1. Nordback IH, Pitt HA, Coleman J, Venbrux AC, Dooley WC, Yeu NN, et al. Unresectable hilar cholangiocarcinoma: percutaneous versus operative palliation. Surgery. 1994; 115:597–603. PMID:
7513906.
2. LaBerge JM, Doherty M, Gordon RL, Ring EJ. Hilar malignancy: treatment with an expandable metallic transhepatic biliary stent. Radiology. 1990; 177:793–797. PMID:
2173842.

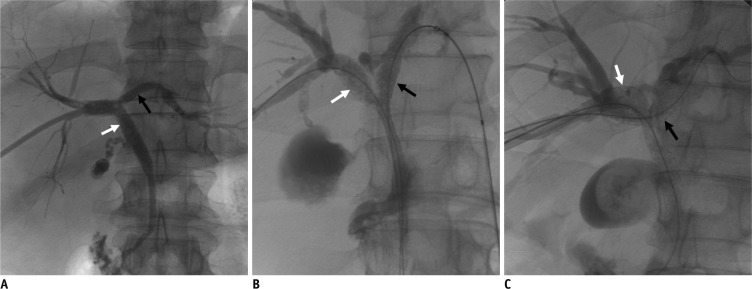
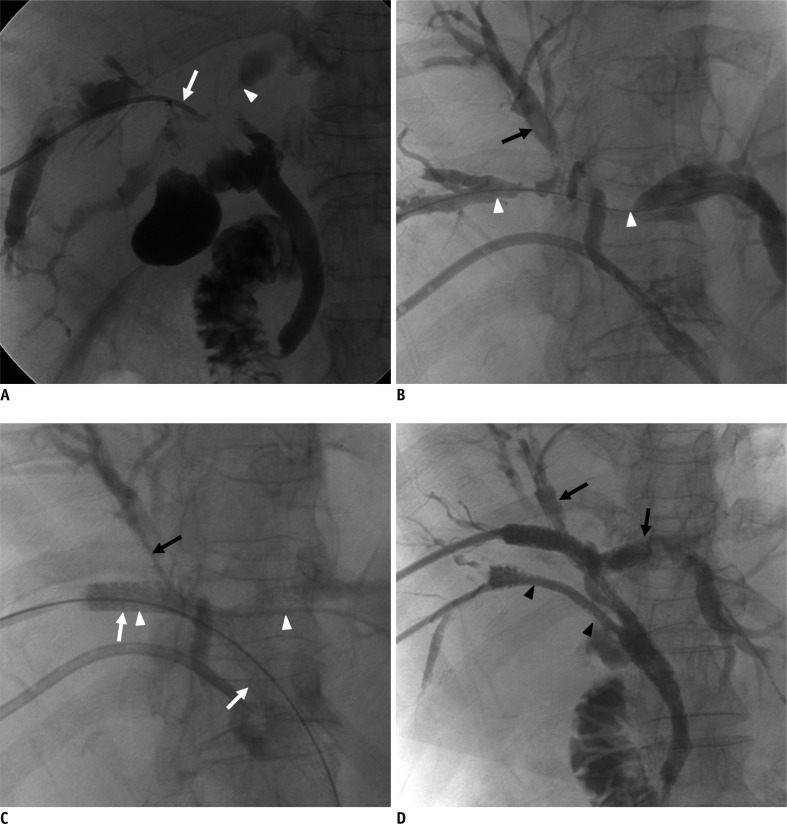
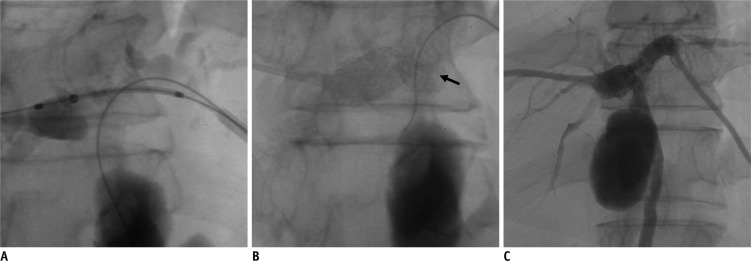
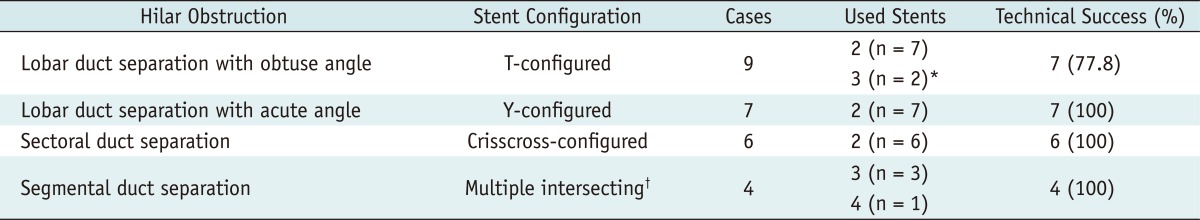
3. Kim CW, Park AW, Won JW, Kim S, Lee JW, Lee SH. T-configured dual stent placement in malignant biliary hilar duct obstructions with a newly designed stent. J Vasc Interv Radiol. 2004; 15:713–717. PMID:
15231885.

