Abstract
Objective
To evaluate the clinical efficacy as well as long-term clinical outcomes of superselective microcoil embolization for lower gastrointestinal bleeding (LGIB).
Materials and Methods
Between 1997 and 2009, 26 patients with intended transcatheter embolotherapy for LGIB were retrospectively reviewed. Embolization was performed only when the catheter could be advanced to or distal to the mesenteric border of the bowel. The main purpose of our study was to assess technical success, recurrent bleeding rate and complications. We also evaluated the long-term clinical outcome, including late recurrent LGIB, bowel ischemia and the survival rate.
Results
Twenty-two bleeding sources were in the territory of superior mesenteric artery and four in the inferior mesenteric artery. Technical success was achieved in 22 patients (84.6%). The target vessel of embolization was vasa recta in seventeen patients and marginal artery in the remaining five patients. Early rebleeding occurred in two patients (7.7%) and bowel ischemia in two patients, of whom the embolized points were both at the marginal artery. Delayed recurrent bleeding (> 30 days) occurred in two angiodysplasia patients. Five patients (19.2%) died within the first 30 days of intervention. Long-term follow-up depicted estimated survival rates of 58.2 and 43.1% after one, and five years, respectively.
Conclusion
Transcatheter embolotherapy to treat LGIB is effective with low rebleeding and ischemic complications. Considering the advanced age and complex medical problems of these patients, the minimal invasive embolotherapy may be used as both a primary and potentially definitive treatment of LGIB.
The lower gastrointestinal bleeding (LGIB) is defined as hemorrhage below the ligament of Treitz and includes jejunal, ileal, colonic, and rectal bleeding. LGIB has an estimated annual incidence rate of 20.5 per 100000 population (1), and increases to 205.3/100000 in those aged more than 80 years (2). Although most of the bleeding episodes resolve spontaneously with conservative management, 10-15% of patients require some form of intervention (3). The reported overall mortality rate was 3.6%, while up to 25% of the bleeding began after hospitalization for another disease (1, 4). Recent studies dealing with transcatheter management of nonvariceal LGIB has revealed high technical success rates and low immediate post-procedural complications (2, 5-10). The incidence of embolization-induced bowel ischemia is reported to be between 5 and 15% of cases (11). Rebleeding after an initially successful therapeutic embolization occurs in 10-30% of cases within the first month (12). Although transcatheter embolization is now accepted as the salvage treatment of choice for acute bleeding from the LGI tract (13), the reports on long-term outcome of patients after embolization are still limited (2, 11, 14, 15). In this study, we represent our short-term clinical outcomes of superselective microcoil embolotherapy for LGIB, as well as the long-term durability of up to 72 months follow-up after embolotherapy.
From June 1997 to May 2009, twenty-six patients receiving attempted embolization for acute LGIB in our institute were retrospectively reviewed. There were nineteen men and seven women with the mean age of 69.1 years (range, 19-95 years). The cases with tumor bleeding were excluded in this study. Major co-morbidities included hypertension (n = 13), diabetes mellitus (n = 9), coronary artery disease (n = 3), renal insufficiency (n = 7), history of malignancy (n = 4) and cerebrovascular accident (n = 2). Multidetector computed tomography (MDCT) has been used as the screening modality for detecting LGIB at our hospital since 2002, and positive findings on MDCT were considered as the only indication for angiography. Before 2002, angiography was used to detect the bleeding source in patients with massive LGIB, whereas a nuclear medicine bleeding scan was used to detect chronic or minor bleeding. The use of colonoscopy for the evaluation of LGIB was at the clinicians' discretion. Thirteen in-patients, including five referred from the intensive care unit, and thirteen out-patients referred from the emergency unit were included in this study. Informed consent was obtained from each patient or from his/her family. Retrospective reviews of the medical records and images were approved by the institutional review board of our hospital.
