Abstract
Objective
To analyze magnetic resonance imaging (MRI) findings of Müllerian remnants in young females clinically suspected of Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome in a primary amenorrhea workup.
Materials and Methods
Fifteen young females underwent multiplanar T2- and transverse T1-weighted MRI at either a 1.5T or 3.0T MR imager. Two gynecologic radiologists reached consensus decisions for the evaluation of Müllerian remnants, vagina, ovaries, and associated findings.
Results
All cases had bilateral uterine buds in the pelvic cavity, with unilateral cavitation in two cases. The buds had an average long-axis diameter of 2.64 ± 0.65 cm. In all cases, bilateral buds were connected with fibrous band-like structures. In 13 cases, the band-like structures converged at the midline or a paramedian triangular soft tissue lying above the bladder dome. The lower one-third of the vagina was identified in 14 cases. Fourteen cases showed bilateral normal ovaries near the uterine buds. One unilateral pelvic kidney, one unilateral renal agenesis, one mild scoliosis, and three lumbar sacralization cases were found as associated findings.
Mayer-Rokitansky-Küster-Hauser syndrome (MRKH) is a congenital Müllerian anomaly that affects 1 in 4000 females, ranking as the second most frequent cause of primary amenorrhea (1-5). The main characteristics of the syndrome are as follows: 1) absence or reduced development of the uterus and upper two-thirds of the vagina, 2) normal external genitalia, 3) functional ovaries, and, 4) normal karyotype for females (46, XX) (1-5). The syndrome is categorized into two types (Type I and II), depending on the presence of associated nongynecologic anomalies affecting the urinary tract, middle ear, and skeletal system (Klippel-Feil syndrome) (1-3, 5).
Affected individuals coping with the syndrome often seek gynecologic surgeons, as the syndrome has a significant influence on both the physical and psychosocial health of the women. The ultimate goal of the surgery is restoration of normal sexual function, while even reproduction may be possible if assisted techniques are performed (1, 5).
Prior to surgery, thorough evaluation of the exact anatomy is crucial for the best surgical outcome (6). Current imaging modalities widely used in clinical practice include laparoscopy and ultrasonography (USG) (2, 3). However, both methods have drawbacks in that laparoscopy is invasive while USG, although noninvasive, is often inconclusive (2, 3).
Despite many strengths of magnetic resonance imaging (MRI) in soft tissue imaging, descriptive MRI findings of Müllerian remnants in MRKH syndrome have not been sufficiently evaluated in the previous literature, although there have been a few case reports on leiomyomas developed in uterine buds (1, 2, 7-12).
The purpose of our study was to analyze MRI findings of Müllerian remnants in young women clinically suspected of MRKH syndrome in primary amenorrhea workup.
Our institutional review board approved this retrospective study and waived the requirement for informed consent. We retrospectively reviewed MR images of 20 consecutive female patients, who were referred to our institution under the suspicion of MRKH syndrome between February 2003 and July 2011. Five patients with MR images of poor quality or with those taken at outside hospitals were excluded.
The final cohort consisted of 15 patients (mean age, 23.7 years; age range, 14 to 51 years), who were clinically suspected of MRKH syndrome on the basis of the following clinical workups: 1) gynecological exam, 2) transvaginal or transrectal USG, 3) hormonal study, and 4) chromosomal analysis. In particular, all patients were genetically proven to be 46, XX on chromosomal analysis.
Magnetic resonance images were obtained for all patients either with a 1.5T (Sonata; Siemens, Erlangen, Germany) or 3.0T MR imager (Trio Tim; Siemens, Erlangen, Germany), using a pelvic phased-array coil.
All patients were examined in the supine position. After a localizer scan, a T1-weighted transverse fast spin-echo sequence of the upper abdomen was obtained with a TR/TE of 130.0/2.5 msec, an echo-train length of 1, a field of view of 35.0 × 28.4 cm, and a matrix of 320 × 208. Subsequently, T2-weighted transverse, coronal, and sagittal fast spin-echo sequences (TR/TE, 3230-4080/93 msec; echo-train length, 11; field of view, 22.0 × 22.0 cm; matrix, 512 × 307) and a T1-weighted transverse fast spin-echo sequence (TR/TE, 762/14 msec; echo-train length, 3; field of view, 22.0 × 22.0 cm; matrix, 512 × 307) were obtained from the aortic bifurcation to the symphysis pubis. Two acquisitions were performed with each sequence at a slice thickness of 5 mm and a gap of 1 mm. An antiperistaltic agent was not routinely administered.
