Abstract
We report 2 cases of complicated spontaneous dissection of the celiac artery, which were successfully treated by a stent graft. The first patient was a 47-year-old man who presented with acute abdominal pain. CT scan showed ruptured saccular aneurysm with surrounding retroperitoneal hematoma. The second patient was a 57-year-old man with progressive dissecting aneurysm. Endovascular stent graft was placed in the celiac trunk to control bleeding, and to prevent rupture in each patient. Follow-up CT scans showed complete obliteration of a dissecting aneurysm.
Spontaneous isolated dissection of visceral arteries is rare. Most of the reported cases have been associated with the superior mesenteric artery, and to our knowledge, only 25 cases of the spontaneous isolated celiac artery dissection can be found in the literature (1). Of the reported cases, only 2 cases of spontaneous celiac artery dissection had ruptured. Awareness of the visceral artery dissection is important because of its life-threatening complications causing extensive hemorrhage or ischemia to the supplied organs.
Although a review of the medical literature suggests that the natural history of spontaneous celiac artery dissection may not be fatal, it is difficult to predict. All of the following can potentially occur: spontaneous resolution, ischemia due to occlusion of the vessel, aneurysm formation, and rupture (2). The management of spontaneous celiac artery dissection includes conservative medical treatment, endovascular therapy, and surgery (1). In complicated cases, the optimal management of spontaneous celiac artery dissection remains controversial because this condition is rare. The medical literature does not provide enough information to assess the superiority of one treatment over another. Herein, we report 2 cases of the complicated spontaneous dissection of the celiac artery, both of which were successfully treated using an endovascular stent graft.
A 47-year-old man, who had presented with acute abdominal pain to a different healthcare facility, was transferred to our emergency room for further evaluation and treatment of dissection of the splanchnic arteries. The patient had a history of uncomplicated dissection of the superior mesenteric artery, and had been taking anti-hypertension medication for 1 year. However, he had stopped taking his prescription medication 10 months prior to admission to the emergency room. On arrival to the emergency room of a local hospital, his blood pressure was 95/60 mm Hg and the pulse rate was 110 beats per min. Laboratory test revealed a hemoglobin level of 10.5 g/dL. Other blood chemistry parameters were within the normal range. After blood transfusion and fluid therapy in local hospital, the patient's blood pressure had increased to 150/100 mm Hg, and there were no obvious abnormalities on the physical examination or in the laboratory findings on admission to our hospital. A contrast-enhanced CT scan showed a newly developed saccular dissecting aneurysm in the celiac artery with surrounding retroperitoneal hematoma, measuring 2.8 × 7.9 × 12.0 cm (Fig. 1A, B). The dissection of the superior mesenteric artery had not changed, compared to the previous CT scan. One day after admission, the patient's hemoglobin level had decreased to 9.6 g/dL again, after cessation of blood transfusion. The patient was offered a less invasive endovascular procedure to avoid surgical repair.
After puncturing of his right common femoral artery, an 8F guiding catheter (Vista brite tip, Cordis, Miami, FL, USA) was inserted into the orifice of the celiac artery, which allowed for celiac angiography that revealed a dissecting aneurysm at the entry point (Fig. 1C). The proximal splenic artery was occluded, and the true lumen of the left gastric artery and common hepatic artery were narrowed by intramural hematoma. We placed the 4-9 × 38 mm peripheral stent graft (Jostent, Abbott Vascular, Rangendingen, Germany), which was mounted over a 6 × 40 mm savvy balloon (Cordis, Miami, FL, USA) from the origin of the celiac artery to the common hepatic artery. Post-procedure angiography showed complete coverage of the dissecting aneurysm with the use of a stent graft (Fig. 1D). The left gastric artery was visualized by collateral flows from the right gastric artery. The postoperative course was uneventful with normalized hemoglobin level without blood transfusion. Follow-up CT scan, obtained 1 week after the procedure, showed a complete obliteration of the dissecting aneurysm in the celiac artery with preservation of the hepatic arterial flow and marked reduction of the retroperitoneal hematoma. Although occlusion of the proximal splenic artery and proximal left gastric artery after stent graft placement persisted, no abnormalities (i.e., splenic infarction, gastric ischemia, or signal of irritated peritoneum) were noted due to an abundance of collateral blood flow.
