Abstract
Objective
To compare the ancillary CT findings between superior mesenteric artery thromboembolism (SMAT) and superior mesenteric vein thrombosis (SMVT), and to determine the independent CT findings of life-threatening mesenteric occlusion.
Materials and Methods
Our study was approved by the institution review board. We included 43 patients (21 SMAT and 22 SMVT between 1999 and 2008) of their median age of 60.0 years, and retrospectively analyzed their CT scans. Medical records were reviewed for demographics, management, surgical pathology diagnosis, and outcome. We compared CT findings between SMAT and SMVT groups. Multivariate analysis was conducted to determine the independent CT findings of life-threatening mesenteric occlusion.
Results
Of 43 patients, 24 had life-threatening mesenteric occlusion. Death related to mesenteric occlusion was 32.6%. A thick bowel wall (p < 0.001), mesenteric edema (p < 0.001), and ascites (p = 0.009) were more frequently associated with SMVT, whereas diminished bowel enhancement (p = 0.003) and paralytic ileus (p = 0.039) were more frequent in SMAT. Diminished bowel enhancement (OR = 20; p = 0.007) and paralytic ileus (OR = 16; p = 0.033) were independent findings suggesting life-threatening mesenteric occlusion.
Bowel ischemia caused by mesenteric occlusion would have a grave prognosis if not timely diagnosed and treated (1, 2). However, the diagnosis of mesenteric occlusion could be elusive based on physical examination because a wide spectrum of clinical presentations may occur ranging from nonspecific abdominal pain in the abdomen (3). The severity of mesenteric occlusion depends on whether the occlusion results in transient mucosal changes or a more severe transmural wall necrosis.
Catheter angiography or the state-of-the-art CT-angiography is the standard reference for diagnosis of mesenteric occlusion in selected patients (4-6). However, because of the limited availability of high-end multiple-row detector CT (MDCT) scanners and the lack of clinical suspicion prior to the CT scan, the more readily available regular CT examination has been used as a screening modality in emergency rooms (7-9). This regular contrast-enhanced MDCT can clearly delineate the mesenteric vessels and ancillary findings of mesenteric occlusion (9-11). Many nonspecific MDCT findings of mesenteric occlusion such as a thick bowel wall, thin bowel wall, strong bowel wall enhancement, diminished bowel wall enhancement, intramural gas, mesenteric edema, and ascites have been reported (10, 12-15). However, findings such as a thick bowel wall and thin bowel wall, strong wall enhancement and diminished wall enhancement could be mutually contradictory and confusing (16).
Our first hypothesis is that the ancillary findings of superior mesenteric artery thromboembolism (SMAT) and superior mesenteric vein thrombosis (SMVT) on contrast-enhanced MDCT are different or occur at different frequencies. Consequently, confusion would occur if we do not address the CT findings of SMAT and SMVT separately. Second, regardless of SMAT or SMVT, life-threatening mesenteric occlusion would occur if the collateral circulation for bowel perfusion is inadequate. Therefore, we conducted a retrospective study to compare the ancillary CT findings between SMAT and SMVT as well as between patients of life-threatening and non-life-threatening mesenteric occlusion.
This retrospective study was approved by our institution review board and informed consent was waived. We searched from our radiology information system for emergency CT reports containing impression keywords of main mesenteric occlusion (SMAT and SMVT) between January 1999 and December 2008. We defined SMAT and SMVT as total occlusion of the SMA trunk and SMV trunk, respectively, by thromboembolism or thrombosis. A total of 68 CT reports of mesenteric occlusion were identified. Eighteen CT examinations were incomplete or of poor enhancement quality and were thus excluded. Also, an additional seven were excluded because they were not admitted or had been transferred to another hospital. The remaining 43 patients (21 SMAT, 22 SMVT), which comprised of 17 women and 26 men, with a median age of 60.0 years (interquartile range 46.0, 78.0 years) formed the study group. The 21 SMATs were caused by atrial fibrillation (n = 13), other heart diseases (n = 3), atherosclerosis (n = 4), and unconfirmed causes (n = 1). Causes for SMVT were more variable and consist of abdominal infection (n = 6), hypercoagulation (n = 3), liver disease (n = 3), renal disease (n = 2), cancer (n = 1), recent surgery (n = 1), others (n = 3), and unconfirmed causes (n = 3).
