Abstract
As recent advances in chemotherapy and surgical treatment have improved outcomes in patients with biliary cancers, the search for an optimal strategy for relief of their obstructive jaundice has become even more important. Without satisfactory relief of biliary obstruction, many patients would be ineligible for treatment. We review all prospective randomized trials and recent retrospective non-randomized studies for evidence that would support such a strategy. For distal malignant biliary obstruction, an optimal strategy would be insertion of metallic stents either endoscopically or percutaneously. Evidence shows that a metallic stent inserted percutaneously has better outcomes than plastic stents inserted endoscopically. For malignant hilar obstruction, percutaneous biliary drainage with or without metallic stents is preferred.
There is good evidence supporting the argument that endoscopic biliary drainage (EBD) is preferred to surgical bypass for biliary decompression in obstructive jaundice due to pancreatic cancer (1-3). This is not the case when it comes to choosing EBD or percutaneous biliary drainage (PBD) with or without stenting (PBDS) for relief of malignant biliary obstruction because few randomized, comparative studies exist. Differences in performance of EBD and PBD are even more clinically important now that effective treatment for biliary cancers has become available. For example, successful surgical resection (R0) for Klatskin tumors has increased from 13% to 60% in a 15 year period (4); surgical resection of Klatskin tumors offers the best treatment results with a median 5 year survival of 30% to 40% (5, 6). Equally important, advances in interventional radiology have enabled patients with to be upgraded unresectable Klatskin tumors on conventional grounds to resectable candidates. These patients have small future liver remnants which are stimulated to undergo compensatory hypertrophy with pre-operative portal vein embolization and biliary drainage (6). Even for patients with inoperable cholangiocarcinomas but eligible for chemotherapy, their median survival can be extended to 11.8 months with the combination of cisplatin and gemcitabine vs a period of less than 4.8 months in patients treated with gemcitabine alone (7). In short, satisfactory decompression of biliary obstruction is crucial for adequate symptomatic relief and for patients to benefit from modern treatment. How best to achieve this drainage has been, and continues to be, the primary concern for patients, physicians and other caregivers alike.
Both endoscopic and percutaneous methods of biliary decompression offer relief for malignant biliary obstruction; each has its own performance characteristics depending on the obstruction sites. This article examines the published evidence in support of the best strategy in managing malignant biliary obstruction.
A literature search for all prospective randomized trials comparing endoscopic and percutaneous biliary drainage was made. Retrospective, non-randomized comparative studies from 2000 to 2010 were also included. We limited the review to publications in English and excluded earlier studies as technical improvements in recent years have rendered them irrelevant to current interventional practices. We acknowledge that our search may be incomplete with but believe that we have captured the most important evidence.
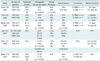
We identified two prospective randomized controlled trials (RCTs) comparing the outcomes of endoscopic and percutaneous biliary stenting in malignant biliary obstruction arising at the hilar region and distal common bile duct. (8, 9) We found only one RCT comparing the two methods in patients with gallbladder cancer causing hilar obstruction (10) Since 2000, three retrospective nonrandomized comparative studies were published (11-13) - one on pre-operative biliary drainage (13) and the other 2 on palliation of Klatskin tumors. (11, 12) One of the palliative studies compared metallic stent insertion by both methods. (12) The study design, inclusion and exclusion criteria, sites of obstruction and types of intervention are detailed in Table 1. The treatment outcomes including efficacy, complications, 30 day mortality, conversion from one intervention to the other, and patient survival are tabulated in Table 2.
The 2 prospective randomized trials (8, 9) comparing EBD vs PBDS in hilar and distal biliary obstruction were published 15 years apart, and reflect the advances made in PBD and PBDS over this period. Although both were palliative studies, with similar inclusion and exclusion criteria, and similar endpoints, they differed in the type of stents inserted. In the first trial, plastic stents were used for both EBD and PBDS. However metallic stents were inserted percutaneously in the second trial and the results were compared with EBD using plastic stents. Both trials were stopped before reaching their full enrolment for ethical concerns but for different reasons. In the first RCT, the statistically higher 30 day mortality (33% vs 15%) and failure of drainage (61% vs 81%) in PBDS were the reasons. There was no significant difference in 30 day mortality between EBD and PBDS in the second trial, but significant differences existed in therapeutic success (71% vs 42%, p = 0.03) and median survival (3.7 months vs 2 months, p = 0.02), in favour of PBDS. As a result, each study drew a different conclusion. The first trial recommended that endoscopy should be tried first in the elderly and frail when stenting is being considered. The second trial concluded that metal stents inserted percutaneously are an alternative to endoscopic plastic stenting. Which one of these conclusions is more applicable in today's practice and why?
