INTRODUCTION
MATERIALS AND METHODS
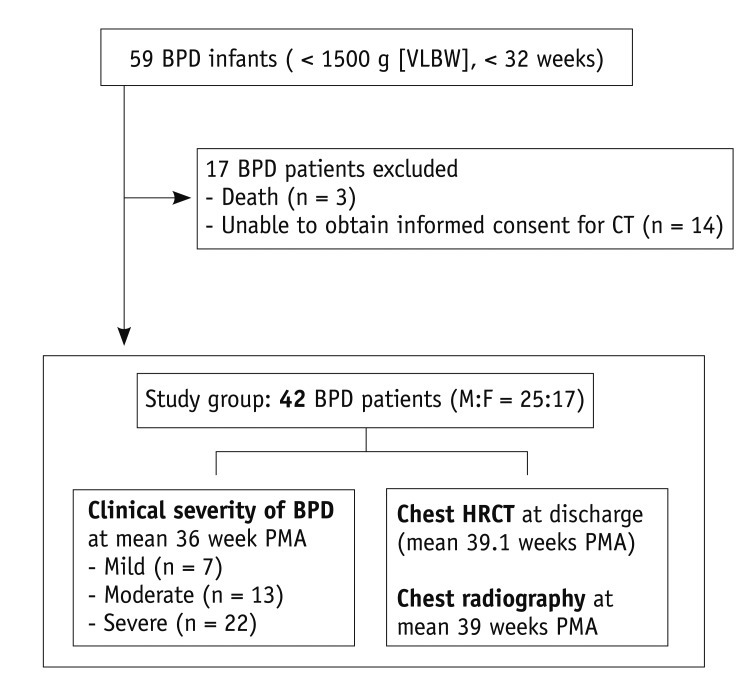
Patients
Clinical Severity of BPD
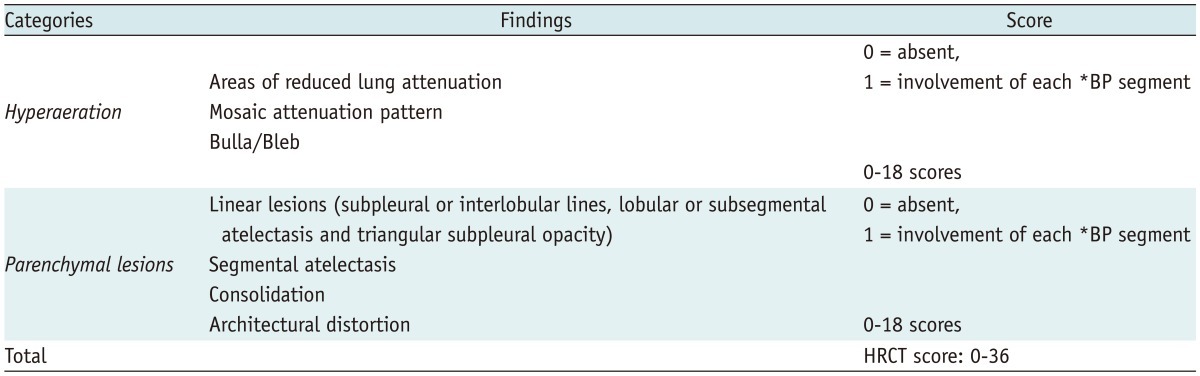
Chest HRCT Score
HRCT Imaging
New HRCT Scoring System for BPD
Chest Radiographic Score
Follow-Up Clinical Information and Follow-Up Imaging Study
Statistical Analysis
RESULTS
Interobserver and Intraobserver Reproducibility
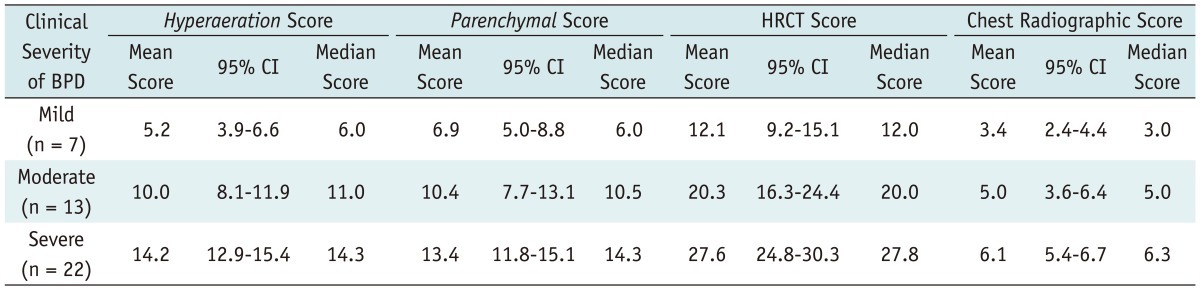
Correlation between Radiologic Scores and Clinical Severity
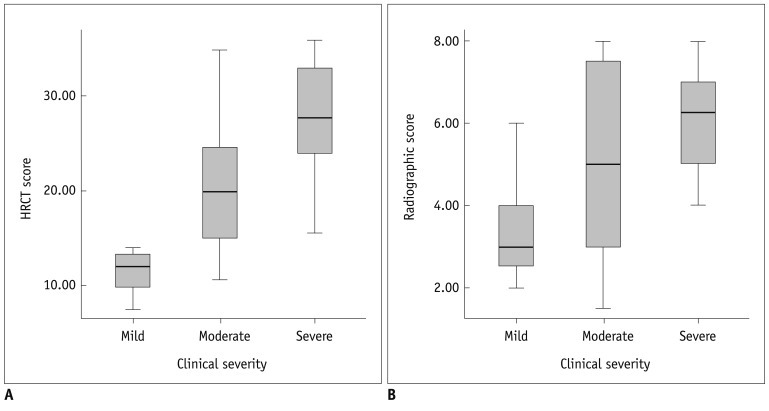 | Fig. 2Correlation between radiologic scores and clinical severity in bronchopulmonary dysplasia (BPD) patients.