The medical charts were independently reviewed by a co-investigator who did not know the CT findings for demographic data, management choice, surgical pathology diagnosis, and outcome (dead or alive). If bowel gangrene or hemorrhagic necrosis was recorded in surgical pathology diagnosis, then the mesenteric occlusion was defined as life-threatening. Life-threatening mesenteric occlusion was also assigned to patients who had not undergone surgery but died within 24 hours after CT examination was performed (11).
All CT examinations were performed in the emergency room with a 4-detector MDCT scanner (LightSpeed QX/i Scanner, General Electric Medical Systems, Milwaukee, WI, USA). The routine protocol for an emergency abdominal CT examination in this study consisted of a non-enhanced and a contrast-enhanced series. All patients were scanned from the basal lung to pubic symphysis. The images were obtained with a high quality mode at 11.25 mm/rotation, 120 kVp, 200-250 mA, 5 mm slice thicknesses and 5 mm intervals. No oral contrast medium was ingested for gastrointestinal tract opacification. A uniphasic injection of 100-120 mL of intravenous iodinated contrast material Omnipaque 350 (Iohexol, 350 mgI/mL, GE Healthcare, Belfast, Ireland) was administered at a rate of 2-3 mL/second for the contrast-enhanced series. The portal venous phase contrast-enhanced series was obtained at 70-90 seconds after the initiation of the contrast material injection.
Two abdominal radiologists with more than 10-years of experience were asked to review all CT examinations retrospectively on picture archiving communication systems for bowel and mesenteric abnormalities. They were aware of mesenteric occlusion but did not know the final condition of the bowel ischemia. They were free to use different window settings and discuss findings. A consensus interpretation obtained after discussion was recorded. Small bowel walls greater than 3 mm in thickness were recorded as abnormal bowel wall thickening. Wall enhancement of the small bowel was compared with that of the duodenum and rectosigmoid colon. Diminished enhancement was recorded if a segment of the small bowel wall was hypodense compared to that of the duodenum or rectosigmoid colon based on qualitative assessment. Enhancement of the duodenum and rectosigmoid colon was used as a standard reference for comparison because enhancement of the duodenum and rectosigmoid colon was mainly supplied by the gastroduodenal artery and hemorrhoidal arteries, respectively. Pneumatosis intestinalis was defined as small bowel intramural gas, and paralytic ileus as small bowel distention more than 3 cm in diameter without a transitional zone. An increase of mesenteric fat density was recorded as mesenteric edema. The presence of peritoneal fluid was recorded as ascites. Another radiologist was requested to measure the cross-sectional diameters of the main mesenteric vessels (SMV and SMA) at the level of occlusion and compute a ratio of SMV to SMA diameters (VA ratio).
We compared the ancillary CT findings between patients of SMAT and SMVT to determine the difference of their occurring frequencies. Demographics and CT findings were compared with life-threatening mesenteric occlusion in a univariate analysis. The categorical variables were tested by the chi-square test or Fisher's exact test if one of the cells had an expected count less than 5. The VA ratio and age were computed with the Mann-Whitney U-test and their respective optimal cutoff values were determined by the receiver operating characteristic (ROC) curve. Logistic regression was used to determine the independent factors and adjusted odds ratios (ORs) of life-threatening mesenteric occlusion. A two-tailed p value of less than 0.05 was considered statistically significant.
Of the 43 patients, 24 had life-threatening mesenteric occlusion. Among these 24 patients, 22 were proven by surgery, and 2 critical patients were non-operable and died of sepsis and acidosis within twenty-four hours after CT examination. Of these two patients, who presented with atrial fibrillation and mesenteric occlusion, one had concurrent spleen infarct and the other had kidney infarct.
Overall, 16 patients died in this series. Among them, 14 patients died of mesenteric occlusion and bowel ischemia. The death rate related to mesenteric occlusion was 32.6% (14/43). Of the other 2 patients, 1 died of cancer, and the other died of fulminant hepatitis.
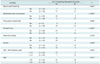
The CT findings (Fig. 1) of the thick bowel wall (p < 0.001), mesenteric edema (p < 0.001), and ascites (p = 0.009) were more frequently associated with SMVT (Table 1). In contrast, diminished bowel wall enhancement (p = 0.003) and paralytic ileus (p = 0.039) were more significantly found in SMAT (Fig. 2). Although pneumatosis intestinalis was more frequent in SMAT (Fig. 3), the difference did not reach a statistical significance (p = 0.185). The VA ratio was larger in the SMVT group than in the SMAT group (p < 0.001).