Two experienced gynecologic radiologists (reader 1, with 5 years of experience and reader 2, with 17 years of experience) rendered consensus analysis of MR images for the following.
For analysis, Müllerian remnants were categorized into three structural components as follows: 1) uterine buds, 2) fibrous band-like structures connecting bilateral uterine buds, and 3) midline or paramedian triangular soft tissue. First, uterine buds were evaluated for the following: 1) presence (unilateral or bilateral) or absence, 2) location, 3) presence or absence of associated cavitation or mass, and 4) the longest diameter. The location was described as either pelvic or extrapelvic. Cavitation was considered to be present when uterine buds exhibited a target pattern - a central zone of increased signal intensity, surrounded by a middle zone of hypointensity, and an outer zone of medium to high signal intensity - on transverse T2-weighted images (T2WI) (3). The average value of the long axis diameters for uterine buds on transverse T2WI was calculated. Second, when bilateral uterine buds were present, the presence or absence of fibrous band-like structures connecting the buds was investigated. Third, midline or paramedian triangular soft tissue was evaluated for its presence or absence and location. In addition, relative T2 signal intensity of the triangular soft tissue was described as being hyperintense, isointense, or hypointense with respect to bilateral uterine buds.
The vagina was divided into two parts, upper two-thirds and lower one-third, in terms of their embryonic origins. The existence of the two parts of the vagina was separately investigated on sagittal T2WI.
Ovaries were analyzed for their existence, location, and associated mass. As for the location, both absolute - pelvic or extrapelvic - and relative locations with respect to bilateral uterine buds were evaluated.
The existence of associated renal and lumbosacral vertebral anomalies was studied. For vertebral anomalies, those known to be commonly associated with MRKH syndrome (1, 7), namely sacralization of the fifth lumbar vertebra, lumbarization of the first sacral vertebra, and scoliosis, were investigated. Additionally, the presence or absence of ascites was also noted.
Demonstrable normal uterine structure was absent in all cases (n = 15). All cases had bilateral uterine buds located in the pelvic cavity on each side of the lateral pelvic walls (Figs. 1A-C, 2). Unilateral cavitation was found in two cases, with one case showing prominent cavitation and thus having a morphology similar to a deformed unicornuate uterus (Fig. 2B). None of the cases showed an associated mass in the uterine bud. The average long axis diameter for the buds was 2.64 ± 0.65 cm. Fibrous band-like structures connecting bilateral uterine buds were present in all cases (Figs. 1B-D, 2B). In 87% (13/15) of the cases, a midline or paramedian triangular soft tissue was found at the convergence of the fibrous band-like structures: 85% (11/13) for the midline (Fig. 1E, F) vs. 15% (2/13) for the paramedian soft tissue. The triangular soft tissue lay above the bladder dome in all 13 cases and its relative T2 signal intensity with respect to bilateral uterine buds varied: hyperintensity in 23% (3/13), isointensity in 46% (6/13), and hypointensity in 31% (4/13).
The upper two-thirds of the vagina was absent in all cases, whereas the lower one-third of the vagina was present in 93% (14/15) of the cases (Fig. 1F).
All cases had bilateral ovaries, 93% (14/15) of which appeared normal with follicular development (Figs. 1G-I, 2C). As for the Müllerian remnants, they were all located in the pelvic cavity: 73% (11/15) abutting the uterine buds (Fig. 2C) vs. 27% (4/15) not abutting the buds (Fig. 1G-I). When abutting the buds, 73% (8/11) of the ovaries were located either superior or inferior to the buds (Fig. 2C), whereas 27% (3/11) of the ovaries were in the same plane as the buds. On the other hand, when not abutting the uterine buds, all of the ovaries were located either superior or inferior to the buds and were connected to the buds via bands of low T2 signal intensity (Fig. 1I). Incidental teratoma was found in one case.