4. Inal M, Akgül E, Aksungur E, Seydaoğlu G. Percutaneous placement of biliary metallic stents in patients with malignant hilar obstruction: unilobar versus bilobar drainage. J Vasc Interv Radiol. 2003; 14:1409–1416. PMID:
14605106.

5. De Palma GD, Galloro G, Siciliano S, Iovino P, Catanzano C. Unilateral versus bilateral endoscopic hepatic duct drainage in patients with malignant hilar biliary obstruction: results of a prospective, randomized, and controlled study. Gastrointest Endosc. 2001; 53:547–553. PMID:
11323577.

6. Cowling MG, Adam AN. Internal stenting in malignant biliary obstruction. World J Surg. 2001; 25:355–359. discussion 359-361. PMID:
11343193.
7. Rerknimitr R, Kladcharoen N, Mahachai V, Kullavanijaya P. Result of endoscopic biliary drainage in hilar cholangiocarcinoma. J Clin Gastroenterol. 2004; 38:518–523. PMID:
15220688.

8. Choi KH, Cho YK, An JK, Woo JJ, Kim HS, Choi YS. Acute obstructive cholangitis after transarterial chemoembolization: the effect of percutaneous transhepatic removal of tumor fragment. Korean J Radiol. 2009; 10:197–201. PMID:
19270868.

9. Han YM, Kwak HS, Jin GY, Lee SO, Chung GH. Treatment of malignant biliary obstruction with a PTFE-covered self-expandable nitinol stent. Korean J Radiol. 2007; 8:410–417. PMID:
17923784.

10. Kim JH. Clinical feasibility and usefulness of CT fluoroscopy-guided percutaneous transhepatic biliary drainage in emergency patients with acute obstructive cholangitis. Korean J Radiol. 2009; 10:144–149. PMID:
19270860.

11. Lee JH, Kang DH, Kim JY, Lee SM, Kim do H, Park CW, et al. Endoscopic bilateral metal stent placement for advanced hilar cholangiocarcinoma: a pilot study of a newly designed Y stent. Gastrointest Endosc. 2007; 66:364–369. PMID:
17643714.

12. Topazian M. Toward a better biliary confluence stent. Gastrointest Endosc. 2007; 66:369–371. PMID:
17643715.

13. Duda SH, Wiskirchen J, Tepe G, Bitzer M, Kaulich TW, Stoeckel D, et al. Physical properties of endovascular stents: an experimental comparison. J Vasc Interv Radiol. 2000; 11:645–654. PMID:
10834499.

14. Sobolevsky SA, Rakin D, Janne d'Othee B, Lang EV. Complex stent assemblies: feasibility of stent-through-stent deployment. Cardiovasular and Interventional Society of Europe e-poster: P100 September 2006.
15. Rutledge JM, Grifka RG, Bryant LL, Mullins CE, Vincent JA. Balloon dilation and stent implant through the side of a previously placed intravascular stent: a new option for the interventionalist. Catheter Cardiovasc Interv. 2002; 56:387–393. PMID:
12112895.

16. Pierce DS, Rosero EB, Modrall JG, Adams-Huet B, Valentine RJ, Clagett GP, et al. Open-cell versus closed-cell stent design differences in blood flow velocities after carotid stenting. J Vasc Surg. 2009; 49:602–606. discussion 606. PMID:
19268763.

17. Sacks D, McClenny TE, Cardella JF, Lewis CA. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol. 2003; 14(9 Pt 2):S199–S202. PMID:
14514818.

18. Bae JI, Park AW, Choi SJ, Kim HP, Lee SJ, Park YM, et al. Crisscross-configured dual stent placement for trisectoral drainage in patients with advanced biliary hilar malignancies. J Vasc Interv Radiol. 2008; 19:1614–1619. PMID:
18823794.

19. Dumas R, Demuth N, Buckley M, Peten EP, Manos T, Demarquay JF, et al. Endoscopic bilateral metal stent placement for malignant hilar stenoses: identification of optimal technique. Gastrointest Endosc. 2000; 51:334–338. PMID:
10699784.

20. Kim JY, Kang DH, Kim HW, Choi CW, Kim ID, Hwang JH, et al. Usefulness of slimmer and open-cell-design stents for endoscopic bilateral stenting and endoscopic revision in patients with hilar cholangiocarcinoma (with video). Gastrointest Endosc. 2009; 70:1109–1115. PMID:
19647244.

21. Müller-Hülsbeck S, Schäfer PJ, Charalambous N, Schaffner SR, Heller M, Jahnke T. Comparison of carotid stents: an in-vitro experiment focusing on stent design. J Endovasc Ther. 2009; 16:168–177. PMID:
19456191.

22. Park do H, Lee SS, Moon JH, Choi HJ, Cha SW, Kim JH, et al. Newly designed stent for endoscopic bilateral stent-in-stent placement of metallic stents in patients with malignant hilar biliary strictures: multicenter prospective feasibility study (with videos). Gastrointest Endosc. 2009; 69:1357–1360. PMID:
19481654.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download