This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
To investigate the value of 3-dimensional (3D) CT virtual anatomy imaging (VAI) in the complex foreign body (FB) retrieval of the soft tissues.
Materials and Methods
Four hundred and seventy-five patients with radiopaque FB(s) diagnosed by radiograph underwent contrast-enhanced 3D CT examination. VAI was reconstructed by volume-rendering opacity software, by sliding down the lowest threshold from -600 to 100 HU. The imaging was grouped into three groups: A (axial and multi-planar reformation [MPR] images), B (standard 3D imaging with axial and MPR images), and C (VAI with axial and MPR images). They were analyzed to reveal the type, size, number, location, complications, and the interventional removability of the object, with the comparisons in the management and clinical outcomes on the patient follow-up studies. The data were subjected to chi-square tests, with p value < 0.05 indicating significant statistical difference.
Results
The FB shape, size, number, site distribution and vessels around FB, as well as the FB-associated vascular complications and the FB interventional removability were assessed more accurately in Group C than in Group B or Group A (p < 0.005). There was no significant difference in disclosing the type and depth of the FB among the three groups (p > 0.75). On the basis of the 3D CT, especially the enhanced 3D CT VAI, the followings were processed: the recommendation of interventional removal in 286 (60.47%) and non-intervention in 187 (39.53%) of the 473 patients with soft-tissue FB(s); in 352 (56.50%) of the 623 radiopaque FBs patients, 258 (54.55%) patients accurately detected on 3D CT and the successful removal by intervention (343 FBs) or surgery (9 FBs) without any sequela; and 215 (45.45%) patients with 271 FBs lost in the follow-up, with their departure from the hospital.
Conclusion
The 3D CT, especially 3D enhanced CT VAI, has great incremental value in further diagnosis and management of complex FB extraction from soft tissues.
Go to :

Keywords: Foreign body, Tomography, X-ray computer, Image processing, Computer-assisted, Regional anatomy, Interventional radiology
INTRODUCTION
The foreign body (FB) can induce immediate or slow tissue trauma, toxicity, allergic reaction, inflammation, infection, tumor-like granuloma, tenosynovitis (
1-
3), and even tumors (
1,
4), as it is introduced into soft tissues through various mechanisms, including penetrating injury, medical accident, cosmetic treatment, or self-embedding behavior (
2,
5,
6). Along with the various processes of the industrialization of the society, quickening course of urbanization, increasing degree of complexity and speed of the industrial mechanization and global events, the incidence of human FB is now significantly increased and the age of onset is getting younger. Once the object is discovered, the clinician must weigh the potential harm of the foreign body in its current location against the risks of the removal attempt (
4,
7). In general, prompt removal of the object is necessary to avoid its migration causing further damage to the surrounding tissues, in particular the vital nerves and blood vessels (
1,
7-
9).
Regardless of the treatment adopted for the FB lodged in soft tissues, the object needs to first be detected and located (
1,
5,
7). Owing to its simplicity of use in the soft tissue FBs in general, much focus has been placed on the value of radiograph (mainly for the radiopaque FB) and ultrasonography (mainly for the radiolucent FB), for detecting, locating, and guiding to remove the object (
1,
5-
9). There have been few studies in the literature that discuss the role of CT and MRI in the patients, especially with the radiopaque objects (
2-
4,
10). The risks including the surgical failure of FB removal are not low in our experience. With the migration risks and susceptibility artifacts secondary to metallic FB under MRI (
11,
12), the values of 3-dimensional (3D) CT, especially VAI, in complex FB retrieval from soft tissues are discussed in this study.
Go to :

MATERIALS AND METHODS
This study was approved by the Institutional Review Board of the authors' hospital. Four hundred and seventy-five patients (359 male and 116 female, aged from 15 to 69 years, median age 34 years), suffering from complex soft tissue radiopaque FB(s) for 3 hours to 11 years, as minimally diagnosed by the radiograph at the current hospital, were subjected to the study between January 2007 and December 2011. Of these, 76 patients also underwent ultrasound before CT examination; and 6 patients were failed to remove FB(s) through the open surgery.
All patients were referred for a 4-multidetector CT (MDCT) (GE LightSpeed Plus, Tokyo, Japan), because of the possible damage or abutting the vital tissues of their FB(s), including the non-enhanced and both the arterial and venous phase enhanced scan (300 mgI/mL Omnipaque, GE, 3 mL/s automatic venous injection with a LF power-injector, about 90 mL total volume). The CT scan was performed with a 2.5-7.5 mm section thickness, 1.2-2.5 mm reconstruction thickness, 50% overlap of the reconstructed sections, pitch 0.75 : 1, table speed 15 mm/rot, 80-120 kV, 200-250 mA, and a standard interpolator and algorithm. The imaging was post-processed at a workstation (GE AW 4.2). The volume-rendering (VR) software was used to obtain the images of multi-planar reformation (MPR), 3D reconstructions including static 3D VR (the lowest and highest threshold value were fixed at 100 and 600 Hounsfield unit [HU] respectively), 3D maximum intensity projection (MIP), and virtual anatomy imaging (VAI). The static 3D VR and MIP were namely the standard 3D images. VAI was reconstructed by sliding down the lowest threshold from 100 to -600 HU (the highest threshold value was fixed at 600 HU), using VR Opacity software listed in the VR software.
