Abstract
Objective
We investigated the clinical significance of incidental diffuse thyroid uptake (DTU) on 18F-FDG PET in subjects without a history of cancer.
Materials and Methods
This study included 2062 studies from adults who underwent 18F-FDG PET as a cancer screening program. Subjects were divided into the following two groups: with (group I) or without (group II) DTU. The presence of DTU and the thyroid visual grading score were compared with thyroid function tests, serum anti-microsomal antibody (AMA) levels, and the presence of diffuse parenchymal change (DPC) on ultrasonography (USG).
Results
DTU was found in 6.6% of the scans (137/2062). Serum thyroid stimulating hormone (TSH) and AMA levels were significantly higher in group I than in group II. Increased AMA level (55.1%) and DPC (48.7%) were more frequently found in group I (p < 0.001). The proportion of subjects with any abnormal results in serum free thyroxine, triiodothyronine, TSH, or AMA levels or DPC on USG was significantly higher in group I than in group II (71.5% vs. 10.6%, p < 0.001), and was significantly and gradually increased according to the visual grading score group (0 vs. 1-2 vs. 3-4 = 10.6% vs. 58.5% vs. 90.9%, p < 0.001). TSH and is AMA levels were significantly increased according to the visual grading score.
18F-Fluorodeoxyglucose (18F-FDG) positron emission tomography (PET) has been used for cancer screening in healthy subjects as well as for the diagnosis, staging, and assessment of treatment response in various cancers given that most malignant tumors are 18F-FDG-avid with increased glucose metabolism (1-4). Since 18F-FDG PET for oncologic purposes usually covers the entire body or torso (base of the skull to mid-thigh), clinically unexpected, incidental hypermetabolic lesions are frequently found. For example, previous studies have reported incidental uptake in secondary primary cancer in cancer patients at the time of initial tumor staging (5), primary parotid tumor (6), or thyroid gland (7-18).
Incidental thyroid uptake on PET is classified into two categories: focal or diffuse thyroid uptake (DTU). According to previous reports, focal thyroid uptake has been detected in 1-4% of cases and is reportedly associated with malignancy in 20-50% of cases (7-11). There were several studies regarding DTU on PET or PET/computed tomography (CT) that reported incidences ranging from 0.6% to 3.5% (12-17). Some studies have reported that DTU can be a normal variant, while several previous reports demonstrated that diffuse thyroid FDG uptake could be an indicator of benign thyroid disease and related to Hashimoto's thyroiditis. Chen et al. (15) reported that diffuse thyroid 18F-FDG uptake most likely represents chronic thyroiditis. Karantanis et al. (16) also reported that increased 18F-FDG uptake in the thyroid gland is associated with chronic lymphocytic thyroiditis. However, these studies involved small numbers of subjects, and there was a possibility of selection bias given that further diagnostic work-up, including in vitro thyroid function tests (TFT) and neck ultrasonography (USG), was only performed in patients with increased thyroid uptake. In other words, we cannot be certain that an absence of significant thyroid uptake excludes the possibility of abnormalities in the thyroid gland. Therefore, the clinical significance of DTU on PET remains unclear.
We retrospectively investigated the clinical significance of incidental DTU in subjects without prior history of cancer and thyroid disease by comparing the results of 18F-FDG PET and the results of in vitro TFT, serum anti-microsomal antibody (AMA) levels, and/or neck USG that were all acquired on the same day as part of a general health examination.
Between January 2007 and May 2008, there were 2204 studies from adults who underwent 18F-FDG PET or PET/CT scan for cancer screening as part of a general health examination that included TFT, serum AMA, and/or USG. All subjects voluntarily selected the tests and imaging for the general health examination after obtaining information and explanations for each exam including potential benefits, radiation exposure and costs. All tests and imaging were performed on the same day. Among the potential studies, we excluded 34 cases with focal thyroid 18F-FDG uptake without diffuse uptake and 108 scans from subjects with a previous history of thyroid disease, other malignancy, or both. Ultimately, 2062 studies from 1917 adult subjects without history of previous malignancy or thyroid disease (1787 males, 275 females; mean age: 51.4 ± 6.7 years, range: 24-82 years) were included for analysis. All subjects underwent in vitro TFT including total triiodothyronine (T3), free thyroxine (FT4) and thyroid stimulating hormone (TSH), and serum AMA. Among the subjects, 1679 (81.4%) underwent neck USG as part of the general health examination. The ethics committee of our institution approved the study protocol for this retrospective cross-sectional study.