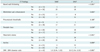
Table 2 shows that life-threatening mesenteric occlusion had no predilection in gender but was associated with the necessity of surgery (p < 0.001), death (p = 0.001), SMAT (p = 0.001), smaller VA ratio (p = 0.001) and older age (p = 0.019). The area under the ROC curve for age and VA ratio was 0.709 (p = 0.020) and 0.802 (p = 0.001), respectively. The optimal cutoff values of age ≥ 50 years and VA ratio < 1.5 for life-threatening mesenteric occlusion were determined by ROC curves.
As detailed in univariate analysis (Tables 2, 3), the significant variables of life-threatening mesenteric occlusion with a p value < 0.100 were SMAT (p = 0.001), diminished bowel wall enhancement (p < 0.001), paralytic ileus (p < 0.001), pneumatosis intestinalis (p = 0.056), VA ratio < 1.5 (p = 0.001), and age ≥ 50 years (p = 0.011). By controlling above variables using logistic regression (Table 4), diminished bowel wall enhancement (OR = 20; p = 0.007) and paralytic ileus (OR = 16; p = 0.033) were independent factors of life-threatening mesenteric occlusion. This model could correctly predict 95.8% of the life-threatening mesenteric occlusion in this study group.
Many abnormal CT findings of mesenteric occlusion have been reported (10, 12-17). Investigators have been attempting to explain these findings by using different physiology states of mesenteric ischemia (14, 18, 19). We were unable to correctly retrieve the exact time of disease onset and therefore could not correlate the CT findings with the changes in pathophysiology states. However, we have confirmed our hypothesis that the abnormal ancillary CT findings occur at different frequencies between patients of SMAT and SMVT.
The mesentery is richly innervated by the autonomic nervous system that coordinates the contractile activity of the bowel (19, 20). As seen in the SMAT patients of this series, the ischemic nervous system would paralyze the coordinated bowel peristalsis and result in paralytic ileus (14, 21). Arterial occlusion could also interrupt bowel perfusion and cause diminished wall enhancement of the affected bowels (16, 19-21). The poor inner-layer enhancement indicates mucosal ischemia, whereas a diminished transmural enhancement is consistent with a whole-layer wall ischemia that may lead to a life-threatening bowel infarct (22). The ischemic mucosa of SMAT may allow dissection of intraluminal gas into the mural layer as pneumatosis intestinalis (19). Moreover, it could be exacerbated by translocation of gas-forming bacilli and the increase of intraluminal pressure as a result of paralytic ileus (19). Although there was no statistical significance, pneumatosis intestinalis was more frequently associated with SMAT than SMVT.
In contrast, SMVT would result in an increase of intravascular volume and elevation of hydrostatic pressure if the collateral draining veins are inadequate (19, 20). The blood cells, plasma and the administered contrast medium are forced through the endothelium fenestrations into submucosal and mucosal spaces (19, 20) that result in concentric bowel wall thickening if the mucosal and serosal enhancement is still preserved. If the venous pressure is not alleviated, it could gradually compromise the in-flow of arterioles and capillaries (15). The concentric bowel wall would then become a thick wall with diminished enhancement. Hemorrhagic necrosis of the affected bowel may subsequently occur (23). In this series, bowel necrosis was less common in SMVT than in SMAT. The increase of mesenteric fat density in SMVT patients is caused by mesenteric edema as a result of the elevated hydrostatic pressure (19, 20). Intravascular fluid could also be forced out into the mesenteric space and other peritoneal spaces as ascites (19, 20).
We have confirmed the observation of Kurimoto et al. (24) that a small VA ratio is a helpful screening criterion for arterial mesenteric occlusion. The SMV diameter is usually larger than the adjacent SMA diameter. However, upon mesenteric occlusion, the diameter of the occluded segment would become larger than its otherwise non-occlusive status (24). In our series, the VA ratio in SMAT was reduced to 1 : 1 due to engorgement of the occluded SMA. In contrast, the VA ratio of SMVT was increased to 2 : 1 due to SMV engorgement.