Two cases had associated renal anomalies, unilateral ectopia in one case and unilateral agenesis in another. In the case of unilateral renal ectopia, the ectopic kidney was located in the pelvic cavity. Associated vertebral anomalies were found in four cases: sacralization of lumbar vertebra in three cases and mild scoliosis in one case. The case with mild scoliosis also showed unilateral agenesis of the right kidney. Ascites was observed in 53% (8/15) of the cases.
Principal findings of the present study can be summarized as follows: 1) Typical Müllerian remnants in MRKH syndrome consisted of three structural components, bilateral uterine buds, fibrous band-like structures, and midline triangular soft tissue, and 2) Bilateral uterine buds were connected by the fibrous band-like structures, which converged at the midline triangular soft tissue lying above the bladder dome (Fig. 3).
Earlier studies of MRKH syndrome including MRI findings comprised mostly case reports on leiomyomas developed in uterine buds. Jadoul et al. (10) reported a case of a large symptomatic myoma in one uterine bud, which was subsequently removed by laparoscopy. Similar reports on symptomatic uterine bud myomas which necessitated surgical intervention also followed (11, 12). In all of the studies, however, imaging based anatomical evaluation was not conducted extensively.
Only recently has MRI begun to be exploited as a noninvasive alternative for diagnostic laparoscopy in MRKH syndrome, despite its advantages in soft tissue imaging (3, 13). To evaluate the potential of MRI as the main preoperative diagnostic imaging modality in place of laparoscopy, Pompili et al. (3) assessed accuracy of MRI findings with respect to diagnostic laparoscopy as the gold standard. The authors performed descriptive analysis on 1) developmental status of the vaginal canal, Müllerian remnants, and ovaries, 2) ascites, and 3) renal anomalies. Their results revealed strong concordance between the MRI and laparoscopic findings, suggesting MRI as a powerful tool in diagnosis and anatomical evaluation of MRKH syndrome (3).
In contrast to the study by Pompili et al. (3), we analyzed anatomical anomalies in MRKH syndrome with a focus on MR findings of its Müllerian remnants. In most cases, bilateral uterine buds showed symmetry, except for one case with one of its uterine buds resembling a deformed unicornuate uterus due to prominent cavitation. The presence of cavitation was evident on MRI, allowing for differentiation of cavitated from non-cavitated ones with high conspicuity. Most importantly, we found that the presence of fibrous bands-like structures connecting bilateral uterine buds was another consistent imaging feature observed in MRKH syndrome. In the majority (87%) of our cases, the fibrous band-like structures converged at the midline or paramedian triangular soft tissue lying above the bladder dome. Both the fibrous band-like structures and triangular soft tissue were speculated to be also part of the Müllerian remnants and the variation in T2 signal intensity of the soft tissue could be attributable to varying degrees of the uterine aplasia. To the best of our knowledge, the presence of the fibrous band-like structures and triangular soft tissue has not yet been widely appreciated in the previous literature. There has been one case report by Lamarca et al. (2), which confirmed the presence of a midline fibrous band joining bilateral uterine buds on laparotomy.
As for the vagina, the lower one-third of the vagina was found in 93% of our cases, reflecting the difference in embryonic origins of the lower one-third of the vagina and other genital tracts including the uterus, cervix, and upper two-thirds of the vagina (7, 14). Moreover, even the lower vagina of budlike appearance, which may not be easily recognized at laparoscopy, could be clearly delineated on MRI.
Our study also demonstrated that MRI is advantageous in evaluation of the presence, location, and associated mass in the ovaries. The majority (93%) of our cases had normally developed bilateral ovaries, as expected from the difference in embryonic origins of the ovaries and uterus (7, 14). These results are in accordance with those of the previous studies (2, 3, 7-12, 15).