The imaging of the patients (n = 475 in every group) was grouped as Group A (axial and MPR images), B (standard 3D images with axial and MPR images), and C (VAI with axial and MPR images). The images were observed by at least one radiologist and one surgeon to assess: the type, shape, size, site, depth, number of FB and its surrounding structures, such as skin, superficial veins, lymph nodes, muscles, tendons, nerves, deep veins, arteries and bones. The interventional removability of FB depends mainly on the successful percutaneous removal with the C-arm fluoroscopy guidance or ultrasound, without any serious complications (
Table 1). The data was subjected to chi-square tests, with
p value < 0.05 indicating significant statistical difference.
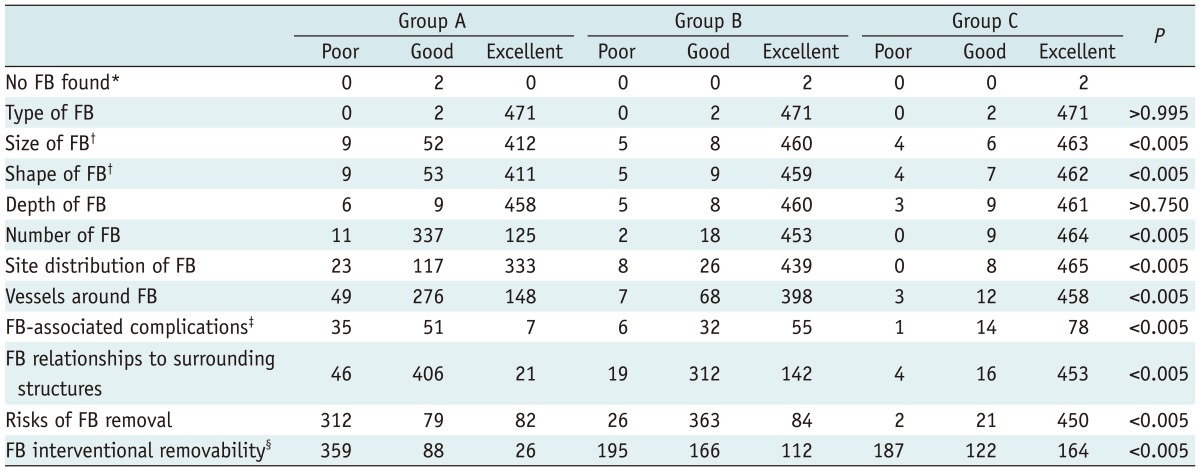
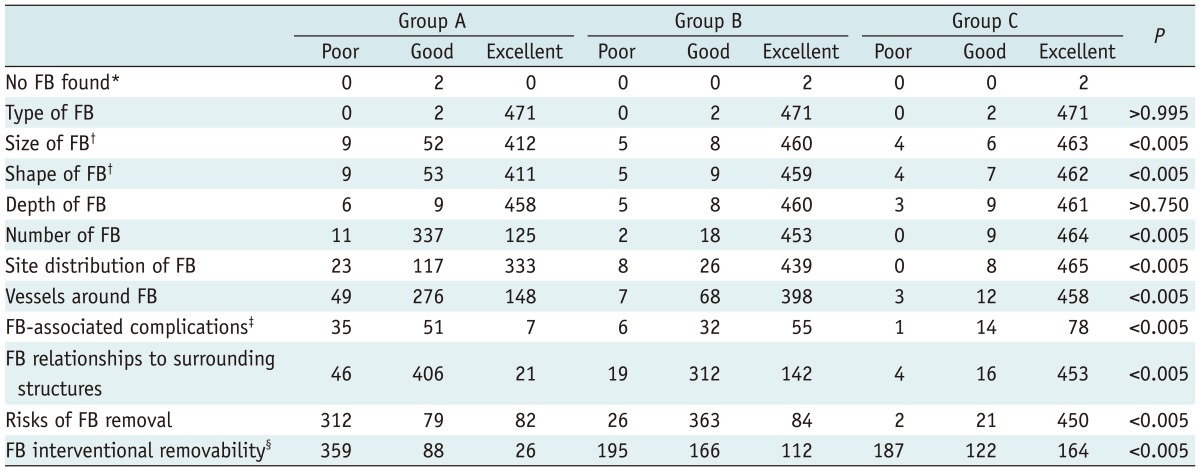
Table 1
Assessment Results of Each Group (n = 475)

Go to :

RESULTS
Simulating regional anatomy, VAI dynamically displayed the FB surrounding structures layer by layer from shallow skin, superficial vessels, superficial lymph node, muscles and tendons, gradually to deep vessels and bones on contrast-enhanced CT in full 360-degree vision. The VAI was different from routine 3D visualization, including the surface shaded display (SSD), MIP, VR, and virtual endoscopy as previously reported (
13,
14). Only the thick peripheral nervous structures, such as the ulnar nerve and radial nerve in scarpal canal, femoral nerve in groin, and sciatic nerve, common peroneal nerve, and tibial nerve in popliteal space, were 3D demonstrated on VAI. The arteries, deep vessels, and their complications shown on the contrast-enhanced VAI were not visualized clearly on the non-enhanced 3D CT, including VAI. The range of the lowest thresholds for the optimal display of the various structures was presented in
Table 2. The image of maximum intensity projection or translucent VR of radiopaque FB, including metallic FB embedded in soft tissues, was insufficient in the anatomical hierarchy details, especially lacking in showing the position relationship between the FB and its abutted structures. Only the opaque VR could be used effectively in the VAI of the soft-tissue FB.