18F-FDG PET was performed using a dedicated PET scanner (Advance, GE Healthcare, Milwaukee, WI, USA) or a PET/CT scanner (Discovery LS, GE Healthcare, Milwaukee, WI, USA). All patients fasted for at least 6 hours before the PET study. Blood glucose levels were measured and were required to be less than 200 mg/dL before 18F-FDG injection. Emission images (5 minute/bed) were obtained 45 minute after intravenous administration of 370 MBq 18F-FDG in the two-dimensional acquisition mode from the base of the skull to the mid-thigh. A post-emission transmission scan with 68Ge rods or a non-contrast CT scan (140 KeV, 40 to 100 mAs) was used for attenuation correction. PET data were reconstructed on a 128 × 128 matrix, using the iterative ordered subsets expectation maximization algorithm. CT and FDG-PET scan data were accurately coregistered using commercial software (Xeleris, GE Healthcare, Milwaukee, WI, USA).
All laboratory tests were performed at our institution. Serum FT4 and T3 were measured with an automated, competitive radioimmunoassay (IMMUNOTECH, Prague, Czech). Serum TSH was measured using a two-site immunoradiometric sandwich assay (IMMUNOTECH, Prague, Czech). The serum AMA screen was performed using an automated, competitive, radioimmunoassay (BRAHMS, Berlin, Germany).
The reference ranges for these laboratory tests at our institution were 76-198 ng/dL for T3, 0.88-1.56 ng/dL for FT4, and 0.3-6.5 µIU/mL for TSH. The results of serum AMA were considered positive at a serum dilution of 1 : 100 or higher.
Ultrasonography of the neck used an HDI 5000 (Advanced Technology Laboratories, Bothell, WA, USA), IU22 (Philips Medical Systems, Bothell, WA, USA), or LOGIQ 700 ultrasound scanner (GE Medical Systems, Milwaukee, WI, USA) equipped with a 5-12 MHz linear-array transducer. Board-certified radiologists with at least 5 years of experience in thyroid US performed all of the sonographic examinations.
When thyroid parenchyma was shown to be heterogeneous and coarsened, or diffusely hypoechoic, the radiologists interpreted this as the presence of diffuse parenchymal change (DPC) on USG.
Two nuclear medicine physicians provided a consensus interpretation of the PET images. Subjects were divided into the following two groups: with (group I) or without (group II) DTU. DTU was defined as the presence of 18F-FDG uptake in the whole thyroid gland greater than cervical background activity. The degree of 18F-FDG uptake in each lobe of the thyroid was determined using the following five-point visual grading system: grade 0, similar to cervical background activity; grade 1, thyroid uptake greater than cervical background activity, but less than mediastinal blood pool activity; grade 2, uptake similar to or greater than mediastinal blood pool activity, but less than liver activity; grade 3, uptake similar to liver activity; and grade 4, uptake greater than liver activity (Fig. 1). The higher grade in the bilateral lobes was considered as a representative visual grading score for each subject. The difference in the grade between each thyroid lobe was less than two grades in all patients. Using the visual grading score, subjects with a grading score of 1 or greater than 1 belonged to group I. The remaining subjects with a grade score of 0 belonged to group II. In addition, subjects were divided into 3 groups according to the visual grading score for evaluating the correlations with other tests; 0, 1-2, vs. 3-4.
The thyroid function statuses were divided based on in vitro TFT. Hypothyroidism was diagnosed on the basis of a low level of serum FT4 or T3, and a high level of TSH. Hyperthyroidism was diagnosed in subjects with a high level of serum T4 or T3, and a low level of TSH. Subclinical hypothyroidism was diagnosed in subjects with a high level of TSH and a normal level of FT4 and T3. Subclinical hyperthyroidism was diagnosed in subjects with a low level of TSH and a normal level of FT4 and T3. The results of in vitro TFT, AMA levels, and neck USG and the thyroid function status were compared with the presence of DTU and the 18F-FDG uptake score.