By using the Seldinger's technique, the common femoral artery was punctured, and a 4 Fr RC-1 catheter (Cordis, Miami, FL, USA) was used for superior mesenteric artery catheterization, or a 4.1 Fr RIM catheter (Cook, Bloomington, IN, USA) for inferior mesenteric artery and/or internal iliac artery if necessary. Once the bleeding source was localized angiographically, superselective catheterization was then attempted with either a 2.7 Fr Progreat microcatheter (Terumo, Tokyo, Japan) or a 2.8 Fr Renegade microcatheter (Boston Scientific, Cork, Ireland) with a 0.018-inch guide wire coaxially advanced to the bleeding site. Attempts were made to position the catheter as close to the bleeding site as possible. Embolization was performed only when the catheter could be advanced to or distal to the mesenteric border of the bowel (at least to the marginal artery or in most cases to the vasa recta). Microcoils measuring 2 × 3 mm in dimension or straight microcoils of 5 or 10 mm in length (Cook, Bloomington, IN, USA) were deployed until no further arterial extravasation was seen. In cases in which superselective embolization was not possible due to small vessel tortuosity, or any other reasons, embolization was not performed, and the microcatheter was left in the mesenteric branching artery for the purpose of guidance during later surgical resection.
All the embolization procedures were performed by three interventionalists with 6-20 years of vascular interventional experience. Intravenous prophylactic antibiotics (cephacin, 1 g) before the procedures, and analgesics (fentanyl citrate, 100 µg, Janssen Pharmaceutica N.V.; Beerse, Belgium) during the procedure were administered to the patients. Oxygen saturation, blood pressure, and heart rate and rhythm were monitored in all the patients by noninvasive means.
After embolotherapy, all the patients were monitored closely for clinical signs and symptoms suggestive of ischemic complications (abdominal pain and/or tenderness, peritoneal signs, nausea, diarrhea, or fever) or recurrent bleeding until discharge or death. These clinical findings were supplemented by laboratory studies (white blood count, lactate level, hemoglobin level). Post-embolization CT follow-up (1-3 days after embolization) was done routinely in our early patients, and later only in patients with clinical suspicion of recurrent LGIB or bowel ischemia. The long-term outcome of the patients, specifically, incidence of rebleeding, mortality and procedure related complications were determined by chart review and/or telephone interview where appropriate. Colonoscpic examination was not a routine practice to be performed following embolotherapy in our unit.
Primary endpoints of our study were technical success, recurrent bleeding rate and the rate of minor and major complications, which are reported according to the guidelines of the Society of Interventional Radiology (16). Technical success was defined as immediate cessation of extravasation on repeat angiography at the end of the embolization procedure. Recurrent bleeding was defined as the stabilization of hemoglobin levels that required more than two units of packed red blood cells within 30 days after the procedure. Any lower GI rebleeding occurring later than 30 days after embolization was defined as delayed. Ischemic complications after embolization were defined as bowel ischemia or infarction that required surgery or as late focal bowel strictures requiring surgery or endoscopic repair. Asymptomatic, radiologic, or endoscopic signs of ischemic sequelae after embolization were not considered as postembolization complications.
Secondary endpoints of our study were to evaluate the long-term clinical outcome, including late recurrent LGIB, bowel ischemia and the survival rate.
Kaplan-Meier survival estimates were used to construct a curve for the overall mortality. Date of embolization was used as start date for the follow-up times. The difference in survival time between in- and out-patient groups was tested using Log rank test. A p value < 0.05 was considered statistically significant. All analyses were performed with the Statistical Package for the Social Sciences 17.0 statistical package (Chicago, IL, USA).