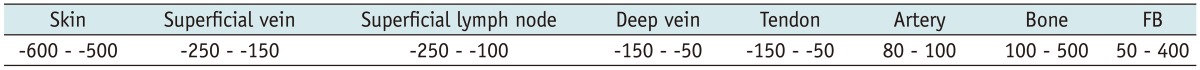
Table 2
Range of Lowest Thresholds for Optimal Display of Various Structures (Hounsfield unit)

The assessment results of each group were listed in
Table 1. Two (0.42%) of 475 patients had no FB shown on CT, including all 3D images proven later by the follow-up radiograph (
Fig. 1). In the shape, size, number, and site distribution of FB(s), Group A showed less accurately than Group B and Group C (
p < 0.005), but there was no significance between Group B and Group C (
p > 0.05). In revealing the vessels, as concerning the FB-associated complications (especially the vascular complications), the FB relationships to the surrounding structures, the FB interventional removability, and the risks of the removal treatment, Group C was more precise than Group B, while Group B was more precise than Group A (
p < 0.005). There was no significant difference in the evaluation of the FB type and depth from shallow skin among the 3 groups (
p > 0.05).
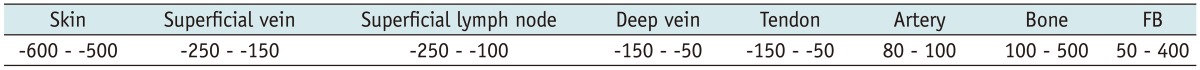
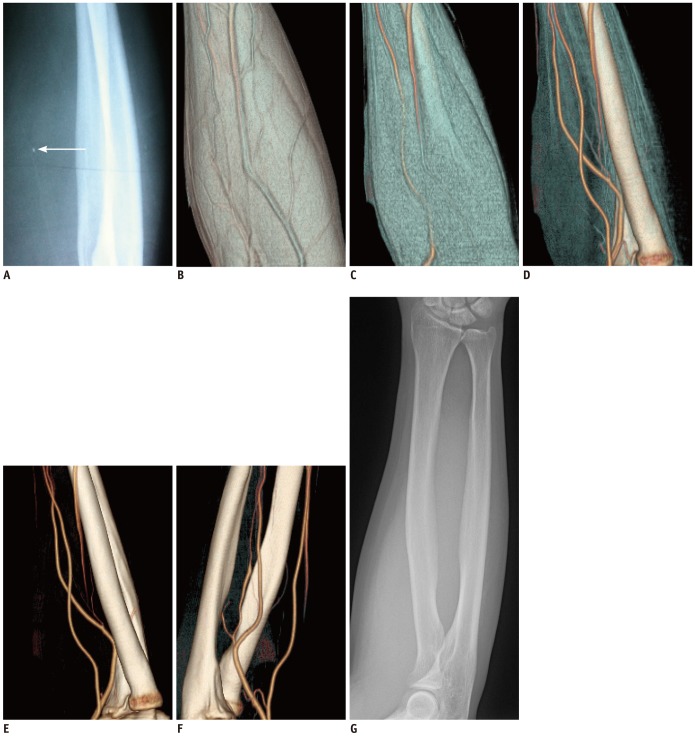
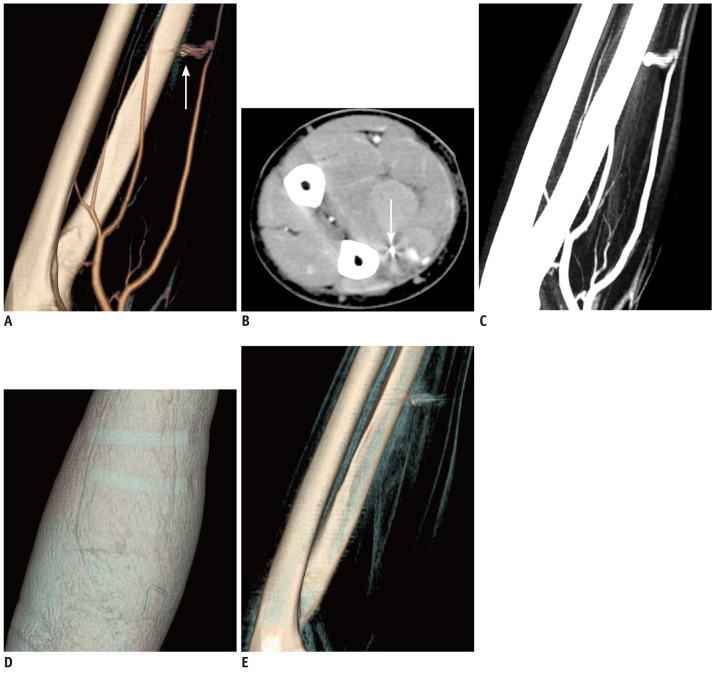
 | Fig. 1
False positive of soft-tissue FB detected by radiograph.