HRCT score (A) shows significant correlation (r = 0.646, p < 0.001) with clinical severity of BPD. Chest radiographic score (B) also shows significant correlation (r = 0.410, p = 0.007) with clinical severity of BPD. HRCT score shows better correlation with clinical severity of BPD than chest radiographic score (p = 0.003). HRCT = high resolution computed tomography
|
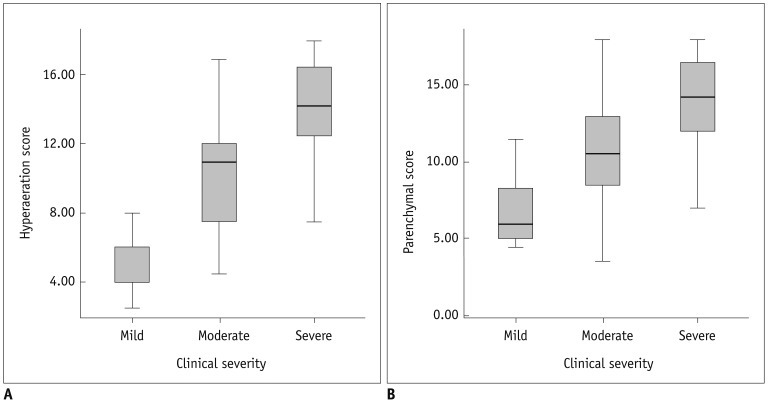 | Fig. 3Correlation between hyperaeration and parenchymal scores of HRCT and clinical severity.
Hyperaeration score (A) shows significant correlation (r = 0.738, p < 0.001) with clinical severity. Parenchymal score (B) shows significant correlation (r = 0.523, p < 0.001) with clinical severity. Hyperaeration score shows better correlation with clinical severity than parenchymal score (p < 0.001). HRCT = high resolution computed tomography
|
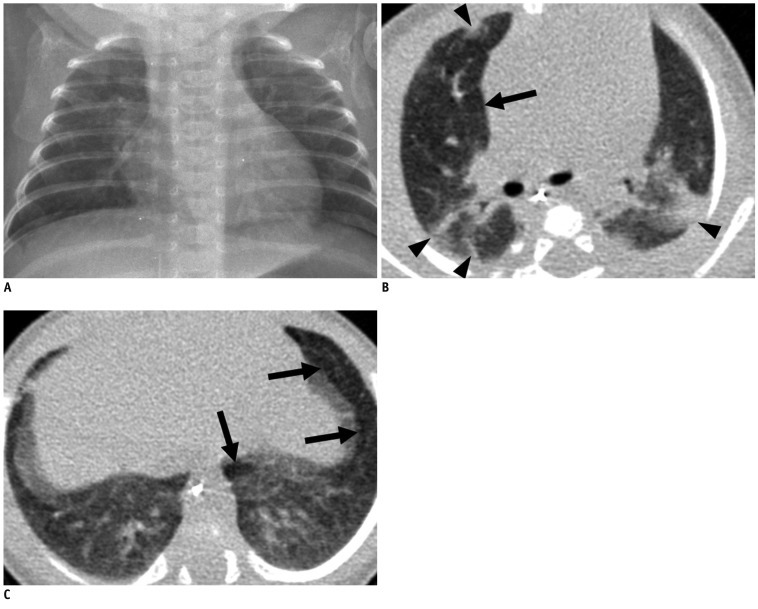 | Fig. 4Mild bronchopulmonary dysplasia in 41.1-week-old female infant born at 29.9 weeks of gestation with birth weight of 1280 g.