In this study, MDCT was used as the first line imaging modality to detect the sources of bleeding in twenty patients, whereas angiography (before 2002) was employed as the initial imaging evaluation in six patients. Of the six patients before 2002, four patients had the bleeding sources detected at the first angiography while in other two patients it was during the second angiography. Seven patients had received colonoscopic evaluation (Table 1) before angiography or MDCT study without any definite bleeding source, but with the identification of blood clot. Twenty-five of the twenty-six patients and nineteen of the twenty patients showed contrast extravasation on angiogram and on MDCT, respectively. The other patient, who demonstrated no contrast extravasation on both MDCT and angiography, was a patient of angiodysplasia in ileum with engorged submucosal vein. Twenty-two bleeding sources were in the territory of superior mesenteric artery (eleven in small bowel, nine in cecum or ascending colon and two in transverse colon), and four in the inferior mesenteric artery (one in sigmoid colon and three in rectum). The most common etiology of bleeding was presumed as diverticular disease (n = 13). The other causes of bleeding were considered to be angiodysplasia in four patients, ulcer in seven patients, and uncertain in two patients.
Technical success with immediate cessation of extravasation was achieved in twenty-two patients (84.6%). The target vessel of embolization was vasa recta (Fig. 1) in seventeen patients and marginal artery in five. Technical failure was encountered in three patients because of small torturous vessels and subsequently they were referred to surgical resection. The pathological diagnosis was diverticular bleeding in two patients, and ulcer bleeding in one. Another patient had inadvertently induced vascular spasm during selective catheterization but with successful control of the bleeding. Early rebleeding after an initial successful embolotherapy occurred in two patients (7.7%). One was a 61 year-old female patient with corrosive injury after gastrectomy. Contrast extravasation at the proximal jejunum on superior mesenteric artery angiograms was noted. Successful embolization with straight microcoils was obtained initially, but rebleeding from another nearby vasa recta was noted a week later (Fig. 2). Subsequently, she underwent another successful embolization. No recurrent bleeding occurred in this patient, but unfortunately, this patient died 1.5 months later due to multi-organ failure. The other patient had a new focus of bleeding at hepatic flexure of the ascending colon as seen in MDCT images 5 days after the initial successful embolotherapy for the bleeding at the cecum. He received conservative management and died of sepsis 28 days after the embolotherapy.
Post-embolizatin abdominal CT images were followed in thirteen patients. One was for confirmation of a jejunal tumor growth (leiomyoma) adjacent to the embolized bleeding source, two for recurrent LGIB, four for clinical complaints of abdominal pain, and six for abdominal surveillance in our early patients. Normal or mild thickening of the bowel wall at the embolized bowel segments was found in nine patients, moderate bowel wall thickening in two patients, and CT evidence of bowel ischemia in two patients, of whom the embolized points were both at the marginal artery (Fig. 3).
Five patients eventually underwent surgical resection in this study, including the three patients, in whom embolotherapy was a failure. One patient had a hypervascular tumor stain at the adjacent bowel segment, which was incidentally found on the angiograms. He received elective surgery 11 days after the initial embolization with the pathological diagnosis of a leiomyoma of the jejunum. A healed shallow mucosal erosion was also noted at the previously embolized site. The other patient had the complication of bowel ischemia noted a day after the embolotherapy and thus underwent right hemicolectomy with uneventful clinical course.
Five of the twenty-six patients (19.2%) died within the first 30 days of intervention, three following surgery and two following embolization. All the three patients underwent urgent surgical resection after failed embolotherapy, but died at 1, 7 and 18 days, respectively after the operation. Of the two successfully embolized patients, one patient with complications of bowel ischemia had bowel perforation with localized abscess formation. No surgical intervention was done because of poor general condition. Consequently, the patient died of sepsis 46 days after the initial embolization. The other patient, an 87 years old man, died during sleep at midnight 2 days after successful embolotherapy without any clinical symptoms or signs of ischemic bowel or other clinical complaints.
