Abstract
A 58-year-old female patient, diagnosed with adenocarcinoma of the lung, underwent percutaneous vertebroplasty at the L4 vertebral body due to painful spinal metastases. Because of deep venous thrombosis of the left femoral and iliac veins, an inferior vena cava filter had been placed before vertebroplasty. Bone cement migrated into the venous bloodstream and then was being trapped within the previously placed filter. This case illustrates that caval filter could capture the bone cement and prevent it from migrating to the pulmonary circulation.
Percutaneous vertebroplasty (PVP) is now widely used for the treatment of many painful vertebral compression fractures, which are secondary to osteoporosis, multiple myeloma, metastatic tumors, and hemangioma (1). Severe complications are rare and most are related to the leakage of the bone cement into the spinal canal or the perivertebral venous system (1). Here we present an interesting case of cement leakage into the venous system during PVP, extending into the inferior vena cava (IVC) and then being trapped within a previously placed IVC filter.
A 58-year-old female patient with a 1 year history of lung cancer was referred to our department for low back pain, left lower-limb swelling, cough and expectoration. Her low back pain was getting aggravated and the pain could not be controlled by analgesics. Computed tomography (CT) scan of spine revealed osteolytic metastatic lesion in the body of L4 without paravertebral space involvement. Ultrasound examination revealed free thrombus in the left iliac-femoral vein. To prevent pulmonary embolism (PE), a permanent IVC filter (OptEase™, Cordis, Roden, the Netherlands) was inserted in the IVC, before PVP was scheduled. The patient's coagulation function was normal. No anticoagulation or thrombolysis therapies were administered for the patient as the coming treatment.
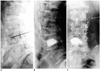
The PVP procedure was performed under local anesthesia, by using a unilateral approach with a 13-gauge needle (Osteo-site, Cook, Bloomington, IN, USA), and it was guided by a digital subtraction angiography (DSA) fluoroscopy. When the needle tip reached the one third of the anterior L4 vertebral body, intraosseous venography was performed, which showed a rapid venous filling (Fig. 1A): contrast material exited though the anterior external vertebral venous plexuses and emptied into the IVC. We repositioned the needle tip to avoid extravasation. However, venography findings were the same as before. The cement (CORIPLAST™ 3, Corin Medical, Gloucestershire, UK) was prepared by mixing a 2 g of sterile barium sulfate powder (Made by our hospital) for opacification, and was injected with a simple syringe during a paste-like viscosity. When the L4 vertebral body was nearly filled, fluoroscopy showed cement leaking into the IVC, and migrating to the filter (Fig. 1B, C). The injection of the cement was interrupted immediately; a total of 5 mL bone cement had been injected. The patient was hemodynamically stable, and no cardiopulmonary function disturbances were noted.
The low-molecular-weight heparin was given subcutaneously for 3 days after the PVP procedure, and was replaced by warfarin later. After the procedure of PVP, the low back pain of the patient was obviously released. No evidence of PE or IVC perforation presented. The left lower-limb swelling of the patient was recovered 1 week later. She was discharged 10 days after PVP, and was followed-up at our outpatient department. There were no complications that occurred, which related to the filter, within the 8 months of follow-up.
Cement leakage is the most frequently reported complication of PVP. The rate of cement leakage, outside the vertebral body, is reported to be 73%, and the rate of venous leakage cases is up to 24% (2). Although most patients with minor leaks are without symptoms, some disastrous consequences have still been reported (Table 1).
Inferior vena cava filter is a useful device to prevent PE in patients with deep-vein thrombosis. However, cases with foreign materials being trapped in the filter have not been reported frequently. To the best of our knowledge, there are only two cases of cement getting trapped in filters after PVP or kyphoplasty, reported in the previous literature (11, 12). In Herbstreit's report (11), the follow-up CT scan on several days after PVP showed cement reaching the IVC and rendering the filter unremovable in the usual fashion. In Agko's report (12), abdominal X-rays at eight weeks follow-up showed that the cement fragment embolized the caval filter. In our report, DSA fluoroscopy observed the whole process that cement migrating into the IVC and being captured in the filter. It is the direct evidence that filter can capture bone cement and prevent it from migrating to the pulmonary circulation.
In Herbstreit's report (11), removal of the cemented filter via endovascular technology was impossible and the patient underwent cavotomy and surgical extraction of the filter. In our report, due to the history of malignancy, a permanent filter was used and removal of the filter was not considered. However, the possibilities of further thrombosis and vascular injury should be considered. There was no evidence of IVC syndrome, IVC perforation, or PE presented in the procedure and follow-up. Surgical attempt at the retrieval of the fiter may pose a prohibitive risk in our case. As such, we decided to administer an anticoagulant treatment, and ask the patient to follow up at the outpatient department. The patient's left lower-limb swelling subsided 1 week later and there were no complications related to the filter at the 8 months follow-up.