FB (arrow, 2 mm in diameter) in right forearm disappears 21 days after being diagnosed by radiograph (A) in 52-year-old male patient. 3D CT VAI shows no FB from superficial (B), muscles (C), tendons (D) to deep arteries and bones (E), and their rotating image (F). Subsequent radiograph (G) and follow up prove CT finds. FB = foreign body, 3D = 3-dimensional, VAI = virtual anatomy imaging

|
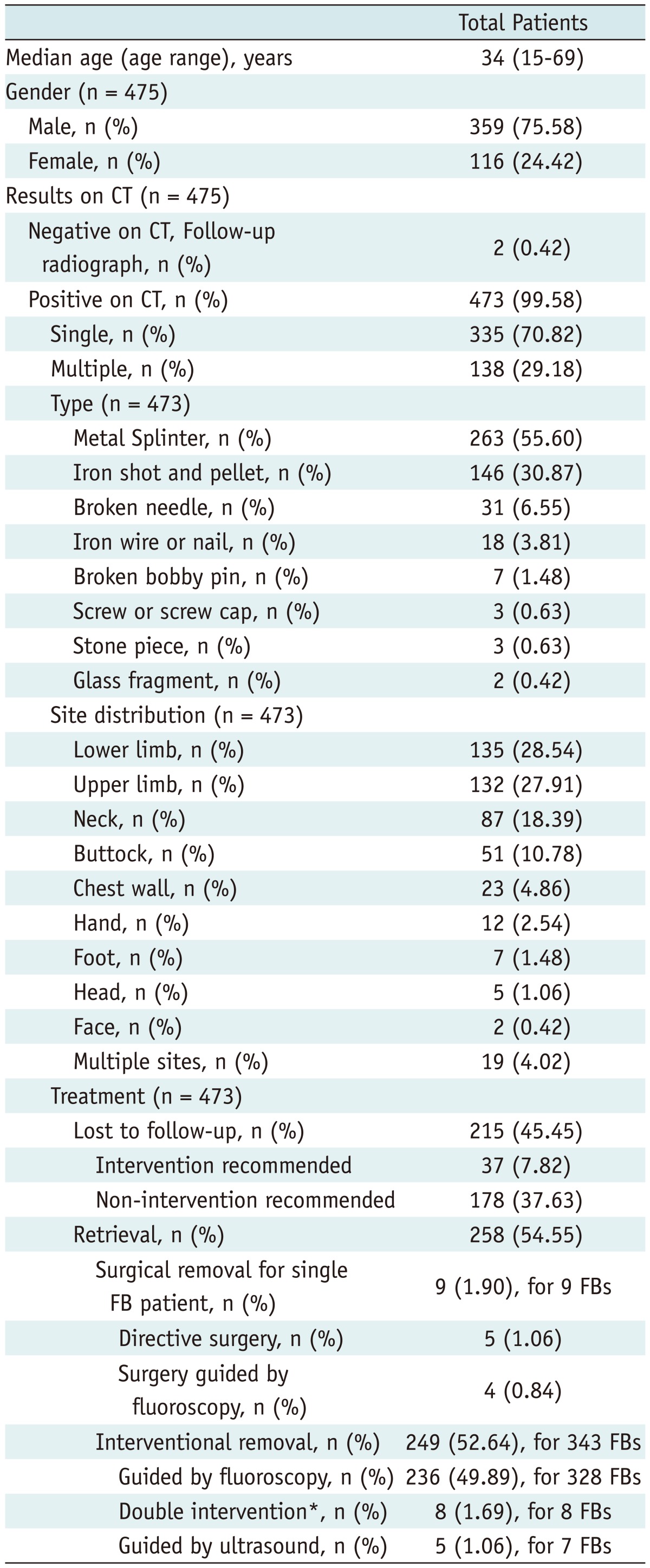
Based on the 3D CT, especially the enhanced 3D CT VAI, interventional removal in 286 (60.47%), as well as non-intervention in 187 (39.53%) of 473 patients with soft-tissue FB(s) were recommended. In 352 (56.50%) of 623 radiopaque FBs patients, 258 (54.55%) patients were accurately detected on 3D CT (the most up to 27 pieces in one patient; 1 mm to 15 mm and 1 mm to 10 mm in length and diameter), and the FBs were successfully removed by intervention (343 FBs) (
Fig. 2) or surgery (9 FBs) (
Fig. 3) without any sequelae. The other 215 (45.45%) patients with 271 FBs lost in follow-up, with their departure from the hospital. The baseline patient characteristics are summarized in
Table 3.