More than 30 days clinical follow-up was available in 21 patients with an average follow-up time of 21.9 months (range, 1-72 months). Two patients (9.5%) experienced further bleeding, which was sufficient to warrant hospital admission. Both of them were angiodysplasia patients (Fig. 4) with re-admission to hospital at 5- and 8-months, respectively following the initial embolotherapy. They were haemodynamically stable and treated nonoperatively. None but one of the twenty-one patients had clinical symptoms or signs of bowel stricture or obstruction. Seven patients died with follow-up period ranging from 1.5-47 months. One was attributed to the ischemic complication. The others were considered not to be related to the LGIB. Five patients remained alive (follow up range, 10-72 months) and nine patients were lost to follow up (follow up range, 1-26 months). The overall survival rates in the twenty-six intended embolized patients and in the twenty-one patients with survival for more than 30 days were plotted in the Kaplan-Meier estimate graphic (Fig. 5). The estimated percentage survival (± standard error) after 1 year was 58.2 ± 10.3% and 72.0 ± 10.7%, respectively and after 5 years were 43.1 ± 12.1% and 53.4 ± 14.1%, respectively. As in the cases of in-patients and out-patients, the estimated survival time (± standard error) was 21.2 ± 7.6 months and 49.1 ± 9.5 months, respectively. Generally, there is a trend of better survival time for out-patient group, however, no statistical significance was observed (p = 0.133).
Although most of the LGIB resolves spontaneously, a significant portion may become life-threatening. The patients with LGIB are often of older age with multiple medical problems and are commonly taking anticoagulants, antiplatelet agents or both, which further contribute in complicating their management (14). The therapeutic options include endoscopy, surgery, vasopressin infusion, and transcatheter embolization. Endoscopy is often the first method that is used to investigate and treat LGIB. Failure of endoscopic diagnosis and therapy (up to 32%) may occur as a result of massive bleeding, which limits precise localization of the site of hemorrhage (17, 18). In addition, most sources of bleeding in the small bowel are not accessible via a colonoscopy or push enteroscopy. Surgical treatment is typically definitive, but is associated with high mortality rates of 10%, and up to 36% in emergent cases (6, 19, 20). The overall morbidity in patients who present with massive LGIB exceeds 15-20% and increases to 20-50% in those who require surgery on a semi-urgent basis (21). Vasopressin infusion is labor-intensive, requiring an intensive care admission with high rates of cardiovascular complication, and with rebleeding rate of 36-50% (22, 23). As most of these patients are elderly with co-morbid cardiovascular disease, the use of vasopressin is hazardous because systemic side effects including hypotension, arrhythmias, angina and cardiac arrest have previously been documented (22-24).
Intra-arterial embolotherapy of LGI bleeding was first introduced by Bookstein et al. in 1974 (25). Because of the relatively poor collateral blood supply in the LGI tract, the safety of embolotherapy had been a matter of concern previously with reported ischemic complications in up to 33% of patients in early series (25-27). Advancements in microcatheter technology have enabled super-selective catheterization and embolization of distal arteries smaller than 1 mm in diameter distal to the mesenteric border, thus minimizing the resulting ischemia and clinically significant infarction. As reported, the technical success of embolotherapy for LGIB ranged from 69-100% (5-10, 12, 20, 28). Vascular spasm, vascular distortion and prior surgery are among the commonest causes of technical failure. In most of the reported series, the target artery of embolization for LGIB was the vasa recta. However, some embolizations were performed within the marginal artery or more proximally due to technical difficulty. In our series, we had the technical success of 84.6% (22/26 patients) with embolization of the vasa recta in seventeen patients and marginal artery in five, which were comparable to those of previous reports.
