Abstract
Objective
Materials and Methods
Results
Figures and Tables
 | Fig. 1Findings of bone positron emission tomography (PET) and bone scan in 84-year-old male prostate cancer patient (no.2 in Table 1) with numerous bone metastatic lesions.
A. Anterior and posterior planar images of bone scan show multiple bone metastases. B. Bone PET anterior and posterior maximum-intensity projection images reveal numerous metasatic bone leisons. Please note that metastatic lesions on bone PET are more prominent than those on bone scan.
|
 | Fig. 2Case demonstration showing higher specificity of bone positron emission tomography (PET) than bone scan in 77-year-old male patient with colon cancer (no.14 in Table 1). He has been complaining of intractable back pain.
A. Bone scan shows focally increased uptake at L4 vertebral body (black arrows), which was suspected of bone metastasis. B. Bone PET maximum-intensity projection images also revealed hot uptake at same location (black arrows). C. Trans-axial images of CT, bone PET, and fusion image (from left to right) clearly demonstrate that osteophyte at L4 has intense uptake of Na18F (white arrow). It is noteworthy that tomographic images (C) play decisive role in determining nature of osteophyte.
|
 | Fig. 3Case demonstration showing higher sensitivity of bone positron emission tomography (PET) than bone scan in 44-year-old female patient with breast cancer (no.3 in Table 1).
A. Anterior and posterior bone scan images show only 3 abnormal foci in skull (arrowheads). B. Skull lesions observed in bone scan are found to be more prominent in bone PET (arrowheads) (top, posterior maximum-intensity projection [MIP]; middle, right lateral MIP; and bottom, left lateral MIP images). In addition, many other bone metastatic lesions are found in skull, lumbar spines, sacrum, pelvic bones, and left femur.
|
 | Fig. 4Case demonstration showing false positivity of bone positron emission tomography (PET) and bone scan in 39-year-old male patient with thyroid cancer (no.9 in Table 1).
A. (left, bone scan posterior planar; middle, bone PET posterior maximum-intensity projection [MIP]; and right, 18F-FDG PET posterior image) Bone scan and bone PET revealed abnormal uptake in left 7th rib posterior arc (black arrows); however, 18F-FDG PET was negative in left 7th rib area. B. (left, CT; middle, fusion of bone PET/CT; and right, fusion of 18F-FDG PET/CT) CT revealed osteosclerotic lesion in left 7th rib posterior arc, which was compatible with hot uptake in bone PET/CT; however, lesion was negative in 18F-FDG PET/CT (white arrows). C. Posterior image of 131I whole body scan obtained 2 days after administration of 131I (30 mCi). No lesion was found in left 7th rib area.
|
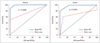 | Fig. 5
Receiver operating characteristic curve analyses. Bone positron emission tomography (PET) was significantly more accurate than bone scan in patient (p = 0.0306) and lesion (p = 0.0001) based analyses. |
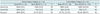
Table 1
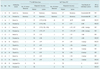
Note.-Gold standard for BM was either presence of typical findings compatible with BM in at least 2 imaging studies among MRI, 18F-FDG PET/CT, or 131I whole body scan, or presence of clinical progression causing change of treatment plan during at least one-year follow-up. BM = bone metastasis, TP = true positive, TN = true negative, FP = false positive, FN = false negative, PET = positron emission tomography
Notes
This study was supported in part by a grant of the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (A111627-1101-0000100), and by grants from the National Research Foundation (NRF), Ministry of Education, Science and Technology (MEST), (2012M2B2A9A02029612 and Basic Science Research Program 2012R1A1A2001060), Republic of Korea.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download