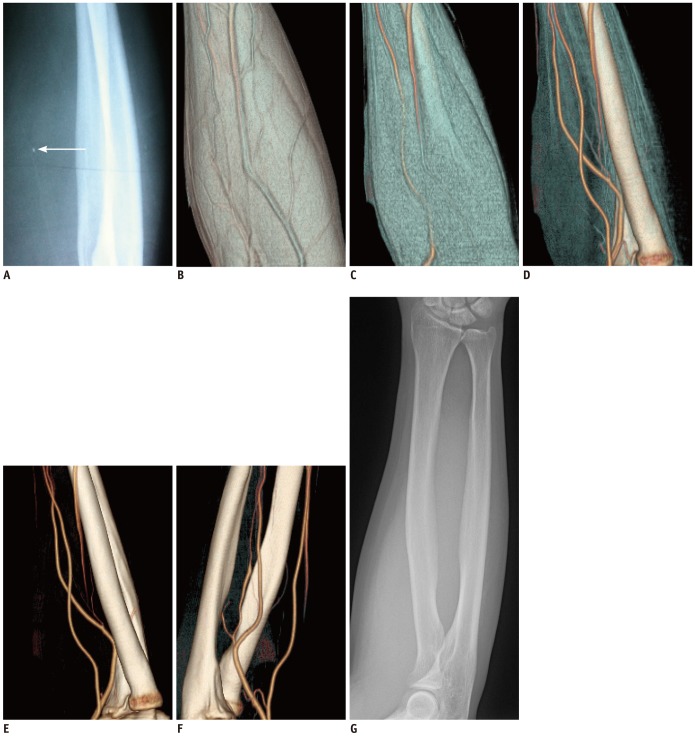
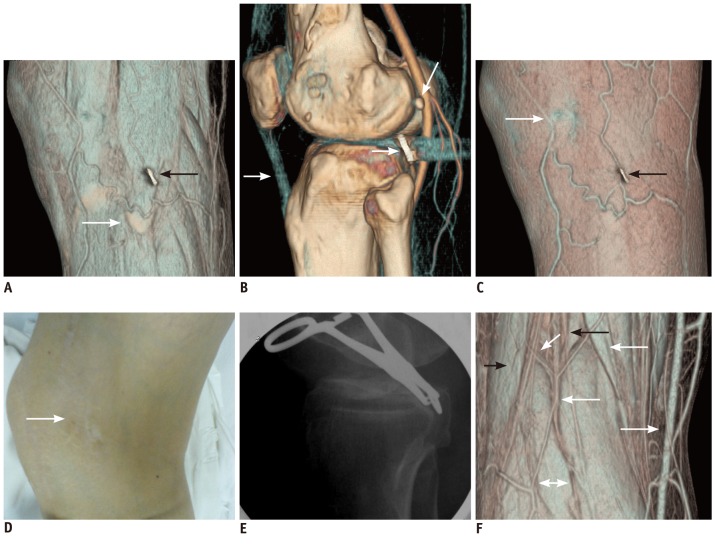
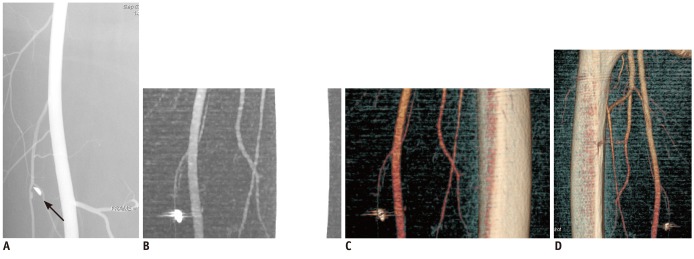
 | Fig. 2
Screw cap (10 mm in diameter and 1 mm thickness) fell off and remained in soft tissues around knee for 8 years, after internal fixation of left knee, in 50-year-old female patient.
Muscle view of VAI (A) clearly shows relationship of FB with fibular head (dovetail arrow) and superficial veins around knee, and damage to biceps femoris tendon (black arrow). Diameter, thickness of FB, and its minimal interval to popliteal artery and fibular head are visualized accurately on arterial view (B). Patellar ligament (white arrow) is clearly visible. Differentiation of sesamoidea (curving arrow) and FB (dovetail arrow) is noted differently here. Imprint of FB (black arrow), adjacent subcutaneous veins, and surgical scar (dashed arrow) are displayed clearly on superficial view (C) in accordance with actual conditions (D). Using Allis' forceps to clamp screw cap in its central hole, FB was removed successfully under guiding fluoroscopy (E) without any complications. Muscle view of popliteal space (F) 3D shows normal structures of biceps femoris tendon (black arrow), semitendinosus muscle (white arrow), gastrocnemius (left-right arrow), popliteal vein (dashed arrow), small saphenous vein (white dovetail arrow), common peroneal nerve (curving arrow), and tibial nerve (black dovetail arrow). FB = foreign body, 3D = 3-dimensional, VAI = virtual anatomy imaging

|
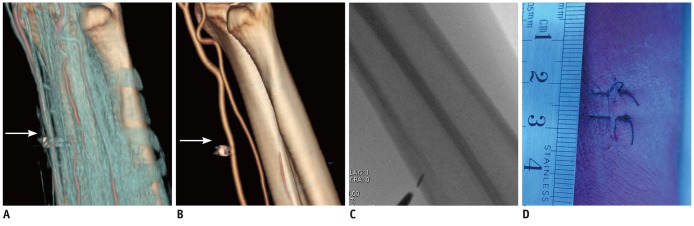 | Fig. 3
62-years-old male patient with soft-tissue injury in right forearm by metallic FB (arrow), adjacent to radial artery.