Additionally, MRI was shown to be effective in delineating associated renal and vertebral anomalies. Renal anomalies are known to be one of the common associated non-gynecologic anomalies in Type II MRKH syndrome, with their spectrum varying from renal ectopia (pelvic kidney) to agenesis (1, 3). One case of unilateral renal agenesis and one case of unilateral pelvic kidney were found in our study. Among the vertebral anomalies frequently associated with type II MRKH syndrome (1, 7), three cases (20%) of lumbar sacralization and one case (7%) of mild scoliosis were noted in our study. According to the previous literature, the renal and vertebral anomalies are known to occur only in type II MRKH syndrome, which is characterized by asymmetry of the uterine buds, ovarian anomalies, as well as other non-gynecologic anomalies involving cardiac and otologic systems (1, 7). In contrast to the findings of the previous literature, size asymmetry in the uterine buds or presence of ovarian anomalies was not evident in our cases.
Apart from the intrinsic limits of any retrospective study, a few other limitations of our study should be mentioned. First, the sample size was rather small to generalize our findings and thus further investigation including a larger population would be warranted. Second, all our cases lacked pathologic confirmation, as they did not have indications (such as endometriosis or myomas) for laparoscopic or surgical removal of the remnants. Third, MRIs of different units (1.5T and 3.0T) were used in the qualitative MR image analysis as the difference in magnetic field strength was speculated to have a minimal effect on delineating the anatomy; however, differences in signal to noise ratio and contrast resolution caused by the varying magnetic field strength might have slightly influenced our interpretations. Fourth, inclusion of one female patient who was first diagnosed as MRKH syndrome at the age of 51 caused minor inhomogeneity in the study population.
Despite these limitations, our results demonstrated the potential of using MRI as an alternative to diagnostic laparoscopy in depiction of the characteristic anatomical features of MRKH syndrome. Furthermore, MRI was shown to be capable of providing the anatomical information that could serve as a guide for the optimal surgical planning. For instance, cavitation within the uterine buds, whose presence has been associated with the cyclic pelvic pain prompting the surgical removal, was easily recognized on MRI with high conspicuity (3, 6). In addition, the presence of the lower one-third of the vagina on MRI, in conjunction with supporting gynecologic exam findings, could raise the possibility of neovaginal creation as a surgical option (3).
In conclusion, characteristic MRI findings of Müllerian remnants - non-visualization of a normal uterus and upper two-thirds of the vagina, along with the presence of bilateral uterine buds connected by the fibrous band-like structures, which converged at the midline triangular soft tissue lying above the bladder dome - may facilitate clinical diagnosis of MRKH syndrome and surgical planning.
Figures and Tables
 | Fig. 1Representative case of MRKH syndrome in 34-year-old woman.
A. On transverse T2WI, bilateral soft tissues suspected as uterine buds (thick arrows) are found on each side of lateral pelvic walls. B-E. Serial coronal T2WIs show fibrous band-like structures (B-D: thick arrows) connecting bilateral uterine buds (B, C: dotted arrows) and converging at midline soft tissue (E: arrowhead). F. On sagittal T2WI, instead of normal uterine structure, triangular soft tissue (thick arrow) is found at midline. Lower one-third of vagina appears normal (thin arrows). G-I. Bilateral ovaries (G, H: thick arrows) are also found in pelvic cavity and appear normal on transverse T2WI. Coronal T2WI shows low signal intensity band (I: thin arrow) between left ovary and uterine bud (right side not shown). MRKH = Mayer-Rokitansky-Küster-Hauser, T2WI = T2-weighted image
|
 | Fig. 2MRKH syndrome in 18-year-old woman.
A, B. Bilateral uterine buds (A, B: thick arrows) are connected only with fibrous band-like structures (B: arrowheads) on transverse T2WI. Prominent cavitation (B: thin arrow) is noted in right uterine bud. C. Coronal T2WI shows bilateral normal ovaries (thick arrows) abutting uterine buds (thin arrows) at superior aspect. MRKH = Mayer-Rokitansky-Küster-Hauser, T2WI = T2-weighted image
|
 | Fig. 3Schematic drawings of typical Müllerian remnants.