Among the various embolizers for LGIB, we prefer to use microcoils. The advantages of using microcoils includes the ability to be well visualized under direct fluoroscopy, avoiding particulate reflux (15), and fulfilling the objective of decreasing the perfusion pressure while allowing enough collateral flow to preclude infarction (6). In most of the institutes, the embolizer used is spiral type microcoil with the size ranging from 2 × 3-5 mm, and a stretched length of 22-42 mm (6, 29). But this size of spiral type microcoils usually cannot loop its shape completely in the very small vasa recta, and that part of the stretched microcoil may compromise the flow in the marginal artery and partial recanalization of the embolized artery might be possible. That is the reason we prefer to use straight microcoils (5-10 mm in length) in the vasa recta, so that a complete flow blockage can be achieved without the possible flow compromise in the marginal artery. In the case of other embolic agents, small particles of polyvinyl alcohol or liquid cyanoacrylates may reach intramural circulation beyond the level of collateralization or may reflux into non-target arteries (29). Thereafter, we recommend that unless the microcatheter cannot reach the vasa recta, the microcoils, especially of the straight type, should be the first choice for LGI embolotherapy.
Early rebleeding (< 30 days) after an initial successful embolotherapy is reported to range from 10-30% (2, 6-10, 30, 31). The rate of early re-bleeding in our patients was 7.7% (two patients). Both of them had a new focus of bleeding source. It is unclear if the early rebleeding cases in other series were due to recanalization of the embolized artery or a new bleeding focus, since it is possible that an unlooped stretched spiral type microcoil will recanalize. The two patients with late rebleeding in our series were both patients of angiodysplasia. The higher incidence of rebleeding in patients with angiodysplasia is not unexpected because of the presence of multiple feeding arteries (32) or multifocal lesions. Peck et al. (33) had reported that rebleeding occurred in 75% (3/4) of cecal angiodysplasia cases after embolizations. The embolotherapy for angiodysplasia might not be as responsive to embolotherapy as bleeding from other causes such as diverticulum or ulcer/erosion.
Bowel ischemia or infarction after embolotherapy for LGIB has been observed in 0-22% (5-9, 11, 19, 27, 28). In our series, ischemic bowel was complicated in 7.7% cases (two patients), which was in the range of literature reports. Notably, both of the two ischemic bowels occurred with embolization involving the marginal artery, while none was reported in patients with embolization of the vasa recta. Thus, we recommend the performance of embolization for LGI bleeding in the vasa recta. Embolization of the marginal artery may carry a higher risk of ischemic complication. Cynamon et al. (34) had proposed a technique of artificially induced vessel spasm to treat LGIB. It was also the experience of ours and Funaki et al.'s (6) that inadvertently induced vessel spasm had successfully controlled the LGIB clinically. Thereafter, for patients with technical difficulty of embolization at the vasa recta, artificially induced vessel spasm may be an ideal alternative.
Long-term follow-up in our series up to 72 months has shown that superselective microcoil embolization for LGIB has a low recurrent delayed bleeding or significant complication sequel, which was comparable to the previous reports, which demonstrated 5% of delayed bleeding (11) and 1.9% of chronic colonic stricture (14). Koh et al. (2), in a mean follow-up period of 12 months, reported that 14.7% of patients required surgical treatment to address the diseased bowel after successful embolization. In our series, except for a single case, which had complications along with bowel ischemia and died 46 days after the initial embolotherapy, none of the other twenty patients who had follow-up period longer than 30 days required surgical treatment. This suggests that successful embolization need not necessarily be followed by elective bowel resection. The overall survival rates of our twenty-six intended embolotherapy patients at 1 and 5 years were 58% and 43%, respectively. The survival rates increased to 72% and 53%, respectively in patients who survived for more than 30 days, which was comparable to the results (71% and 51%) shown in Maleux's series (11). The encouraging survival data, considering the advanced age and complex medical problems of these patients (nearly 20% of patients died within 30 days), it may imply that the minimally invasive transcatheter embolotherapy can be considered as both a primary and potentially definitive treatment for life threatening LGIB.