Although life-threatening mesenteric occlusion was associated with elderly patients, small VA ratio, SMAT, diminished wall enhancement, pneumatosis intestinalis and paralytic ileus in univariate analysis, the significant independent factors were diminished wall enhancement and paralytic ileus. Patients exhibiting mesenteric occlusion (regardless of SMAT or SMVT) with diminished bowel wall enhancement were twenty times more likely than otherwise to proceed to a life-threatening condition. Likewise, patients of mesenteric occlusion with paralytic ileus were sixteen times more likely to proceed to a life-threatening condition. Death is still significantly associated with life-threatening mesenteric occlusion despite aggressive surgical intervention to remove the nonviable bowel and restore mesenteric blood flow. Death related to mesenteric occlusion in this study was 32.6%, consistent with the high mortality rates previously reported (1, 2).
Although small VA ratio (< 1.5) and pneumatosis intestinalis were more frequently associated with life-threatening mesenteric occlusion, this study of the small sample was not able to prove that they were significant independent predictors. Unlike CT-angiography, the regular contrast-enhanced CT has a limitation in detecting embolic occlusion of peripheral arterial branches leading to a false negative diagnosis and underestimation of acute SMAT. Selection bias was unavoidable because we retrieved records of main trunk mesenteric occlusion from the radiology information system and excluded those with poor CT quality or those without hospital admission. Regarding CT interpretation, we recorded the consensus of two experienced radiologists and did not analyze if there was any discrepancy in interpretation between experienced radiologists and junior radiologists. Another limitation of this study is that two patients of the life-threatening group did not have a pathology diagnosis and died within twenty-four hours after CT examination. They were un-operable at the time of presentation. Furthermore, autopsy is seldom performed in our hospital unless it is court ordered.
Abnormal ancillary CT findings occur at different frequencies in arterial or venous mesenteric occlusion. Diminished bowel wall enhancement, paralytic ileus and pneumatosis intestinalis are more frequent in SMAT. In contrast, bowel wall thickening, mesenteric edema, and ascites are more frequent in SMVT. The independent CT findings of life-threatening mesenteric occlusion are diminished bowel wall enhancement and paralytic ileus.
Figures and Tables
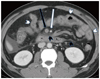 | Fig. 1
46 year-old male of nephrotic syndrome. CT scans shows acute superior mesenteric vein thrombosis (black arrow) with bowel wall thickening (white arrowhead), mesenteric edema (black arrowhead) and ascites. Note the normal SMA enhancement (white arrow) and ratio of SMV to SMA diameters > 2. He did not receive surgery but was treated with anticoagulation therapy. Follow-up CT showed abundant collateral veins and no bowel necrosis. SMA = superior mesenteric artery, SMV = superior mesenteric vein |
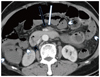 | Fig. 2
73 year-old female of atrial fibrillation and paralytic ileus. CT scan shows acute superior mesenteric artery occlusion (white arrow) with diminished enhancement of thin bowel walls (white arrowheads) as compared to normal duodenum (black arrowhead). Note normal SMV enhancement (black arrow) and ratio of SMV to SMA diameters of about 1. Extensive bowel gangrene was found at exploratory laparotomy. Bowel resection was not possible and she died of sepsis and acidosis. SMA = superior mesenteric artery, SMV = superior mesenteric vein |
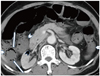 | Fig. 3
Although the SMA orifice is normally enhanced, CT scans caudal to this level (not shown) reveal acute superior mesenteric artery occlusion. Note diminished enhancement of thin bowel walls (white arrowheads) as compared to normal duodenum (black arrowhead) and pneumatosis intestinalis (white arrows). Resection of small bowel and right colon showed coagulative necrosis. This 86 year-old female patient died of sepsis 4 days later. SMA = superior mesenteric artery |
Table 2
Comparison of Clinical Characteristics between Life-Threatening and Non-Life-Threatening Mesenteric Occlusion Groups

References
1. Schoots IG, Koffeman GI, Legemate DA, Levi M, van Gulik TM. Systematic review of survival after acute mesenteric ischaemia according to disease aetiology. Br J Surg. 2004. 91:17–27.
2. Yasuhara H. Acute mesenteric ischemia: the challenge of gastroenterology. Surg Today. 2005. 35:185–195.
3. Martinez JP, Hogan GJ. Mesenteric ischemia. Emerg Med Clin North Am. 2004. 22:909–928.
4. Bakal CW, Sprayregen S, Wolf EL. Radiology in intestinal ischemia. Angiographic diagnosis and management. Surg Clin North Am. 1992. 72:125–141.