Key structures, especially vessels adjacent to FB, are situated only in one side and no vital vessels and other important structures are observed in its superficial side on tendon view image (A) and arterial view image (B) of VAI. Open incision is thus recommended, with fluoroscopic guiding, precise localization of object (C), and local anesthesia, for direct exposure of FB and its retrieval. Procedure left 2 cm suture in local skin (D); FB was removed successfully, and patient recovered without any sequelae. FB = foreign body, VAI = virtual anatomy imaging

|
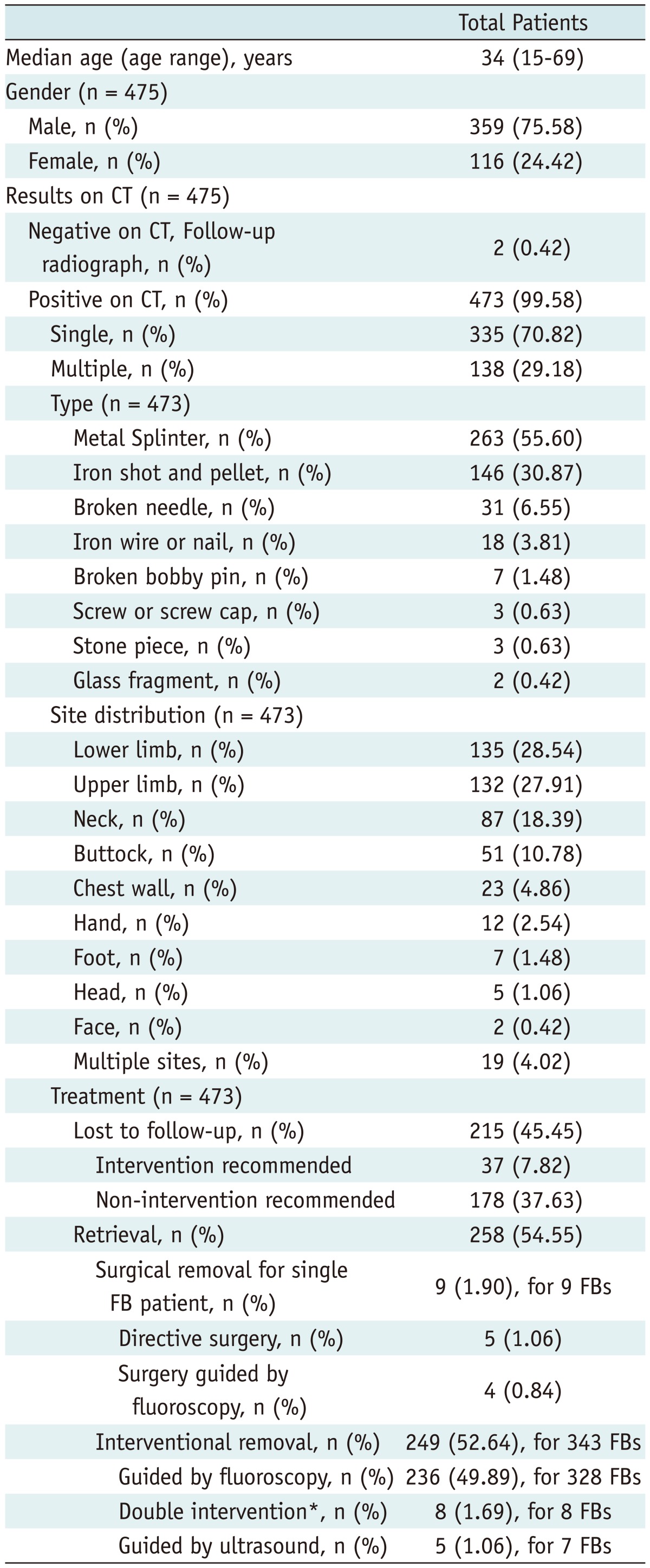
Table 3
Baseline Patient Characteristics

The non-interventional removal depended mainly on the FB-associated complications, such as pseudoaneurysm (8.56%, 16/187) (
Fig. 4), huge hematoma (17.11%, 32/187), large granuloma (14.97%, 28/187), large abscess (2.67%, 5/187), and less than 3 mm interval from the FB to the surrounding vital structures, such as the key vessels and nerves (50.80%, 95/187). Additionally, 11 (5.89%, 11/187) patients were not advocated intervention, because of the difficulties in the differential diagnosis of the arteriospasm and arterial laceration and contusion, due to the disappearance of the distal artery abutting the FB on the 3D CT. No FB-associated complications of artery fracture and arteriovenous fistula were found in this study, which were also the interventional FB removal contraindications. On the outward appearance and physical examination only, the treatment risks of the complicated soft-tissue FB were not found (
Fig. 4). There was one (12.50%, 1/8) false negative result of pseudoaneursym on the 3D CT, compared to DSA in 8 patients. Open surgical removal with a small incision under the fluoroscopic guidance and local anesthesia was recommended to some patients with single FB adjacent to the shallow blood vessels in one side only (
Fig. 3). Of the 187 patients who were recommended the non-interventional treatment, 178 (95.19%, 178/187) patients were lost in follow-up, while 9 (4.81%, 9/187) patients received the surgical removal.