A 57-year-old man, presented with acute abdominal pain, was admitted to the emergency room. The patient had a previous medical history of spontaneous celiac artery and of the superior mesenteric artery dissection. An abdominopelvic CT scan, obtained 3 months prior to admission, demonstrated a 7 mm-sized saccular aneurysm, with a mural hematoma along the celiac artery to the common hepatic artery and a dissection of the superior mesenteric artery with a mural hematoma (Fig. 2A). Infiltration of the fat surrounding the celiac artery was noticed as a secondary sign of acute spontaneous celiac artery dissection. Other than the acute abdominal pain, the patient was healthy and had no risk factors associated with the occurrence of visceral artery dissection. He had been treated with an anticoagulant to prevent a thromboembolic complication for 3 months, because he had no major complication associated with the dissection of the celiac artery and superior mesenteric artery. The patient had no obvious abnormality on physical examination or in his laboratory findings. Vital signs were stable. Contrast enhanced CT revealed a progressive dissecting aneurysm along the celiac artery, which had a maximal inner diameter of 2 cm (Fig. 2B). The aneurysm originated 2 cm distal from celiac artery orifice without compromised distal flow to the distal hepatic artery. In addition, the patient's previous superior mesenteric artery dissection with mural thrombus had improved completely without associated complications. The patient was transferred to an interventional suite for endovascular treatment, because the risk of rupture was high, due to the progressive enlargement of an aneurysm sac. Celiac angiography, obtained after an insertion of the 8 Fr guiding catheter (Cordis), showed a dissecting aneurysm, which obviously defined the celiac artery, proximal to splenic artery and left gastric artery orifice (Fig. 2C). The involved vessel course had a relatively smooth curvature. We placed the 4-9 × 38 mm peripheral stent graft (Jostent, Abbott Vascular, Rangendingen. Germany), which was mounted over a 6 mm × 40 mm savvy balloon (Cordis) from the origin of celiac artery to the bifurcation of the common hepatic artery and the splenic artery. Post-procedure angiography showed complete exclusion of the dissecting aneurysm (Fig. 2D). There was no noticeable compromise in the blood flow to the distal hepatic artery, gastroduodenal artery, and splenic artery. The postoperative course was uneventful and the patient's symptoms abated after the procedure. The follow-up CT scan, obtained 3 months after the procedure, showed a complete disappearance of the dissecting aneurysm.
Spontaneous dissection of the celiac artery, which is not associated with aortic dissection, is extremely rare. Approximately one half of the patients with celiac artery dissection are asymptomatic, due to a good collateral flow, via the superior mesenteric artery (3). The symptoms are usually non-specific epigastric pain or post-prandial abdominal pain. These symptoms are considered to be the result of the dissection itself, or to ischemic signs of the abdominal organ (4). However, various clinical presentations, such as liver ischemia, splenic infarction, may occur according to the involvement of the branch vessels, and life threatening hemorrhage due to a rupture of the aneurysm (1, 4). The initial diagnosis of the visceral artery dissection is rarely established by symptoms. This disease entity is found incidentally during imaging studies for the purpose of evaluating other symptoms. Contrast enhanced CT is considered as the primary technique for diagnosing celiac artery dissection. There have been reported cases in which the CT findings of isolated dissection of the celiac artery were described (4, 5). The intimal flap with double lumen, thrombosis of false lumen or intramural hematoma, enlarged involved vessels were the findings of visceral artery dissection. Infiltration of the fat surrounding the affected vessel is a well-known secondary sign of acute spontaneous dissection of a visceral artery. Complications of the celiac artery dissection include hemorrhage or ischemic change of the distal organs, propagation of dissection into adjacent vessels, expansion of a false lumen, and the development of an aneurysm. The hepatic artery aneurysm could be presented as a complication of the celiac artery dissection. Expansion of a false lumen may cause either a rupture or poor perfusion to the supplied organ, secondary to the mechanical compression of the true lumen flow (6). However, the inability to predict either regression or expansion of a false lumen mandates close, life-long follow-up.
The management of celiac artery dissection depends on the hemodynamic status of the patient, response to conservative treatment, and development of complications (ischemia or hemorrhage). In asymptomatic stable dissection, current treatment recommendations are conservative treatment with anticoagulation or antiplatelet agents under close observation to prevent thromboembolic complications. Blood pressure control is necessary to minimize the progression of a dissection (4, 5). The indications for surgical or endovascular treatment include visceral ischemia, rupture of the dissection, progressing aneurysm (1, 2, 6-8). In the era of improved radiologic intervention, percutaneous endovascular treatment has been used as a surgical alternative with increasing frequency for the management of complicated splanchnic artery dissection because of its less invasiveness. Endovascular therapies include coil embolization, bare metal stent, and stent graft. The specific application of any interventional technique should be tailored to the needs of the individual patient, because each technique offers different advantages and disadvantages (6-8). Takach et al. (6) reported placement of a bare metal stent in a patient with celiac artery dissection as a treatment of poor perfusion secondary to mechanical compression of the true lumen by an expansion of the false lumen, following a failed conservative treatment. But, there was no evidence of a rupture in that case. In our cases, dissection of the celiac artery resulted in a rupture of aneurysm with decreased hemoglobin level in the first case, and progressing aneurysm with high risk of rupture in the second case. Conservative treatment, including anticoagulation or placement of a bare stent, was not amenable to treat or prevent bleeding in our cases because these therapies could not limit the aneurysm. Takeda et al. (8) reported isolated dissecting aneurysm of the celiac artery, extending into the proper hepatic artery that was successfully treated by transcatheter arterial embolization. Fortunately, in this reported case, intrahepatic branches were visualized after embolization through collateral pathways of the pancreatic arcade and epicholedochal arterial plexus from the superior mesenteric artery and dorsal pancreatic artery. However, proper collateral flow is essential for the use of transcatheter arterial embolization to treat a dissecting celiac artery to avoid organ infarction. Therefore, a stent-graft could be considered to control the bleeding from a ruptured aneurysm without the inadvertent development of complications caused by arterial embolization in poor collateral channels. Several reports have suggested the stent-graft as a valid alternative endovascular treatment for ruptured SMA dissection or celiac artery aneurysm (9, 10). A stent-graft that better preserves the distal flow might provide a safe, efficacious alternative to coil or plug embolization. In our cases, the involved vessels showed a smooth curvature to allow an easy navigation of a stent graft. In the first case, the patient had experienced a previous dissection of the superior mesenteric artery without complications. In addition, he had been treated with anticoagulant and hypertensive medication. The patient had discontinued anticoagulation after 6 months, and no serious complications concerning a superior mesenteric artery dissection was noted on a follow-up CT angiogram. The patient had stopped his hypertension medication arbitrarily. In addition, 10 months later, a ruptured dissecting aneurysm of the celiac artery developed with a concomitant decrease in hemoglobin. Most likely, arbitrary discontinuation of medication could explain the episode of celiac artery dissection. We successfully treated the dissecting aneurysm of the celiac artery that had ruptured with the retroperitoneal hematoma by the use of a stent graft. In the second case, although the urgent complication had not been noticed, the progressive enlargement of the aneurysm is at the greatest risk from rupturing. The patient was managed successfully with the placement of a stent graft.