5. Klein HM, Lensing R, Klosterhalfen B, Töns C, Günther RW. Diagnostic imaging of mesenteric infarction. Radiology. 1995. 197:79–82.
6. Kim JH, Ha HK, Sohn MJ, Shin BS, Lee YS, Chung SY, et al. Usefulness of MR imaging for diseases of the small intestine: comparison with CT. Korean J Radiol. 2000. 1:43–50.
7. Leschka S, Alkadhi H, Wildermuth S, Marincek B. Multi-detector computed tomography of acute abdomen. Eur Radiol. 2005. 15:2435–2447.
8. Federle MP. CT of the acute (emergency) abdomen. Eur Radiol. 2005. 15:Suppl 4. D100–D104.
9. Horton KM, Fishman EK. Multi-detector row CT of mesenteric ischemia: can it be done? Radiographics. 2001. 21:1463–1473.
10. Rosow DE, Sahani D, Strobel O, Kalva S, Mino-Kenudson M, Holalkere NS, et al. Imaging of acute mesenteric ischemia using multidetector CT and CT angiography in a porcine model. J Gastrointest Surg. 2005. 9:1262–1274. discussion 1274-1275.
11. Kirkpatrick ID, Kroeker MA, Greenberg HM. Biphasic CT with mesenteric CT angiography in the evaluation of acute mesenteric ischemia: initial experience. Radiology. 2003. 229:91–98.
12. Wiesner W, Khurana B, Ji H, Ros PR. CT of acute bowel ischemia. Radiology. 2003. 226:635–650.
13. Segatto E, Mortelé KJ, Ji H, Wiesner W, Ros PR. Acute small bowel ischemia: CT imaging findings. Semin Ultrasound CT MR. 2003. 24:364–376.
14. Romano S, Romano L, Grassi R. Multidetector row computed tomography findings from ischemia to infarction of the large bowel. Eur J Radiol. 2007. 61:433–441.
15. Tang ZH, Qiang JW, Feng XY, Li RK, Sun RX, Ye XG. Acute mesenteric ischemia induced by ligation of porcine superior mesenteric vein: multidetector CT evaluations. Acad Radiol. 2010. 17:1146–1152.
16. Rha SE, Ha HK, Lee SH, Kim JH, Kim JK, Kim JH, et al. CT and MR imaging findings of bowel ischemia from various primary causes. Radiographics. 2000. 20:29–42.
17. Moschetta M, Stabile Ianora AA, Pedote P, Scardapane A, Angelelli G. Prognostic value of multidetector computed tomography in bowel infarction. Radiol Med. 2009. 114:780–791.
18. Chang RW, Chang JB, Longo WE. Update in management of mesenteric ischemia. World J Gastroenterol. 2006. 12:3243–3247.
19. Gore RM, Yaghmai V, Thakrar KH, Berlin JW, Mehta UK, Newmark GM, et al. Imaging in intestinal ischemic disorders. Radiol Clin North Am. 2008. 46:845–875. v
20. Romano S, Niola R, Maglione F, Romano L. Small bowel vascular disorders from arterial etiology and impaired venous drainage. Radiol Clin North Am. 2008. 46:891–908. vi
21. Romano S, Lassandro F, Scaglione M, Romano L, Rotondo A, Grassi R. Ischemia and infarction of the small bowel and colon: spectrum of imaging findings. Abdom Imaging. 2006. 31:277–292.
22. Chou CK, Wu RH, Mak CW, Lin MP. Clinical significance of poor CT enhancement of the thickened small-bowel wall in patients with acute abdominal pain. AJR Am J Roentgenol. 2006. 186:491–498.
23. Cenedese A, Monneuse O, Gruner L, Tissot E, Mennesson N, Barth X. Initial management of extensive mesenteric venous thrombosis: retrospective study of nine cases. World J Surg. 2009. 33:2203–2208.
24. Kurimoto Y, Morishita K, Fukada J, Kawaharada N, Komatsu K, Yama N, et al. A simple but useful method of screening for mesenteric ischemia secondary to acute aortic dissection. Surgery. 2004. 136:42–46.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download