Abstract
Objective
To assess the feasibility of visualizing hand and foot tendon anatomy and disorders by Gemstone Spectral Imaging (GSI) high-definition CT (HDCT).
Materials and Methods
Thirty-five patients who suffered from hand or foot pain were scanned with GSI mode HDCT and MRI. Spectrum analysis was used to select the monochromatic images that provide the optimal contrast-to-noise ratio (CNR) for tendons. The image quality at the best selected monochromatic level and the conventional polychromatic images were compared. Tendon anatomy and disease were also analyzed at GSI and MRI.
Results
The monochromatic images at about 65 keV (mean 65.09 ± 2.98) provided the optimal CNR for hand and foot tendons. The image quality at the optimal selected monochromatic level was superior to conventional polychromatic images (p = 0.005, p < 0.05). GSI was useful in visualizing hand and foot tendon anatomy and disorders. There were no statistical differences between GSI and MRI with regard to tendon thickening (χ2 = 0, p > 0.05), compression (χ2 = 0.5, p > 0.05), absence (χ2 = 0, p > 0.05) and rupture (χ2 = 0, p > 0.05). GSI was significantly less sensitive than MRI in displaying tendon adhesion (χ2 = 4.17, p < 0.05), degeneration (χ2 = 4.17, p < 0.05), and tendinous sheath disease (χ2 = 10.08, p < 0.05).
Conclusion
GSI with monochromatic images at 65 keV displays clearly the most hand and foot tendon anatomy and disorders with image quality improved, as compared with conventional polychromatic images. It may be used solely or combined with MRI in clinical work, depending on individual patient disease condition.
Tendon and ligament imaging is problematic for routine computed tomography (CT), with low specificity and sensitivity, limiting applications in this area (1). Magnetic resonance imaging (MRI) has fine soft-tissue contrast resolution and multi-planar capability, making it a useful tool in diagnosis (2), but the long duration and high cost of MRI and occasional contraindications limit usefulness in this application. Recently the emergence of gemstone spectral imaging (GSI) technique may allow broader application in musculoskeletal diseases by dint of its high resolution and spectral imaging, especially for tendons and ligaments (3, 4). The aim of this study was to investigate the primary value of GSI in hand and foot tendon anatomy and disease diagnosis.
From October 2010 to May 2011, thirty-five patients (22 men and 13 women) who suffered from hand or foot disease were scanned with GSI mode by high-definition CT (HDCT) and MRI. Patients experienced one or more of the following symptoms: extension and flexion dysfunction, pain and deformation after hand or foot surgery, hand or foot external injury, hand or foot pain, and activity limitation. The age range was 18-64 years with a mean age of 35.8 years. All patients provided informed written consent and all the cases were confirmed by operation or follow-up. The tendon disorders included adhesion (n = 16), thickening (n = 14), compression (n = 12), absence (n = 10), rupture (n = 11), degenerative type (n = 6), and tendinous sheath diseases (n = 25). Twenty-one patients were treated surgically, and the remainder's diagnoses were confirmed by the combination with patient history, clinical signs and other information with the consensus of surgeons and radiologists. Each type of tendon disorder follows: 1) The tendon margin was rough, and the boundary with surrounding soft tissues was unclear, in adhesion type. 2) The tendon diameter was increased, and the boundary was clear, in thickening type. 3) The tendon itself was normal, but compressed or shifted from primary location because of external lesions, in compression type. 4) With part or the whole tendon loss, normal tendon tissues were not found in original area, in absence type. 5) The tendon's continuity was broken, and the broken ends of ruptured tendons were always contracted, in rupture type. 6) Tendon degeneration demonstrated the pathological changes of chronic injury. 7) Tendinous sheath diseases included inflammation and cyst lesions.
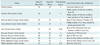
We used spectral HDCT (GE Discovery CT750 HD; GE Healthcare, Milwaukee, WI, USA) in GSI mode and 1.5T MRI (GE signal 1.5T HD; GE Healthcare, Milwaukee, WI, USA). When imaging a hand, the patient was placed in a prone position with arms above the head and the forearm in maximun pronation. When imaging a foot, the patient was placed in neutral supine position. The patients were scanned bilaterally with GSI for contrast. The detailed scan parameters are listed in (Tables 1, 2).
The monochromatic images with the slice thickness of 0.625 mm and spacing of 0.625 mm were sent to a special GSI viewer for analysis. The keV of optimal contrast-to-noise ratio (Optimal CNR) for viewing tendons compared to surrounding muscle and other soft tissues was selected using energy spectrum analysis software (Fig. 1). Each patients were measured for three times.
Images with the optimal selected monochramatic level were transferred to an AW 4.4 workstation (GSI viewer 2.00 and GE VolumeShare 4 AW 4.4, GE Healthcare). Two radiographers performed the post-processing. Image-processing techniques including volume rendering (VR), multiple planner reconstruction (MPR), and curved planner reconstruction (CRP) were used to observe the tendons' anatomy in non-diseased hand and foot. The emphasis of the observation was tendon's shape, density and stop point.
Normal tendons were evaluated as follows (5): 1) The tendon's stop points displayed: clearly, 2 points; fuzzily, 1 point; could not be displayed, 0 point. 2) The tendon's shape displayed: clearly, 2 points; fuzzily, 1 point; could not be displayed, 0 point.
The image quality at the optimal selected monochromatic level and the conventional polychromatic images were compared. Comparison included the following four parts with four scores in all: the shape of tendons, the attachment points of tendons, image noise and the contrast of tendon and surrounding tissues.