Clinical characteristics and the results of the TFT, AMA levels, and USG between group I and group II were analyzed by Student's t test or Pearson's chi-square test. Visual thyroid uptake scores according to the thyroid functional status and TFT and AMA levels according to the visual uptake score group were compared using ANOVA with post hoc LSD tests. A commercial software package (PASW Statistics 18, SPSS Inc., Chicago, IL, USA) was used for all of the analyses, and p-values of < 0.05 were considered statistically significant. Data were expressed as mean ± standard deviation.
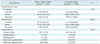
The characteristics of each group were described in Table 1. Among all 2062 scans, diffuse thyroid 18F-FDG uptake was found in 137 (group I; incidence, 6.6%). The proportion of female subjects was significantly higher in group I than in group II. The percentage of subjects with DTU in the female group was 16.0% and 5.2% in the male group, which was significantly different (p < 0.001).
Serum TSH and AMA levels were significantly higher in group I than in group II (p < 0.001). An elevated AMA level (55.5% vs. 3.3%, p < 0.001) and DPC on USG were more frequently observed in group I than in group II (48.7% vs. 3.9%, p < 0.001). The FT4 level was slightly lower in group I than in group II (p < 0.05). The T3 level was not statistically different between the two groups. The proportion of subjects with any abnormal results in serum FT4, T3, TSH, or AMA levels or with DPC on USG was significantly higher in group I than in group II (71.5% vs. 10.6%, p < 0.001). Among group I subjects who had any abnormal results in serum FT4, T3, TSH, or AMA levels or DPC on USG, 49.0% (48/98) had two or more abnormal findings. The remaining 50 subjects had only one abnormal finding. In contrast, among group II subjects with any abnormal results in serum FT4, T3, TSH, or AMA levels or DPC on USG, 89.7% (183/204) had only one abnormal finding, including one abnormal TFT result in 94 subjects, an increased AMA level in 50, and DPC on USG in 39. The remaining 21 subjects had two or more abnormal findings. Also, the AMA levels of group I subjects with elevated AMA were significantly higher than those of group II subjects with elevated AMA (2922.4 ± 6402.6 vs. 53.9 ± 459.2, p < 0.001). In addition, there were no significant differences in abnormal TFT, AMA levels, or DPC on USG between female and male subjects in group I.
The analysis of thyroid functional status revealed that 1918 scans (93.0%) had euthyroid status, 9 (0.4%) had hyperthyroidism, 19 (0.9%) had hypothyroidism, 14 (0.7%) had subclinical hyperthyroidism, and 102 (5.0%) had subclinical hypothyroidism. Abnormal thyroid function was more frequently observed in group I (26.3% vs. 5.6%, p < 0.001). The most common thyroid disease in group I was subclinical hypothyroidism (83.3%). In group I, subclinical hyperthyroidism, hypothyroidism, and hyperthyroidism all exhibited the same prevalence of 5.6% (Table 2).
To evaluate the thyroid functional status according to the combination of DTU on PET and DPC on USG, subjects were divided into 4 groups; neither DTU nor DPC, presence of DPC without DTU, presence of DTU without DPC and presence of both DTU and DPC. In regard to the results, the thyroid functional status was significantly different between the groups (Table 3). In the group with both DTU and DPC, a significantly lower FT4 level, higher TSH and AMA levels, and higher prevalence of subclinical hypothyroidism were observed than in the other groups. In the group without DTU or DPC, significantly lower TSH and AMA levels, and a higher prevalence of euthyroid status were observed than in the other groups.
On visual grading analysis, the mean uptake score was 0.16 ± 0.65. There were significant differences in the visual grading score according to the functional status of the thyroid (p < 0.001, Fig. 2). Post hoc LSD testing showed significantly higher uptake parameters in the subclinical hypothyroidism group than in the euthyroid, hypothyroidism, and subclinical hyperthyroidism groups. When subjects were divided into three groups according to the visual grading score (0 vs. 1-2 vs. 3-4), the proportion of abnormal TFT results (5.6% vs. 18.3% vs. 38.2%, respectively) or elevated AMA levels (3.3% vs. 43.9% vs. 72.7%, respectively) was significantly increased according to the visual grading score (p < 0.001). There were significant differences in FT4, TSH, and AMA levels (p < 0.001) according to visual grading score group; however, there were no significant differences in T3 levels (Fig. 3). More specifically, FT4 was significantly decreased according to the visual grading score while TSH and AMA levels were significantly increased according to the visual grading score. Post hoc LSD tests showed that the subgroup with a visual grading score of 3-4 had significantly higher TSH and AMA levels and lower FT4 levels compared to both of the other subgroups. The subgroup with a visual grading score of 0 had significantly lower TSH and AMA levels than the other two subgroups (Fig. 2). The proportion of subjects with any abnormal results in serum FT4, T3, TSH, or AMA levels or DPC on USG was significantly and gradually increased according to the visual grading score group (0 vs. 1-2 vs. 3-4 = 10.6% vs. 58.5% vs. 90.9%, p < 0.001).