Several limitations of this study can be identified. First, this is a retrospective, monocenter analysis with small patient number. Small patient number may be the reason for showing only a trend of better survival time (21 months vs. 49 months), but not reaching statistical significance, between the in- and out-patient groups. Second, the decision to perform embolotherapy for LGIB rather than surgery was made based on a discussion between the interventional radiologist and clinicians without a clear medical protocol to be followed. Third, as no regular colonoscopic follow-up after embolization in our patients was done, the full extent of ischemic complications may be likely underestimated. However, any undiagnosed complications that are clinically asymptomatic in the elderly population with extensive comorbidity are of debatable significance. Finally, the overall survival outcome is not only determined by the embolotherapy but also by the medical treatment of all the comorbidities that these patients are suffering from, and the variable follow-up as well as the retrospective data collection limits the clinical inferences that can be drawn from this data.
In conclusion, superselective microcoil embolization is a safe and efficacious modality in the management of acute LGIB. It might be of great benefits for critical patients, if urgent surgical resection is required. The treatment can also be considered as a definitive treatment for stable patients without the need for further surgical resection.
Figures and Tables
 | Fig. 136-year-old man with bleeding jejuna ulcer.
A. CT angiography showing contrast extravasation (arrow), indicating active bleeding in the jejunum. B. Confirmation of contrast extravasation (arrow) in jejunum based on superior mesenteric artery angiogram. C. Bowel had moved to left upper abdomen during superselective catheterization. Arrow: contrast extravasation. D. Two straight microcoils (arrow) were placed in vasa recta. Immediate follow-up angiogram revealed no residual contrast extravasation. Patient is uneventful without recurrent lower gastrointestinal bleeding until end of study for 72-month follow up.
|
 | Fig. 261-year-old female with corrosive injury post gastrectomy.
A. Superior meaenteric artery angiogram showing contrast extravasation (arrow) at proximal jejunum. B. After straight microcoils (arrow) embolization, no residual contrast extravasation on follow-up angiogram can be identified. C. Recurrent bleeding occurred 7 days after initial successful embolization. SMA angiogram showing contrast extravasation from another vasa recta branch (arrow). Previously embolized branch was occluded (curved arrow). D. After another microcoils embolization (arrow), no residual contrast extravasation can be identified on follow-up angiogram. No recurrent bleeding occurred in this patient, but unfortunately patient died due to multi-organ failure 1.5 months later.
|
 | Fig. 366-year-old man with cecal bleeding.
A. Superior mesenteric artery angiogram showing contrast extravasation (arrow) in cecum. B. Superselective angiograms showing large amount of contrast extravasation (arrow) in cecum. C. 2 × 3 mm tornado microcoil (arrow) was placed in marginal artery with successful cessation of bleeding. D. Marked wall thickening of cecum (arrow) was noted on follow-up CT image 3 days after embolization. Abscess formation in pericecal (curved arrow) and subcutaneous region (arrow head) was also noted.
|
 | Fig. 472-year-old female with angiodysplasia.
A. MDCT showing early opacification of right mesenteric veins (arrow) and segmental engorged submucosal vein (curved arrow) at distal ileum. No contrast extravasation on MDCT images can be identified. B. On superior mesenteric artery angiograms, no contrast extravasation can be identified but enlarged vascular tufts (arrow) in distal ileum are evident. C. Engorged submucosal vein (arrow) of distal ileum is also demonstrated in late arterial phase. D. After superselective microcoil embolization (arrow), follow-up angiograms showed disappearance of enlarged supplying artery and submucosal vein. MDCT = multidetector computed tomography
|
 | Fig. 5Overall survival rates in twenty-six intended embolized patients and in twenty-one patients with survival for more than 30 days. |
Table 1
Basic Demographics and Clinical Outcomes of the Twenty-Six Patients
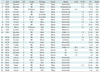
Note.- S/A = sex/age, I/O = in-/out-patient, -scope = colonoscope, 30-M = 30 days mortality, FU CT = follow-up CT, A-colon = ascending colon, A-loop = afferent loop, ND = not done, H-flexture = hepatic flexure, 30/45 cm = 30/45 cm above the anal verge, Dvtcm = diverticulum, AGD = angiodysplasia, Marg = marginal artery, Recta = vasa recta, Rebld = rebleeding, Op = operation, Lfu = lost to follow up, Exp = expired, m = months, d = days
References
1. Longstreth GF. Epidemiology and outcome of patients hospitalized with acute lower gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol. 1997. 92:419–424.