Since the first trial in 1987 (8), major technical advances have taken place in endoscopy and Interventional Radiology resulting in improved performance in biliary drainage, especially for percutaneous work. Examples of these advances were the use of ultrasound guidance (14) and improved equipment, including the introduction of self-expandable metallic stents (SEMS) (15). These advances have made PBD and stenting easier and safer to perform. Indeed, the high mortality in PBDS reported in the first trial has not been shown in any comparative series since 1987. Instead, significant differences in the therapeutic success and survival benefits with PBDS were reported in the second published randomized trial. (9) The superior performance of metallic stents compared to plastic stents has also been reported in EBD (16, 17). The longer duration of metallic stent patency has reduced the need for future re-interventions and enhances cost effectiveness (18). More importantly, plastic stents have long been replaced by metallic stents in percutaneous practice even though they are still used for EBD. Consequently, the results and conclusion of the first randomized trial are no longer relevant in today's clinical practice. By default, the second trial now becomes the only relevant source for level I evidence in biliary intervention and its recommendations remain valid today; percutaneous insertion of self-expanding metallic stents is an alternative to endoscopic stenting. The question that now remains is: how does endoscopic insertion of metallic stents compare with the percutaneous method? This question will remain unanswered until results of a randomized study become available, which is unlikely to appear soon.
Malignant obstruction at the hilar and peri-hilar regions is usually caused by Klatskin tumors or gallbladder carcinoma with local extension to involve the hilum. These obstructions present significant challenges for both endoscopic and percutaneous biliary drainage for a number of reasons. First and foremost, patients with Klatskin tumor or malignant hilar obstruction do not tolerate failure of drainage well, an observation recognized by both radiologists and endoscopists alike. Devierre (19) cautioned us of the serious negative impact on outcomes due to sepsis of undrained segments. Life-threatening septic complications may occur, and prolonged sepsis may delay or even disqualify patients from their intended treatment. Unlike distal biliary obstruction, remedial bypass surgery is seldom available and often risky. Second, biliary drainage is technically more difficult to perform, especially for EBD, and more than one stent or drainage catheter may be required due to the presence of multiple obstructed sites. Third, technical success may not translate into therapeutic success as consistently shown by all the RCT and retrospective studies in this review. Some general principles are available but they are not reliable predictors. Despite all of the above, some patients may benefit from well-designed treatment strategies skilfully executed by teams of dedicated health professionals, with long-term survival. Very often, the optimal strategy begins by choosing a drainage method that is highly successful and safe. In the East and Japan, the method of choice is PBD (6), but in Europe and North America, EBD is preferred. (13, 20). Here we review RCTs and non-randomized retrospective studies for evidence to address this controversy.
For hilar obstruction, the only randomized trial (10) showed that PBD out-performed EBD using plastic stents; a significantly higher therapeutic success (89% vs 41%, p ≤ 0.001) and a significantly lower complication rate (52% vs 18%, p = 0.04,) than EBD. This trial also assessed quality of life in the study groups and demonstrated a significant improvement in scores in the PBD group at 3 months post insertion.
The higher therapeutic success in PBD over EBD was also confirmed by 2 retrospective, non-randomized palliative studies (Lee (11) 97% vs 79%, p = 0.03; Paik (12): 92.7% vs 77.3%, p = 0.049) and corroborated by a retrospective preoperative study. (13) It should be noted that metallic stents were inserted in both EBD and PBD for palliation in the Paik study. Paik (12) also showed a significant increase in survival in those with initial successful drainage compared with those who failed the first attempt but succeeded subsequently (8.7 months vs 1.8 months, p <0.001).