Chest radiograph (A) shows mild cardiomegaly and few streaks of abnormal density (radiographic score = 2). Transverse HRCT scan (B) at level of bronchus intermedius shows hyperaeration in anterior segment of right upper lobe (arrow) and parenchymal lesions in anterior and posterior segments of right upper lobe and apicoposterior segment of left upper lobe (arrowheads). Transverse HRCT scan (C) at level of liver dome shows hyperaeration in anteromedial basal segment of left lower lobe and in lingular inferior segment of left upper lobe (arrows). HRCT score was 12 with hyperaeration and parenchymal lesions in 6 segments, respectively. HRCT = high resolution computed tomography
|
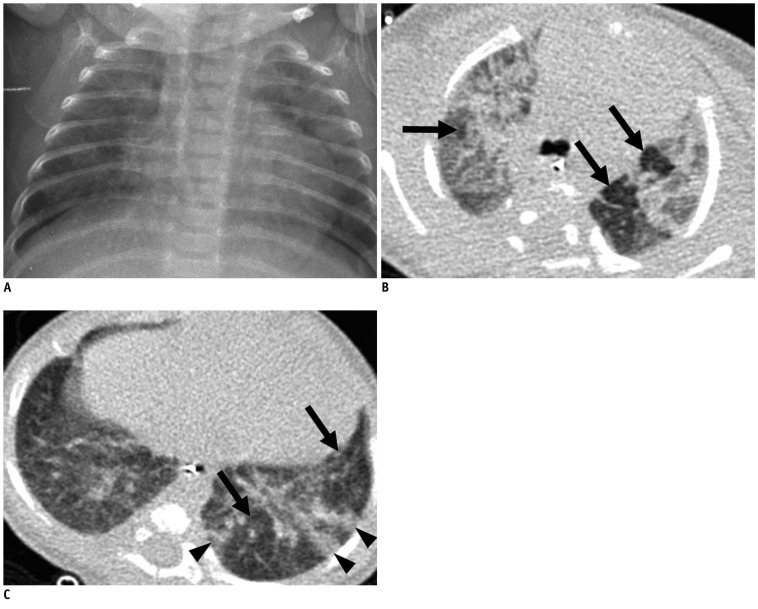 | Fig. 5Moderate bronchopulmonary dysplasia in 39.0-week-old male infant born at 29.9 weeks of gestation with birth weight of 620 g.
Chest radiograph (A) shows mild cardiomegaly, hyperexpansion (rib count: 15 1/2) and many abnormal strands (radiographic score = 5.5). Transverse HRCT scan (B) at level of carina shows hyperaeration (arrows) and parenchymal lesions in all segments of both upper lobes. Transverse HRCT scan (C) at level of liver dome shows hyperaeration in lateral and posterior basal segments of left lower lobe (arrows), and parenchymal lesions in lateral and posterior basal segment of left lower lobe (arrowheads). HRCT score was 24 with hyperaeration in 13 segments and parenchymal lesions in 11 segments, respectively. HRCT = high resolution computed tomography
|
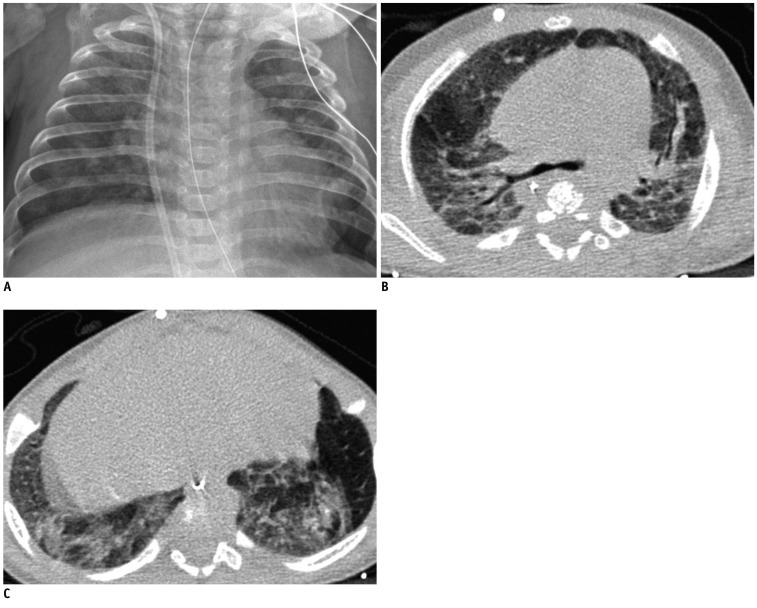 | Fig. 6Severe bronchopulmonary dysplasia in 54.7-week-old male infant born at 25.1 weeks of gestation with birth weight of 820 g.
Chest radiograph (A) shows mild cardiomegaly, hyperexpansion (rib count: 16), scattered small abnormal lucencies and many abnormal strands (radiographic score = 6). Transverse HRCT scans at level of carina (B) and liver dome (C) show hyperaeration and parenchymal lesions in all segments seen on scan. HRCT score was 36 with hyperaeration and parenchymal lesions in 18 segments, respectively. HRCT = high resolution computed tomography
|




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download