Abstract
Objective
Materials and Methods
Results
Figures and Tables
 | Fig. 1
Diagram showing definition of technical success. If viable tumor (T) around retained iodized oil (asterisk) was completely ablated on immediate follow-up CT scan, it was defined as primary technical success (A). When both viable tumor (T) and retained iodized oil (asterisk) were completely ablated, it was defined as secondary technical success (B). |
 | Fig. 2
Flow chart of inclusion and exclusion criteria. "Visible on fluoroscopy" was defined when index tumor was radio-opaque enough to be visible on both anteroposterior and lateral projections, and thus could be targeted under biplane fluoroscopy with US guidance. *Among 40 referred patients, 37 had single viable HCC around retained iodized oil, while other 3 had 2 or 3 HCCs (including at least one viable HCC around the retained iodized oil), resulting in total of 42 viable HCCs around retained iodized oil and 3 new HCCs. †Two patients who had viable HCC around retained iodized oil surrounded by inferior vena cava and right hepatic vein (n = 1) or inadequate electrode path (n = 1) were excluded for percutaneous radiofrequency ablation. ‡In two patients with multinodular HCCs, although two viable HCCs around retained iodized oil were visible on fluoroscopy, other new HCCs were invisible on US. In remaining one patient, viable HCC around retained iodized oil was invisible on fluoroscopy. Therefore, total of 27 viable HCCs were visible on fluoroscopy, whereas remaining 15 viable HCCs were invisible. HCC = hepatocellular carcinoma, TACE = transcatheter arterial chemoembolization |
 | Fig. 357-year-old man with viable hepatocellular carcinoma (HCC) in left hepatic dome after repeated transcatheter arterial chemoembolization (TACE).
A. Arterial phase axial CT scan obtained one month after four TACE sessions shows enhancing lesion with maximum diameter of 2.2 cm (arrowheads), located around incomplete accumulation of iodized oil (black asterisk) in hepatic segment III. Patient had previous history of radiofrequency ablation (RFA) for another HCC (white asterisk) in segment VIII of liver. B. Delayed phase CT scan shows wash-out (arrowheads) suggestive of viable HCC, in site corresponding to enhancing lesion in A. C. Fluoroscopic images demonstrate accumulation of iodized oil (arrowheads) around viable HCC on magnified anteroposterior (C) and lateral (D) projection images, which were not visualized by US. Biplane fluoroscopy using retained iodized oil as radio-opaque anatomic landmark was chosen as main guiding modality for percutaneous RFA. D. Fluoroscopic images demonstrate accumulation of iodized oil (arrowheads) around viable HCC on magnified anteroposterior (C) and lateral (D) projection images, which were not visualized by US. Biplane fluoroscopy using retained iodized oil as radio-opaque anatomic landmark was chosen as main guiding modality for percutaneous RFA. E. Representative anteroposterior (AP) and lateral (Lat) fluoroscopic images obtained during six overlapping radiofrequency ablation (RFA) procedures. We inserted electrode to lateral aspect of retained iodized oil, where viable HCC was considered to be present (left column). Multiple overlapping ablations were facilitated using steep oblique approach based on biplane fluoroscopic images in which retained iodized oil remained almost unchanged over 6 overlapping ablations. On sixth overlapping (right column), electrode was positioned in anterior side of retained iodized oil. Although not shown here, US was used for monitoring purposes during each ablation cycle. Total ablation time of six overlapping treatments was 26 minutes. F. Transverse portal phase CT image obtained immediately after single RFA session reveals partial intratumoral deposition of iodized oil, with sufficient non-enhancing ablative zone (arrowheads), with maximum diameter of 4.5 cm.
|
Table 2
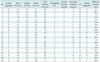
Table 3
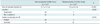
Note.- *When retained iodized oil in tumors was visible on both anteroposterior and lateral projection images, and thus was suitable for targeting tumor under guidance of biplane fluoroscopy, they were classified in fluoroscopically visible group. If index tumors were invisible or poorly visible on anteroposterior, lateral or both images, and thus not feasible for targeting tumor, they were regarded as part of fluoroscopically invisible group, †Subphrenic location of tumor was defined when index tumor was either located within 1 cm from diaphragm or abutting diaphragm, ‡Visible group on US was defined when index tumor was conspicuous enough to allow percutaneous US-guided RFA, whereas invisible group was defined when index tumor was inconspicuous, thus unsuitable for percutaneous US-guided RFA. US = ultrasonography, RFA = radiofrequency ablation




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download