In a retrospective non-randomized study in pre-operative drainage for Klatskin tumor, Kloek (13) reported that EBD took 15 weeks to achieve adequate therapeutic drainage while PBD took only 11 weeks (p = 0.033). In addition, 33% of patients in the EBD group were later converted to PBD due to inadequate or failed drainage. This report also found that PBD had fewer infectious complications and required fewer procedures. (13) Two other similar studies (20, 21) from tertiary referral centers in the United Kingdom also confirmed a high conversion rate from initial EBD to PBD from 80% (120 of 150 patients) to 88% (36 of 41 patients). None had reported a conversion in the opposite direction from failed PBD to EBD. The conclusions from these centres were uniformly negative towards EBD in pre-operative drainage in Klatskin tumors.
In summary, we consistently found supportive evidence that favours PBD as the preferred drainage procedure in malignant hilar obstruction: higher therapeutic success, shorter time to reach desired drainage, and negligible conversion rate. With the emergence of newer chemotherapeutic agents, effective drainage is key to early treatment. In this regard, the method that allows chemotherapy or surgery to start earlier is more preferable. When patients fail to respond to their EBD and require conversion to PBD, treatment is delayed and or may even disqualify them (due to prolonged sepsis or its sequaele) from receiving the appropriate care that they require and deserve. In this respect, the method that has the highest rate of conversion from EBD to PBD is the least clinically desirable.
It is generally believed that EBD is less invasive and has fewer complications than percutaneous drainage. Other than the earliest RCT in 1987 (8), this has not been validated statistically in any comparative studies included in this review. In fact, in malignant hilar obstruction, one RCT (10) and one retrospective non-randomized study (13) reported a significantly higher rate of cholangitis in the EBD group compared with the percutaneous group.
Cosmetic appeal is another reason for choosing EBD as the preferred drainage method as there is No need for catheter exposure as in PBD. Recent innovation in catheter fixation with the low profile device has improved the cosmetic appeal of PBD by making it less obtrusive. Once the device is applied, the external portion of the drainage catheter is shortened to 3 mm above the skin level and the device is taped to the skin with a small piece of adhesive over a small dressing. (Fig. 1) It also has an added benefit of allowing early detection of impending biliary re-obstruction (22). When biliary re-obstruction occurs or is about to occur, bile leakage around the insertion site would appear, alerting the patient to seek medical help and thus avoiding severe sepsis that may otherwise follow. In EBD, signs of early stent occlusion are non-specific and are often missed or ignored by patients. When overt signs appear, severe sepsis may have already set in; vigorous antibiotic treatment or even hospitalization may become necessary. Both physicians and their patients should be aware of the trade-off between EBD and PBD when choosing the method for biliary drainage.
In conclusion, the management of distal malignant biliary obstruction can be achieved most optimally through insertion of metallic stents either endoscopically or percutaneously. Evidence shows that metallic stents inserted percutaneously results in better outcomes than plastic stents inserted endoscopically. For malignant hilar obstruction, percutaneous drainage with catheter or metallic stents is preferred to endoscopic plastic stents or metallic stents.
Figures and Tables
Fig. 1
Low profile fixation device for transfixing internal / external biliary drainage catheter at skin surface.

Fig. 2
Patient with internal/external biliary drainage for palliation of obstructive jaundice. External portion of catheter has been transfixed by low profile device and cut short to 3 mm above skin level. Photo showing device covered by dressings and transparent adhesive tape (Reproduced with permission from AJR).

Table 1
Comparative Studies between EBD and Percutaneous Drainage in Malignant Biliary Obstruction: Study Type, Inclusion, Exclusion criteria, Obstruction Site

References
1. Andersen JR, Sørensen SM, Kruse A, Rokkjaer M, Matzen P. Randomised trial of endoscopic endoprosthesis versus operative bypass in malignant obstructive jaundice. Gut. 1989. 30:1132–1135.
2. Shepherd HA, Royle G, Ross AP, Diba A, Arthur M, Colin-Jones D. Endoscopic biliary endoprosthesis in the palliation of malignant obstruction of the distal common bile duct: a randomized trial. Br J Surg. 1988. 75:1166–1168.
3. Smith AC, Dowsett JF, Russell RC, Hatfield AR, Cotton PB. Randomised trial of endoscopic stenting versus surgical bypass in malignant low bileduct obstruction. Lancet. 1994. 344:1655–1660.
4. Dinant S, Gerhards MF, Rauws EA, Busch OR, Gouma DJ, van Gulik TM. Improved outcome of resection of hilar cholangiocarcinoma (Klatskin tumor). Ann Surg Oncol. 2006. 13:872–880.