To our knowledge, we are reporting the first case of a spontaneous celiac artery dissection treated with a stent graft. Percutaneous stent graft placement for the treatment of complicated spontaneous dissection of celiac artery is safe and feasible. However, studies with a large group of patients and long-term follow-up will be needed to validate this procedure.
Figures and Tables
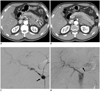 | Fig. 147-year-old man presented with acute abdominal pain.
A, B. Abdominal CT scan shows dissecting aneurysm in celiac artery with surrounding retroperitoneal hematoma (arrow). True lumen of celiac artery is narrowed by intramural hematoma (arrow). C. Celiac angiography shows saccular aneurysm in celiac artery (arrow). Splenic artery is occluded. D. Celiac angiography obtained after placement of stent graft reveals disappearance of dissecting aneurysm. Left gastric artery is visualized by collaterals from right gastric artery (arrow).
|
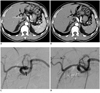 | Fig. 257-year-old man presented with acute abdominal pain.
A. Abdominal CT scan obtained 3 months before admission shows small dissecting aneurysm in celiac artery (arrow). B. Abdominal CT scan obtained on admission reveals growth of dissecting aneurysm along celiac artery, which has maximal inner diameter of 2 cm (arrow). C. Celiac angiography shows dissecting aneurysm in celiac artery. D. Post-procedure angiography shows complete exclusion of dissecting aneurysm with stent graft. No compromising blood flow was notice to distal hepatic artery, gastroduodenal artery, and splenic artery.
|
References
1. Nordanstig J, Gerdes H, Kocys E. Spontaneous isolated dissection of the celiac trunk with rupture of the proximal splenic artery: a case report. Eur J Vasc Endovasc Surg. 2009. 37:194–197.
2. Glehen O, Feugier P, Aleksic Y, Delannoy P, Chevalier JM. Spontaneous dissection of the celiac artery. Ann Vasc Surg. 2001. 15:687–692.
3. Woolard JD, Ammar AD. Spontaneous dissection of the celiac artery: a case report. J Vasc Surg. 2007. 45:1256–1258.
4. Oh S, Cho YP, Kim JH, Shin S, Kwon TW, Ko GY. Symptomatic spontaneous celiac artery dissection treated by conservative management: serial imaging findings. Abdom Imaging. 2011. 36:79–82.
5. D'Ambrosio N, Friedman B, Siegel D, Katz D, Newatia A, Hines J. Spontaneous isolated dissection of the celiac artery: CT findings in adults. AJR Am J Roentgenol. 2007. 188:W506–W511.
6. Takach TJ, Madjarov JM, Holleman JH, Robicsek F, Roush TS. Spontaneous splanchnic dissection: application and timing of therapeutic options. J Vasc Surg. 2009. 50:557–563.
7. Zhang T, Zhang X, Zhang X, Jiang J, Zhou B. Endovascular treatment of isolated spontaneous celiac artery dissection. Vascular. 2012. 20:118–120.
8. Takeda H, Matsunaga N, Sakamoto I, Obata S, Nakamura S, Hayashi K. Spontaneous dissection of the celiac and hepatic arteries treated by transcatheter embolization. AJR Am J Roentgenol. 1995. 165:1288–1289.
9. Carrafiello G, Rivolta N, Fontana F, Piffaretti G, Mariscalco G, Bracchi E, et al. Combined endovascular repair of a celiac trunk aneurysm using celiac-splenic stent graft and hepatic artery embolization. Cardiovasc Intervent Radiol. 2010. 33:352–354.
10. Nomura Y, Yamaguchi M, Kitagawa A, Okada T, Okita Y, Sugimoto K. Hybrid management of ruptured isolated superior mesenteric artery dissecting aneurysm. J Vasc Surg. 2011. 54:1808–1811.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download