Representative cases of subjects with DTU and without DTU are illustrated in Figure 1. A PET image of a 54-year-old male patient revealed no definite 18F-FDG uptake in the thyroid gland (Fig. 1A). The visual grading score was 0 and the AMA level was normal (1 U/mL). Thyroid function status was euthyroid (T3, 157 ng/dL; FT4, 1.11 ng/dL; TSH, 0.67 µIU/mL). The next PET image of a 54-year-old male patient demonstrated mildly increased FDG uptake in the thyroid gland (Fig. 1B). The visual grading score was 2 and the AMA level was 196 U/mL. Thyroid function status was euthyroid (T3, 101 ng/dL; FT4, 1.17 ng/dL; TSH, 1.82 µIU/mL). On the other hand, PET image of a 54-year-old male patient demonstrated diffuse 18F-FDG thyroid uptake (Fig. 1C). The visual grading score was 4 and the AMA level was 42300 U/mL. Thyroid functional status was subclinical hypothyroidism (T3, 96 ng/dL; FT4, 0.84 ng/dL; TSH, 13.97 µIU/mL).
In this study, we investigated the clinical significance of incidental DTU on 18F-FDG PET in subjects without a history of cancer. Our data revealed that the presence of DTU was closely correlated with increased serum AMA and TSH levels and the presence of DPC on USG in non-cancer subjects. In 56% of patients with DTU, the level of serum AMA was increased. In 23% of patients with DTU, the level of serum TSH was increased. The group with a combined presence of DTU and DPC had the lowest FT4 level, highest TSH and AMA levels, and the highest prevalence of subclinical hypothyroidism. These suggest that DPC may provide an additional contribution to thyroid functional abnormality and an elevated AMA level. In addition, the degree of increased thyroid uptake was significantly associated with an increase in serum AMA and TSH levels. However, T3 was not associated with DTU. There was a very small difference in FT4 between group I and II. These results suggest that further diagnostic work-ups such as a TFT and thyroid autoantibody check is necessary to rule out benign thyroid disorder such as autoimmune thyroid disease, when incidental DTU is observed in a routine interpretation of PET images, especially showing high 18F-FDG uptake.
There was a large discrepancy in the incidence of DTU between our study (6.6%) and previous PET reports (0.6-3.5%) (14, 19, 20). This is probably due to different detection rates derived from different consensuses regarding DTU. For several years, incidentally detected 18F-FDG uptake on whole-body PET/CT scans has been of interest to our group (21, 22). As such, we have made an effort to carefully review thyroid uptake encountered in routine clinical practice. The use of PET/CT might also contribute, in part, to the difference between our data and that of other studies due to the precise lesion localization and evaluation that can be achieved with PET/CT. As a consequence, we observed a relatively large number of cases with incidental thyroid uptake, and the overall intensity of thyroid uptake was lower than that of the previous reports.
There have been previous studies regarding DTU on PET or PET/CT (12-17, 23). With the exception of a few studies, the majority of previous studies evaluated non-cancer subjects in a manner similar to ours. The major aspects that differentiated our study from previous research were that we included all consecutive scans during a set period and only excluded subjects with known thyroid disease irrespective of the presence of DTU. Additionally, in our study the results of TFT and AMA were available in all subjects. In two previous reports, a control group without DTU was artificially selected (14, 16) and included subjects with known thyroid disease in the group, and comparative analyses of TFT and other tests were not performed for the group with DTU (16). Furthermore, the number of subjects was the largest in this study compared with previous studies.