5. Nakeeb A, Tran KQ, Black MJ, Erickson BA, Ritch PS, Quebbeman EJ, et al. Improved survival in resected biliary malignancies. Surgery. 2002. 132:555–563. discussion 563-564.
6. Seyama Y, Makuuchi M. Current surgical treatment for bile duct cancer. World J Gastroenterol. 2007. 13:1505–1515.
7. Valle J, Wasan H, Palmer DH, Cunningham D, Anthoney A, Maraveyas A, et al. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 2010. 362:1273–1281.
8. Speer AG, Cotton PB, Russell RC, Mason RR, Hatfield AR, Leung JW, et al. Randomised trial of endoscopic versus percutaneous stent insertion in malignant obstructive jaundice. Lancet. 1987. 2:57–62.
9. Piñol V, Castells A, Bordas JM, Real MI, Llach J, Montañà X, et al. Percutaneous self-expanding metal stents versus endoscopic polyethylene endoprostheses for treating malignant biliary obstruction: randomized clinical trial. Radiology. 2002. 225:27–34.
10. Saluja SS, Gulati M, Garg PK, Pal H, Pal S, Sahni P, et al. Endoscopic or percutaneous biliary drainage for gallbladder cancer: a randomized trial and quality of life assessment. Clin Gastroenterol Hepatol. 2008. 6:944–950.e3.
11. Lee SH, Park JK, Yoon WJ, Lee JK, Ryu JK, Yoon YB, et al. Optimal biliary drainage for inoperable Klatskin's tumor based on Bismuth type. World J Gastroenterol. 2007. 13:3948–3955.
12. Paik WH, Park YS, Hwang JH, Lee SH, Yoon CJ, Kang SG, et al. Palliative treatment with self-expandable metallic stents in patients with advanced type III or IV hilar cholangiocarcinoma: a percutaneous versus endoscopic approach. Gastrointest Endosc. 2009. 69:55–62.
13. Kloek JJ, van der Gaag NA, Aziz Y, Rauws EA, van Delden OM, Lameris JS, et al. Endoscopic and percutaneous preoperative biliary drainage in patients with suspected hilar cholangiocarcinoma. J Gastrointest Surg. 2010. 14:119–125.
14. Laméris JS, Obertop H, Jeekel J. Biliary drainage by ultrasound-guided puncture of the left hepatic duct. Clin Radiol. 1985. 36:269–274.
15. Lammer J, Hausegger KA, Flückiger F, Winkelbauer FW, Wildling R, Klein GE, et al. Common bile duct obstruction due to malignancy: treatment with plastic versus metal stents. Radiology. 1996. 201:167–172.
16. Davids PH, Groen AK, Rauws EA, Tytgat GN, Huibregtse K. Randomised trial of self-expanding metal stents versus polyethylene stents for distal malignant biliary obstruction. Lancet. 1992. 340:1488–1492.
17. Knyrim K, Wagner HJ, Pausch J, Vakil N. A prospective, randomized, controlled trial of metal stents for malignant obstruction of the common bile duct. Endoscopy. 1993. 25:207–212.
18. Raju RP, Jaganmohan SR, Ross WA, Davila ML, Javle M, Raju GS, et al. Optimum palliation of inoperable hilar cholangiocarcinoma: comparative assessment of the efficacy of plastic and self-expanding metal stents. Dig Dis Sci. 2011. 56:1557–1564.
19. Deviere J, Baize M, de Toeuf J, Cremer M. Long-term follow-up of patients with hilar malignant stricture treated by endoscopic internal biliary drainage. Gastrointest Endosc. 1988. 34:95–101.
20. Silva MA, Tekin K, Aytekin F, Bramhall SR, Buckels JA, Mirza DF. Surgery for hilar cholangiocarcinoma; a 10 year experience of a tertiary referral centre in the UK. Eur J Surg Oncol. 2005. 31:533–539.
21. Mansfield SD, Barakat O, Charnley RM, Jaques BC, O'Suilleabhain CB, Atherton PJ, et al. Management of hilar cholangiocarcinoma in the North of England: pathology, treatment, and outcome. World J Gastroenterol. 2005. 11:7625–7630.
22. Ho CS, Hatrick AG. Innovative catheter fixation using a low-profile device. AJR Am J Roentgenol. 2000. 174:823–825.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download