2. Koh DC, Luchtefeld MA, Kim DG, Knox MF, Fedeson BC, Vanerp JS, et al. Efficacy of transarterial embolization as definitive treatment in lower gastrointestinal bleeding. Colorectal Dis. 2009. 11:53–59.
3. Billingham RP. The conundrum of lower gastrointestinal bleeding. Surg Clin North Am. 1997. 77:241–252.
4. Peter DJ, Dougherty JM. Evaluation of the patient with gastrointestinal bleeding: an evidence based approach. Emerg Med Clin North Am. 1999. 17:239–261. x
5. Gordon RL, Ahl KL, Kerlan RK, Wilson MW, LaBerge JM, Sandhu JS, et al. Selective arterial embolization for the control of lower gastrointestinal bleeding. Am J Surg. 1997. 174:24–28.
6. Funaki B, Kostelic JK, Lorenz J, Ha TV, Yip DL, Rosenblum JD, et al. Superselective microcoil embolization of colonic hemorrhage. AJR Am J Roentgenol. 2001. 177:829–836.
7. Bandi R, Shetty PC, Sharma RP, Burke TH, Burke MW, Kastan D. Superselective arterial embolization for the treatment of lower gastrointestinal hemorrhage. J Vasc Interv Radiol. 2001. 12:1399–1405.
8. Sheth R, Someshwar V, Warawdekar G. Treatment of acute lower gastrointestinal hemorrhage by superselective transcatheter embolization. Indian J Gastroenterol. 2006. 25:290–294.
9. Defreyne L, Vanlangenhove P, De Vos M, Pattyn P, Van Maele G, Decruyenaere J, et al. Embolization as a first approach with endoscopically unmanageable acute non variceal gastrointestinal hemorrhage. Radiology. 2001. 218:739–748.
10. d'Othée BJ, Surapaneni P, Rabkin D, Nasser I, Clouse M. Microcoil embolization for acute lower gastrointestinal bleeding. Cardiovasc Intervent Radiol. 2006. 29:49–58.
11. Maleux G, Roeflaer F, Heye S, Vandersmissen J, Vliegen AS, Demedts I, et al. Long-term outcome of transcatheter embolotherapy for acute lower gastrointestinal hemorrhage. Am J Gastroenterol. 2009. 104:2042–2046.
12. Weldon DT, Burke SJ, Sun S, Mimura H, Golzarian J. Interventional management of lower gastrointestinal bleeding. Eur Radiol. 2008. 18:857–867.
13. Loffroy R, Cercueil JP, Guiu B, Krausé D. Detection and localization of acute lower gastrointestinal bleeding prior to therapeutic endovascular embolization: a challenge! Am J Gastroenterol. 2009. 104:3108–3109. author reply 3109-3110.
14. Lipof T, Sardella WV, Bartus CM, Johnson KH, Vignati PV, Cohen JL. The efficacy and durability of super-selective embolization in the treatment of lower gastrointestinal bleeding. Dis Colon Rectum. 2008. 51:301–305.
15. Ahmed TM, Cowley JB, Robinson G, Hartley JE, Nicholson AA, Lim M, et al. Long term follow-up of transcatheter coil embolotherapy for major colonic haemorrhage. Colorectal Dis. 2010. 12:1013–1017.
16. Drooz AT, Lewis CA, Allen TE, Citron SJ, Cole PE, Freeman NJ, et al. Quality improvement guidelines for percutaneous transcatheter embolization. J Vasc Interv Radiol. 2003. 14(9 Pt 2):S237–S242.