In our study, 72% of subjects with DTU (group I) had an abnormal TFT, AMA level or DPC on USG, which was similar with the incidences of previous studies ranging from 59% to 100% (12-16). In contrast, 89% of subjects without DTU (group II) had no abnormal findings in serum FT4, T3, TSH, or AMA levels or DPC on USG. Most subjects in both groups had euthyroid status. In addition, the degree of the 18F-FDG visual uptake score was significantly associated with the risk of abnormal TFTs, an elevated AMA level, and serum levels of TSH and AMA. These findings suggest that the most plausible cause of DTU may be autoimmune thyroid disease, which corroborates the results of previous studies (12-17). Though subclinical hypothyroidism with autoimmune thyroiditis was the most frequently found in our study and other previous reports, other autoimmune thyroid disorders such as Graves' disease and chronic autoimmune thyroiditis may cause DTU (15, 17, 24). Additionally, the presence and degree of DTU seems to reflect the severity of thyroid cell damage caused by an autoimmune mechanism. Although there have been several studies regarding DTU on PET, the uptake mechanism of autoimmune thyroid disease still remains uncertain. In the process of chronic autoimmune thyroiditis, there is lymphocyte infiltration, inflammation, and tissue destruction (14). Activated lymphocytes within the thyroid gland affected by inflammation and autoimmune disease are reported to show intensive glycolysis (24). In a destructive step of autoimmune thyroiditis, T-helper type 1-mediated mechanisms lead to the infiltration of activated macrophages into the thyroid gland (25). Considering the results of our study and those of previous studies, we suggest that 18F-FDG uptake may be increased due to the lymphocytes and activated macrophages that have accumulated in the damaged thyroid gland as a result of an autoimmune mechanism.
In this study, only 11% of subjects without DTU and previous thyroid disease had one or more abnormal findings in serum FT4, T3, TSH, or AMA levels or DPC on USG, which is similar to a result of 8% in a previous study of 36 subjects without DTU (25). Furthermore, those subgroup subjects without DTU had significantly less severe abnormal findings on TFT and AMA levels than subjects with DTU. Therefore, we suggest that further evaluation regarding functional thyroid disease is not always necessary if subjects have no DTU on PET. In contrast, 59% of subjects with mild to moderate DTU (uptake score 1-2) had one or more abnormal findings in serum FT4, T3, TSH, or AMA levels or DPC on USG. This suggests that even mild or low-grade uptake in the thyroid should not be ignored because this uptake may be associated with overt or subclinical hypothyroidism requiring hormone therapy, which supports findings from previous studies (16, 17). Therefore, any kind of incidental DTU may require further evaluation, such as TFT and anti-thyroid antibodies with or without USG. Nevertheless, approximately 10% of subjects with severe DTU (uptake score 3-4) had normal TFT and AMA levels without DPC on USG. Although the cause of DTU in these subjects is not clear, checking a single anti-thyroid antibody instead of multiple kinds of anti-thyroid antibodies might influence the result.
In this study, we used a semiquantitative thyroid uptake score compared with reference organs instead of conventional standardized uptake value (SUV)-based methods, which demonstrated significant positive associations with TFT and AMA levels. Conversely, in another study maximum SUV of the thyroid was not significantly correlated with serum TSH or thyroperoxidase antibody levels (16). This might have resulted from the small number of subjects (about 20) and the lack of a control group. Furthermore, another possible cause is that they measured the maximum SUV which cannot fully reflect the entire thyroid gland uptake. In practice, only a moderate correlation was found when we analyzed the correlation of AMA level and maximum SUV in group I (r = 0.44, p < 0.001, unpublished data).
We found that the percentage of DTU among females was higher than in males. This is possibly related to a well-known fact that autoimmune thyroid disease occurs more frequently in women than in men. According to previous reports, hormones, especially estrogen, are thought to play an important role in women's higher risk of autoimmune disorders (26-28). Gender differences in immunity may also explain the difference in risk for autoimmune disorders. For example, women naturally have stronger inflammatory responses than men when immune reactions are generated (26-28).
Our present study had several limitations. Only subjects undergoing PET or PET/CT among populations receiving a general health examination were enrolled in this study. This might result in a significant discrepancy of the sex ratio and high incidence of office workers as an occupation, which may potentially induce a selection bias. Another possible limitation was the use of two different kinds of scanners and acquisition protocols; therefore, the SUV of thyroids could not be compared in this study. Instead, the thyroid uptake score was acquired by comparison with the uptakes of reference organs, which is a commonly used objective semiquantitative method. Moreover, it was not possible to examine the correlation of the clinical exam, such as subjects' symptoms, with the results due to the lack of relevant medical records in our health promotion center.