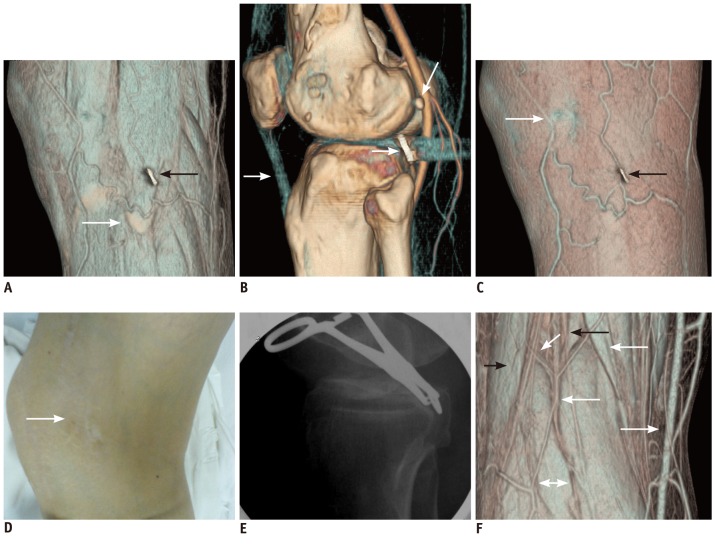
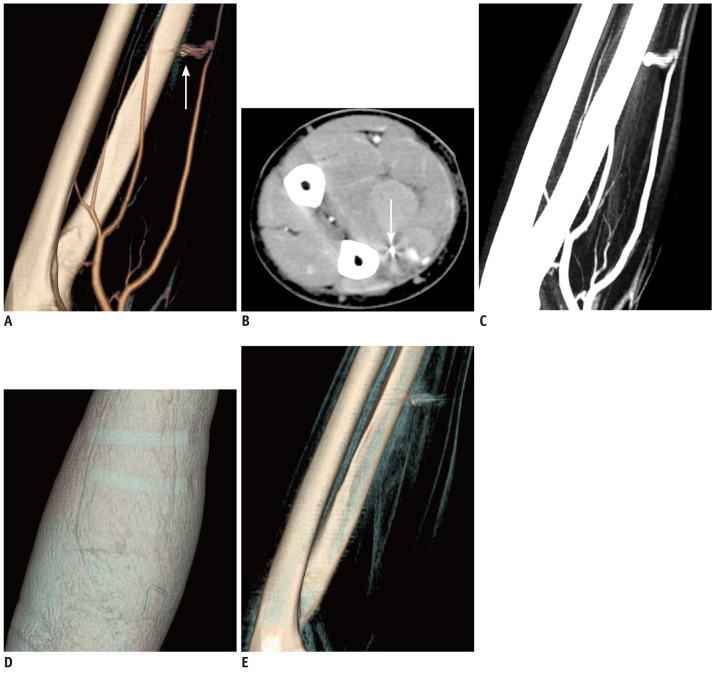 | Fig. 4
On outward apearance and physical examination only, FB-associated pseudoaneurysm can not be found.
45-year-old male patient with small steel patch (arrow) in left forearm and FB-associated vascular complications of irregular pseudoaneurysm and arteriospasm of distal radial artery, shown on VAI images of arterial view (A), which is contraindication of FB interventional removal. Pseudoaneurysm is not shown on axial contrast-enhanced CT images (B), and FB cannot be distinguished from pseudoaneursym on routine CT, even 3D MIP images (C). From appearance only, including skin view images (D) of VAI, FB, vascular injuring complications, and potential risks of retained FB, and in particular removal risks, cannot be discovered. On non-enhanced VAI (E), arteries, deep veins, and traumatic pseudoaneurysm shown on contrast-enhanced VAI (A, C) were not visualized clearly. FB = foreign body, VAI = virtual anatomy imaging, MIP = maximum intensity projection

|
For interventional removal, 249 (87.06%, 249/286) patients responded and received to be treated successfully with the guidance by fluoroscopy (97.99%, 244/249) (
Fig. 4) or ultrasound (2.01%, 5/249); and 37 (12.94%, 37/286) patients were lost in follow-up. Eight patients with small metal FB in the soft tissues of the limbs, within 2 mm interval of the surrounding vital blood vessels, accepted the new double interventional treatment of the fluoroscopy-guided percutaneous, both on the soft-tissue and vascular intervention of the foreign body extraction from the soft tissues, without any serious intervention-associated complications. One of the eight patients had a FB-associated traumatic pseudoaneurysm (3 × 2 × 1 mm in size), clarified by the pre-intervention angiography but missed on the 3D CT (
Fig. 5). All of the interventional removal patients recovered without any sequelae.