17. Zuckerman GR, Prakash C. Acute lower intestinal bleeding: part I: clinical presentation and diagnosis. Gastrointest Endosc. 1998. 48:606–617.
18. Kwak HS, Han YM, Lee ST. The clinical outcomes of transcatheter microcoil embolization in patients with active lower gastrointestinal bleeding in the small bowel. Korean J Radiol. 2009. 10:391–397.
19. Leitman IM, Paull DE, Shires GT 3rd. Evaluation and management of massive lower gastrointestinal hemorrhage. Ann Surg. 1989. 209:175–180.
20. Kuo WT, Lee DE, Saad WE, Patel N, Sahler LG, Waldman DL. Superselective microcoil embolization for the treatment of lower gastrointestinal hemorrhage. J Vasc Interv Radiol. 2003. 14:1503–1509.
21. Khanna A, Ognibene SJ, Koniaris LG. Embolization as first-line therapy for diverticulosis-related massive lower gastrointestinal bleeding: evidence from a meta-analysis. J Gastrointest Surg. 2005. 9:343–352.
22. Darcy M. Treatment of lower gastrointestinal bleeding: vasopressin infusion versus embolization. J Vasc Interv Radiol. 2003. 14:535–543.
23. Browder W, Cerise EJ, Litwin MS. Impact of emergency angiography in massive lower gastrointestinal bleeding. Ann Surg. 1986. 204:530–536.
24. Sherman LM, Shenoy SS, Cerra FB. Selective intra-arterial vasopressin: clinical efficacy and complications. Ann Surg. 1979. 189:298–302.
25. Bookstein JJ, Chlosta EM, Foley D, Walter JF. Transcatheter hemostasis of gastrointestinal bleeding using modified autogenous clot. Radiology. 1974. 113:277–285.
26. Chuang VP, Wallace S, Zornoza J, Davis LJ. Transcatheter arterial occlusion in the management of rectosigmoidal bleeding. Radiology. 1979. 133(3 Pt 1):605–609.
27. Rosenkrantz H, Bookstein JJ, Rosen RJ, Goff WB 2nd, Healy JF. Postembolic colonic infarction. Radiology. 1982. 142:47–51.
28. Luchtefeld MA, Senagore AJ, Szomstein M, Fedeson B, Van Erp J, Rupp S. Evaluation of transarterial embolization for lower gastrointestinal bleeding. Dis Colon Rectum. 2000. 43:532–534.
29. Kickuth R, Rattunde H, Gschossmann J, Inderbitzin D, Ludwig K, Triller J. Acute lower gastrointestinal hemorrhage: minimally invasive management with microcatheter embolization. J Vasc Interv Radiol. 2008. 19:1289–1296.e2.
30. Pennoyer WP, Vignati PV, Cohen JL. Management of angiogram positive lower gastrointestinal hemorrhage: long term follow-up of non-operative treatments. Int J Colorectal Dis. 1996. 11:279–282.
31. Weldon DT, Burke SJ, Sun S, Mimura H, Golzarian J. Interventional management of lower gastrointestinal bleeding. Eur Radiol. 2008. 18:857–867.
32. Nicholson AA, Ettles DF, Hartley JE, Curzon I, Lee PW, Duthie GS, et al. Transcatheter coil embolotherapy: a safe and effective option for major colonic haemorrhage. Gut. 1998. 43:79–84.
33. Peck DJ, McLoughlin RF, Hughson MN, Rankin RN. Percutaneous embolotherapy of lower gastrointestinal hemorrhage. J Vasc Interv Radiol. 1998. 9:747–751.
34. Cynamon J, Atar E, Steiner A, Hoppenfeld BM, Jagust MB, Rosado M, et al. Catheter-induced vasospasm in the treatment of acute lower gastrointestinal bleeding. J Vasc Interv Radiol. 2003. 14(2 Pt 1):211–216.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download