In conclusion, the presence of DTU in subjects without a history of cancer is closely correlated with increased AMA and TSH levels and the presence of DPC on USG. Furthermore, the degree of DTU increased according to the elevation of serum AMA and TSH levels. Therefore, the most plausible pathological cause of DTU may be thyroid cell damage caused by an autoimmune mechanism. Our results suggest that incidental DTU may deserve further diagnostic evaluation such as TFT with a thyroid autoantibody check to rule out the possibility of benign thyroid disease. Nevertheless, approximately 10% of subjects with severe DTU had normal TFT and AMA levels without DPC on USG, which warrant further investigations to find a cause.
Figures and Tables
 | Fig. 1Representative cases of visual grading score.
A. Grade 0 with euthyroid and normal serum anti-microsomal antibody (AMA) level. B. Grade 2 with euthyroid and increased serum AMA level. C. Grade 4 with subclinical hypothyroidism and elevated serum AMA level.
|
 | Fig. 2
Visual thyroid uptake score according to thyroid functional status (error bars; 95% CI for mean). CI = confidence interval |
 | Fig. 3Differences in T3, FT4, TSH, and AMA levels according to visual grading score group.
T3 (A), FT4 (B), TSH (C), and AMA (D) levels (error bars; 95% CI for mean). T3 = triiodothyronine, FT4 = free thyroxine, TSH = thyroid stimulating hormone, AMA = anti-microsomal antibody
|
References
1. Fletcher JW, Djulbegovic B, Soares HP, Siegel BA, Lowe VJ, Lyman GH, et al. Recommendations on the use of 18F-FDG PET in oncology. J Nucl Med. 2008. 49:480–508.
2. Nabi HA, Zubeldia JM. Clinical applications of (18)F-FDG in oncology. J Nucl Med Technol. 2002. 30:3–9. quiz 10-11.
3. Ko DH, Choi JY, Song YM, Lee SJ, Kim YH, Lee KH, et al. The usefulness of 18F-FDG PET as a cancer screening test. Nucl Med Mol Imaging. 2008. 42:444–450.
4. Chung JI, Cho HB, Shim JY, Choi Y, Lee KH, Kim BT, et al. Detection of cancer with PET and PET/CT in asymptomatic volunteers. Nucl Med Mol Imaging. 2009. 43:526–534.
5. Choi JY, Lee KS, Kwon OJ, Shim YM, Baek CH, Park K, et al. Improved detection of second primary cancer using integrated [18F] fluorodeoxyglucose positron emission tomography and computed tomography for initial tumor staging. J Clin Oncol. 2005. 23:7654–7659.
6. Lim I, Lee WW, Chung JH, Park SY, Kim SH, Kim YK, et al. Incidental benign parotid lesions on FDG PET: Prevalence and clinico-pathologic findings. Nucl Med Mol Imaging. 2007. 41:359–363.
7. Bae JS, Chae BJ, Park WC, Kim JS, Kim SH, Jung SS, et al. Incidental thyroid lesions detected by FDG-PET/CT: prevalence and risk of thyroid cancer. World J Surg Oncol. 2009. 7:63.
8. Choi JY, Lee KS, Kim HJ, Shim YM, Kwon OJ, Park K, et al. Focal thyroid lesions incidentally identified by integrated 18F-FDG PET/CT: clinical significance and improved characterization. J Nucl Med. 2006. 47:609–615.
9. Cohen MS, Arslan N, Dehdashti F, Doherty GM, Lairmore TC, Brunt LM, et al. Risk of malignancy in thyroid incidentalomas identified by fluorodeoxyglucose-positron emission tomography. Surgery. 2001. 130:941–946.
10. Kim TY, Kim WB, Ryu JS, Gong G, Hong SJ, Shong YK. 18F-fluorodeoxyglucose uptake in thyroid from positron emission tomogram (PET) for evaluation in cancer patients: high prevalence of malignancy in thyroid PET incidentaloma. Laryngoscope. 2005. 115:1074–1078.
11. Shie P, Cardarelli R, Sprawls K, Fulda KG, Taur A. Systematic review: prevalence of malignant incidental thyroid nodules identified on fluorine-18fluorodeoxyglucose positron emission tomography. Nucl Med Commun. 2009. 30:742–748.
