent treatment of angioplasty-related extravasation during hemodialysis access intervention: technical and 180-day patency. J Vasc Interv Radiol. 2010. 21:322–326.
6. Vesely TM. Role of stents and stent grafts in management of hemodialysis access complications. Semin Vasc Surg. 2007. 20:175–183.
7. Beathard GA. Management of complications of endovascular dialysis access procedures. Semin Dial. 2003. 16:309–313.
8. Gray RJ, Sacks D, Martin LG, Trerotola SO. Society of Interventional Radiology Technology Assessment Committee. Reporting standards for percutaneous interventions in dialysis access. J Vasc Interv Radiol. 2003. 14(9 Pt 2):S433–S442.
9. Sidawy AN, Gray R, Besarab A, Henry M, Ascher E, Silva M Jr, et al. Recommended standards for reports dealing with arteriovenous hemodialysis accesses. J Vasc Surg. 2002. 35:603–610.
10. Weng MJ, Chen MC, Chi WC, Liu YC, Liang HL, Pan HB. Endovascular revascularization of chronically thrombosed arteriovenous fistulas and grafts for hemodialysis: a retrospective study in 15 patients with 18 access sites. Cardiovasc Intervent Radiol. 2011. 34:319–330.
11. Sacks D, Marinelli DL, Martin LG, Spies JB. Society of Interventional Radiology Technology Assessment Committee. Reporting standards for clinical evaluation of new peripheral arterial revascularization devices. J Vasc Interv Radiol. 2003. 14(9 Pt 2):S395–S404.
12. Kornfield ZN, Kwak A, Soulen MC, Patel AA, Kobrin SM, Cohen RM, et al. Incidence and management of percutaneous transluminal angioplasty-induced venous rupture in the "fistula first" era. J Vasc Interv Radiol. 2009. 20:744–751.
13. Turmel-Rodrigues L, Pengloan J, Baudin S, Testou D, Abaza M, Dahdah G, et al. Treatment of stenosis and thrombosis in haemodialysis fistulas and grafts by interventional radiology. Nephrol Dial Transplant. 2000. 15:2029–2036.
14. Turmel-Rodrigues L, Pengloan J, Rodrigue H, Brillet G, Lataste A, Pierre D, et al. Treatment of failed native arteriovenous fistulae for hemodialysis by interventional radiology. Kidney Int. 2000. 57:1124–1140.
15. Turmel-Rodrigues L, Pengloan J, Bourquelot P. Interventional radiology in hemodialysis fistulae and grafts: a multidisciplinary approach. Cardiovasc Intervent Radiol. 2002. 25:3–16.
16. Rajan DK, Clark TW, Simons ME, Kachura JR, Sniderman K. Procedural success and patency after percutaneous treatment of thrombosed autogenous arteriovenous dialysis fistulas. J Vasc Interv Radiol. 2002. 13:1211–1218.
17. Liang HL, Pan HB, Chung HM, Ger LP, Fang HC, Wu TH, et al. Restoration of thrombosed Brescia-Cimino dialysis fistulas by using percutaneous transluminal angioplasty. Radiology. 2002. 223:339–344.
18. Requejo F, Schumacher M, van Velthoven V. Coating the wall of an injured intracranial carotid artery during tumor removal with n-butyl-2-cyanoacrylate: technical case report. Neurosurgery. 2006. 59:4 Suppl 2. ONSE484–ONSE485. discussion ONSE485.
19. Sheikh BY. Efficacy of acrylate tissue adhesive as vascular repair and hemostatic material. Ann Vasc Surg. 2007. 21:56–60.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download