The utility of antecedent venography to decrease the cement leakage during PVP is controversial. Some authors emphasized that venography does not preclude the cement leakage exactly because of the difference of viscosity between the contrast material and bone cement. Some reports demonstrated no significant differences in the frequency or amount of cement leakage and no differences in the clinical outcome between venography and no venography (13, 14). However, some authors advocated using an antecedent venography to confirm the needle position in the trabecular space, to outline the venous outflow pattern, and to show where to look for the cement migration. We conformed to the latter perspective (15). In this case, the direction of cement migration was coincident with the venous blood flow, detected by a venography, which indicated that intraosseous venography predicted the direction of venous cement leakage effectively. According to our experience, cement leakage happened more often in patients with draining veins, which appeared ahead of time on a venography (15). In this case, the antecedent venography showed rapid venous filling, which reminded us to prevent cement leakage. However, it did occur, though the needle tip was repositioned. Bhatia recommended a routine pre-injection of the gelatin clotting agent to reduce the cement leakage during PVP (16). In our opinion, this method is more suitable to the vertebrae with rapid venous flow, such as the status of this patient. If this method was used in this patient, venous leakage would have been avoided.
In summary, this interesting case illustrates that IVC filter could capture bone cement and prevent it from migrating to the pulmonary circulation. Vertebral body venography could predict the direction of the bone cement leakage to the veins, effectively.
Figures and Tables
Fig. 1
Cement getting trapped in IVC filter during percutaneous vertebroplasty.
A. Basivertebral veins drained into anterior external vertebral venous plexuses and IVC (arrowhead). Cement injection of L4 vertebrae: cement migrates into IVC and gets caught in filter. B. Lateral fluoroscopy. C. Anteroposterior fluoroscopy. IVC = inferior vena cava
References
1. Barragán-Campos HM, Vallée JN, Lo D, Cormier E, Jean B, Rose M, et al. Percutaneous vertebroplasty for spinal metastases: complications. Radiology. 2006. 238:354–362.
2. Yoo KY, Jeong SW, Yoon W, Lee J. Acute respiratory distress syndrome associated with pulmonary cement embolism following percutaneous vertebroplasty with polymethylmethacrylate. Spine (Phila Pa 1976). 2004. 29:E294–E297.
3. Chung SE, Lee SH, Kim TH, Yoo KH, Jo BJ. Renal cement embolism during percutaneous vertebroplasty. Eur Spine J. 2006. 15:Suppl 5. 590–594.
4. Marden FA, Putman CM. Cement-embolic stroke associated with vertebroplasty. AJNR Am J Neuroradiol. 2008. 29:1986–1988.
5. Stricker K, Orler R, Yen K, Takala J, Luginbühl M. Severe hypercapnia due to pulmonary embolism of polymethylmethacrylate during vertebroplasty. Anesth Analg. 2004. 98:1184–1186.
6. Lim KJ, Yoon SZ, Jeon YS, Bahk JH, Kim CS, Lee JH, et al. An intraatrial thrombus and pulmonary thromboembolism as a late complication of percutaneous vertebroplasty. Anesth Analg. 2007. 104:924–926.
7. Kim SY, Seo JB, Do KH, Lee JS, Song KS, Lim TH. Cardiac perforation caused by acrylic cement: a rare complication of percutaneous vertebroplasty. AJR Am J Roentgenol. 2005. 185:1245–1247.
8. Kao FC, Tu YK, Lai PL, Yu SW, Yen CY, Chou MC. Inferior vena cava syndrome following percutaneous vertebroplasty with polymethylmethacrylate. Spine (Phila Pa 1976). 2008. 33:E329–E333.
9. Chen YJ, Tan TS, Chen WH, Chen CC, Lee TS. Intradural cement leakage: a devastatingly rare complication of vertebroplasty. Spine (Phila Pa 1976). 2006. 31:E379–E382.
10. Son KH, Chung JH, Sun K, Son HS. Cardiac perforation and tricuspid regurgitation as a complication of percutaneous vertebroplasty. Eur J Cardiothorac Surg. 2008. 33:508–509.
11. Herbstreit F, Kühl H, Peters J. A cemented caval vein filter: case report. Spine (Phila Pa 1976). 2006. 31:E917–E919.
12. Agko M, Nazzal M, Jamil T, Castillo-Sang M, Clark P, Kasper G. Prevention of cardiopulmonary embolization of polymethylmethacrylate cement fragment after kyphoplasty with insertion of inferior vena cava filter. J Vasc Surg. 2010. 51:210–213.
13. Vasconcelos C, Gailloud P, Beauchamp NJ, Heck DV, Murphy KJ. Is percutaneous vertebroplasty without pretreatment venography safe? Evaluation of 205 consecutives procedures. AJNR Am J Neuroradiol. 2002. 23:913–917.
14. Wong W, Mathis J. Is intraosseous venography a significant safety measure in performance of vertebroplasty? J Vasc Interv Radiol. 2002. 13(2 Pt 1):137–138.
15. Ni RF, Chen L, Xu BS, Yang HL, Hu YC, Ding Y, et al. [The application value of vertebral body venography in performance of percutaneous vertebroplasty]. Chin J Orthop. 2006. 26:1–6.
16. Bhatia C, Barzilay Y, Krishna M, Friesem T, Pollock R. Cement leakage in percutaneous vertebroplasty: effect of preinjection gelfoam embolization. Spine (Phila Pa 1976). 2006. 31:915–919.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download