A. Fibrous band-like structures connecting bilateral uterine buds converge at midline triangular soft tissue. Cavitation may be present in uterine buds (shown as triangular area within left bud). Ovaries abutting uterine buds are also shown. B. Sagittal T2-weighted images shows triangular soft tissue lying above bladder dome. Soft tissue is continuous with vagina showing atrophy in upper two-thirds.
|
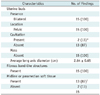
Table 2
Other MRI Findings of MRKH Syndrome

Note.- *Low signal intensity bands were found between bilateral ovaries and uterine buds, †Teratoma, ‡One case of unilateral ectopia and one case of unilateral agenesis, §Three cases of lumbar sacralization and one case of mild scoliosis. Case with mild scoliosis also showed unilateral agenesis of right kidney. MRKH = Mayer-Rokitansky-Küster-Hauser
References
1. Giusti S, Fruzzetti E, Perini D, Fruzzetti F, Giusti P, Bartolozzi C. Diagnosis of a variant of Mayer-Rokitansky-Kuster-Hauser syndrome: useful MRI findings. Abdom Imaging. 2011. 36:753–755.
2. Lamarca M, Navarro R, Ballesteros ME, García-Aguirre S, Conte MP, Duque JA. Leiomyomas in both uterine remnants in a woman with the Mayer-Rokitansky-Küster-Hauser syndrome. Fertil Steril. 2009. 91:931.e13–931.e15.
3. Pompili G, Munari A, Franceschelli G, Flor N, Meroni R, Frontino G, et al. Magnetic resonance imaging in the preoperative assessment of Mayer-Rokitansky-Kuster-Hauser syndrome. Radiol Med. 2009. 114:811–826.
4. Reinhold C, Hricak H, Forstner R, Ascher SM, Bret PM, Meyer WR, et al. Primary amenorrhea: evaluation with MR imaging. Radiology. 1997. 203:383–390.
5. Zhou JH, Sun J, Yang CB, Xie ZW, Shao WQ, Jin HM. Long-term outcomes of transvestibular vaginoplasty with pelvic peritoneum in 182 patients with Rokitansky's syndrome. Fertil Steril. 2010. 94:2281–2285.
6. Jurkiewicz B, Matuszewski L, Cisłak R, Rybak D. Rokitansky-Kustner-Hauser syndrome - a case report. Eur J Pediatr Surg. 2006. 16:135–137.
7. Chandiramani M, Gardiner CA, Padfield CJ, Ikhena SE. Mayer - Rokitansky - Kuster - Hauser syndrome. J Obstet Gynaecol. 2006. 26:603–606.
8. Deligeoroglou E, Kontoravdis A, Makrakis E, Christopoulos P, Kountouris A, Creatsas G. Development of leiomyomas on the uterine remnants of two women with Mayer-Rokitansky-Küster-Hauser syndrome. Fertil Steril. 2004. 81:1385–1387.
9. Govindarajan M, Rajan RS, Kalyanpur A, Ravikumar . Magnetic resonance imaging diagnosis of Mayer-Rokitansky-Kuster-Hauser syndrome. J Hum Reprod Sci. 2008. 1:83–85.
10. Jadoul P, Pirard C, Squifflet J, Smets M, Donnez J. Pelvic mass in a woman with Mayer-Rokitansky-Kuster-Hauser syndrome. Fertil Steril. 2004. 81:203–204.
11. Lanowska M, Favero G, Schneider A, Köhler C. Laparoscopy for differential diagnosis of a pelvic mass in a patient with Mayer-Rokitanski-Küster-Hauser (MRKH) syndrome. Fertil Steril. 2009. 91:931.e17–931.e18.
12. Papa G, Andreotti M, Giannubilo SR, Cesari R, Ceré I, Tranquilli AL. Case report and surgical solution for a voluminous uterine leiomyoma in a woman with complicated Mayer-Rokitansky-Küster-Hauser syndrome. Fertil Steril. 2008. 90:2014.e5–2014.e6.
13. Sönmezer M, Atabekoglu C, Dökmeci F. Laparoscopic excision of symmetric uterine remnants in a patient with mayer-rokitansky-küster-hauser syndrome. J Am Assoc Gynecol Laparosc. 2003. 10:409–411.
14. Chandler TM, Machan LS, Cooperberg PL, Harris AC, Chang SD. Mullerian duct anomalies: from diagnosis to intervention. Br J Radiol. 2009. 82:1034–1042.
15. Reichman DE, Laufer MR. Mayer-Rokitansky-Küster-Hauser syndrome: fertility counseling and treatment. Fertil Steril. 2010. 94:1941–1943.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download