12. Chen W, Parsons M, Torigian DA, Zhuang H, Alavi A. Evaluation of thyroid FDG uptake incidentally identified on FDG-PET/CT imaging. Nucl Med Commun. 2009. 30:240–244.
13. Kurata S, Ishibashi M, Hiromatsu Y, Kaida H, Miyake I, Uchida M, et al. Diffuse and diffuse-plus-focal uptake in the thyroid gland identified by using FDG-PET: prevalence of thyroid cancer and Hashimoto's thyroiditis. Ann Nucl Med. 2007. 21:325–330.
14. Yasuda S, Shohtsu A, Ide M, Takagi S, Takahashi W, Suzuki Y, et al. Chronic thyroiditis: diffuse uptake of FDG at PET. Radiology. 1998. 207:775–778.
15. Chen YK, Chen YL, Cheng RH, Yeh CL, Lee CC, Hsu CH. The significance of FDG uptake in bilateral thyroid glands. Nucl Med Commun. 2007. 28:117–122.
16. Karantanis D, Bogsrud TV, Wiseman GA, Mullan BP, Subramaniam RM, Nathan MA, et al. Clinical significance of diffusely increased 18F-FDG uptake in the thyroid gland. J Nucl Med. 2007. 48:896–901.
17. Liu Y. Clinical significance of thyroid uptake on F18-fluorodeoxyglucose positron emission tomography. Ann Nucl Med. 2009. 23:17–23.
18. Rothman IN, Middleton L, Stack BC Jr, Bartel T, Riggs AT, Bodenner DL. Incidence of diffuse FDG uptake in the thyroid of patients with hypothyroidism. Eur Arch Otorhinolaryngol. 2011. 268:1501–1504.
19. Wolf G, Aigner RM, Schaffler G, Schwarz T, Krippl P. Pathology results in [18F]fluorodeoxyglucose positron emission tomography of the thyroid gland. Nucl Med Commun. 2003. 24:1225–1230.
20. Kang KW, Kim SK, Kang HS, Lee ES, Sim JS, Lee IG, et al. Prevalence and risk of cancer of focal thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography for metastasis evaluation and cancer screening in healthy subjects. J Clin Endocrinol Metab. 2003. 88:4100–4104.
21. Cho YS, Choi JY, Lee SJ, Hyun SH, Lee JY, Choi Y, et al. Clinical significance of focal breast lesions incidentally identified by 18F-FDG PET/CT. Nucl Med Mol Imaging. 2008. 42:456–463.
22. Hyun SH, Choi JY, Lee KH, Choe YS, Kim BT. Incidental focal 18F-FDG uptake in the pituitary gland: clinical significance and differential diagnostic criteria. J Nucl Med. 2011. 52:547–550.
23. Kang BJ, O JH, Baik JH, Jung SL, Park YH, Chung SK. Incidental thyroid uptake on F-18 FDG PET/CT: correlation with ultrasonography and pathology. Ann Nucl Med. 2009. 23:729–737.
24. Boerner AR, Voth E, Theissen P, Wienhard K, Wagner R, Schicha H. Glucose metabolism of the thyroid in Graves' disease measured by F-18-fluoro-deoxyglucose positron emission tomography. Thyroid. 1998. 8:765–772.
25. Chistiakov DA. Immunogenetics of Hashimoto's thyroiditis. J Autoimmune Dis. 2005. 2:1.
26. Barbesino G, Tomer Y, Concepcion ES, Davies TF, Greenberg DA. International Consortium for the Genetics of Autoimmune Thyroid Disease. Linkage analysis of candidate genes in autoimmune thyroid disease. II. Selected gender-related genes and the X-chromosome. J Clin Endocrinol Metab. 1998. 83:3290–3295.
27. Cutolo M, Sulli A, Seriolo B, Accardo S, Masi AT. Estrogens, the immune response and autoimmunity. Clin Exp Rheumatol. 1995. 13:217–226.
28. Ahmed SA, Hissong BD, Verthelyi D, Donner K, Becker K, Karpuzoglu-Sahin E. Gender and risk of autoimmune diseases: possible role of estrogenic compounds. Environ Health Perspect. 1999. 107:Suppl 5. 681–686.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download