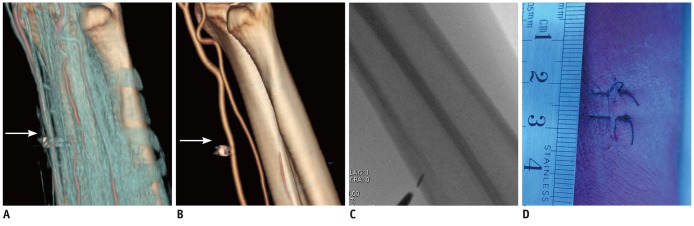
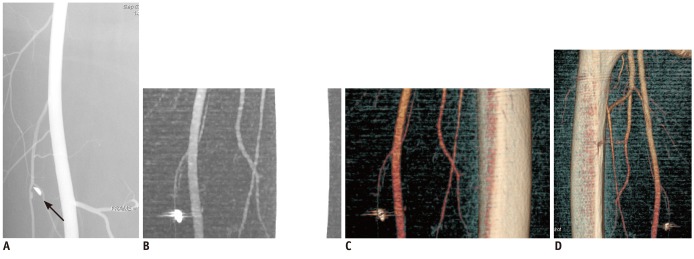 | Fig. 5
False negative of FB-associated traumatic pseudoaneurysm on 3D CT VAI.
40-years-old male patient with metallic soft-tissue FB in his left thigh and small FB-associated traumatic pseudoaneurysm (arrow, 2 × 3 × 1 mm in size) shown in FB adjacent branch femoral artery on angiograms (A). 3D MIP (B) and VAI with rotation and threshold adjusting (C, D) show no pseudoaneurysm near FB arteries. Sharp shape of FB is shown as obtuse on 3D CT. FB = foreign body, 3D = 3-dimensional, VAI = virtual anatomy imaging, MIP = maximum intensity projection

|
Go to :

DISCUSSION
Diagnosis and imaging-guided FB extraction from the soft tissues is not a new idea. This research has studied in detail on the improvement of the complex patients by using 3D CT, especially the 3D contrast-enhanced CT VAI. As seen in this study, the ordinary imaging, including radiograph and ultrasound, is often sufficient in the identification of the FB-associated complications, such as arteriospasm, vascular laceration and contusion, pseudoaneurysm, hematoma, granuloma, and abscess in deep soft tissues (
2,
3,
14). This study showed that 3D CT, especially the 3D enhanced CT VAI, revealed accurately the FB-associated complications, in particular the vascular complications and the FB interventional removability, along with the FB size, number, shape, and characteristics. Such functionality was from its display of the FB surrounding structures layer by layer, simulating the regional anatomy. On the outward appearance and physical examination, the treatment risks of the complicated soft-tissue FB patient were usually not found. Based on the 3D CT findings, over 87% of the patients recommended to the interventional removal responded to be treated successfully with the guidance of fluoroscopy or ultrasound. Also recommended by 3D CT, some patients' FBs retained in soft tissues were removed successfully by open surgery with or without fluoroscopy guidance. With the accompanying high risk, the interventional removal was not recommended to the patients with the FB-associated complications revealed on 3D CT of pseudoaneurysm, huge hematoma, large granuloma, large abscess, or less than 3mm interval from the FB to its surrounding vital structures, such as the key vessels and nerves. The reason for the 4.81% of the patients, who were recommended to the non-interventional removal, having received surgery may be mainly related to the characterization of the aspects of the FB intervention of our hospital in China, and the patients having been lost in the follow-up, with their departure from the hospital. In this clinical trial, there was a false positive of soft-tissue FB in 0.42% patients as detected by the radiographs, and they were diagnosed correctly by the 3D CT. The results indicated that the 3D CT, especially VAI, was of great benefit to increasing the operator's goal and confidence for successfully removing the object(s). After reviewing the 3D CT images, the operator could determine the FB removal method, and even the definite path (
15). That all of the FB removal patients, with the routine interventional contraindications in some, recovered without any sequelae maybe from the benefits of the preoperative 3D CT, with its precise evaluation and indirect visualization of the vessels adjacent to FB by guidewire or catheter endovascular, positing accurately under the fluoroscopy.
There were several limitations of the 3D CT. Compared to DSA, it had higher false negative in the detection of small pseudoaneursym, and it showed incorrectly the obtuse replacing sharp shapes of the FB. These may be the limitations of 4-MDCT and FB artifacts and the partial volume effect. New advanced CT and image workstation would improve the depiction, and 3D CT VAI can now be realized by a simple workstation use. Application of this one-key technology of VR image threshold value conversion in the new CT makes VAI very convenient. Additionally, it is worth mentioning that the differential diagnosis of metal artifacts, sesamoidea, and persistent epiphysis should be noted. Relative hypo-density without metallic artifact is helpful to the diagnosis of sesamoidea and persistent epiphysis, compared to the metal FB. Also, it is important to review carefully the standard axial and MPR images preoperatively, especially in differential diagnosis of the FB artifacts (
16).
In summary, 3D CT, especially VAI, has great incremental values in the diagnosis and management of complex radiopaque FB extraction from the soft tissues, in particular in the assessment of the FB-associated complications, the FB removability, the removal method to be chosen, and the removal path to be determined. However, with the concern regarding the radiation hazard, 3D CT VAI is used as a routine protocol for evaluation of the deep soft tissue radiopaque FB in complicated cases, following the diagnosis with the radiography or/and ultrasound.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download