Selected optimal monochromatic images were transferred to an AW 4.4 workstation where image-processing techniques including VR, MPR and CPR, were applied. Two radiologists observed and diagnosed the GSI and MRI images. Comparison of the two imaging modalities were analyzed.
SAS 9.0 software was used for statistical analysis. A standard non-parametric test of two independent samples (Mann-Whitney U test) was used to analyze the imaging quality at different imaging modalities. Tendon disorders in GSI and magnetic resonance (MR) image were compared using χ2 test adjusted for paired fourfold table and p < 0.05 was considered statistically significant.
The monochromatic images at about 65 keV (mean 65.09 ± 2.98) were found to provide the best CNR for hand and foot tendons across three replications (Fig. 1).
Most hand and foot tendons were displayed clearly with GSI (Tables 3, 4). Normal tendons were always shown as smooth, continuous, with steady density and clear edge (Fig. 2). However, some problems remained. The stop points of tibialis posterior tendon, flexor carpi radialis muscle tendon and long fibular muscle tendon were not shown clearly since the deep position was covered with many muscles. The distal end of digit extensor tendon and musculus flexor digitorum sublimis tendon were too tenuous to find with GSI. We could also detect some tendon variations. For example, tibialis posterior tendons in six patients were found extending through para-ankle central bone and two of them felt complaint.
The scores of the monochramatic images at 65 keV and the conventional polychromatic images were 3.33 ± 0.48 and 2.87 ± 0.73. This difference is statistically significant statistical (p = 0.005, p < 0.05), meaning that the image quality at 65 keV was superior to the conventional polychromatic images (Table 5) (Fig. 3).
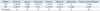
Gemstone spectral imaging and MRI both displayed most tendondisorders. The comparison of GSI and MRI in displaying basic tendon disorders is provided in Table 6. There were no statistical differences between GSI and MR imaging with regard to tendon thickening (χ2 = 0, p > 0.05), compression (χ2 = 0.5, p > 0.05), absence (χ2 = 0, p > 0.05) and rupture (χ2 = 0, p > 0.05). GSI was significantly less sensitive than MRI in displaying tendon adhesion (χ2 = 4.17, p < 0.05), degeneration (χ2 = 4.17, p < 0.05), and tendinous sheath disease (χ2 = 10.08, p < 0.05). Using three-dimensional volume rendering, GSI displayed the tendons' whole shape and relationship with other tissues more directly than MRI. (Figs. 4-8)
Hand and foot tendon injuries are very common in routine work. Diagnosis is usually based on trauma history and clinical examination in the absence of direct imaging modality. MRI, because of good tissue contrast resolution, remains the gold standard for musculoskeletal imaging (6). However, there is a wide range of situations when MRI cannot be performed, such as patients with pacemakers or claustrophobia, or in emergency situations. Though CT techniques was earlier used to diagnose tendon injuries and proved to be a useful tool, tendon imaging is still weak with conventional CT for lack of density contrast (7, 8). Recently, a new technique with higher soft tissue resolution, GSI, may improve the application of tendon imaging for multi-detector computed tomography (MDCT).
Now GSI images can be obtained from HDCT (GE Discovery CT750 HD; GE Healthcare, Milwaukee, WI, USA). This spectral CT has undergone many technical innovations, such as momentary switching between high and low energy (140 kV and 80 kV) in a single X-ray tube, a high-performance gemstone detector, and powerful image post-processing. This makes material differentiation with monochromatic energy feasible (9, 10). The monochromatic imaging can help to eliminate the ray-hardening artifacts, optimizes imaging quality, and increases image contrast (11). With GSI imaging, we can get 101 monochromatic images from 40 keV to 140 keV. The use of optimal monochromatic energy allows selection of the best CNR image for tendon and surrounding tissues. In this study, the monochromatic images at about 65 keV provided the best CNR for hand and foot tendons, with quality superior to conventional polychromatic images. Most hand and foot tendons could be shown clearly, including the tendon shape and stop points. These improvements result in a great increase in the ability of GSI to display minor lesions.
The chief advantage of GSI over MRI and sonography is the ability to provide a three-dimensional (3D) display of tendons (12). Although MRI can make 3D acquisition now, it requires long scanning times and the resolution is poor. Many patients cannot tolerate staying in one position for long durations, especially for surgical trauma (13). MDCT in combination with 3D image reconstruction has shown to be useful for the evaluation of a variety of tendon abnormalities (5, 7). MDCT may serve as a valuable alternative imaging tool for the assessment of soft tissues when ultrasound or MRI cannot be used; for example, in the presence of large open wounds or when there is post surgical metallic hardware close to the anatomical area of interest (14). Ohashi et al. (15) showed that VR technique with MDCT could display various kinds of tendon injuries for fracture more directly. We also found that GSI images with 3D model could detect tendon diseases such as tendon thickening, absence, compression and rupture more directly than MRI. These direct reconstruction images help define the best surgical procedure and post-operative therapy for specific injury.
However, GSI also has limitations in visualizing hand and foot tendons, such as the inner lesions of tendons and paratendons. In this study, there were six tendon degeneration and twelve tendinous sheath disorders missed in GSI because no change of density could be found, although detected readily with MRI. This problem might be resolved by using spectral analysis. The change of spectral analysis curve might suggest presence of tendon injuries before density changes appear. The cases in this study were too few to examine this. We hope to examine this in further studies. Furthermore, not all tendons could be shown clearly with GSI, especially in the distal end of digit extensor tendon and musculus flexor digitorum sublimis tendon, limiting application in this area. Another shortfall of GSI is the radiation dose. The average radiation dose in GSI mode may be increased for switching between high and low energy. In this study, the average CTDIvol was 18.25 mGy, much higher than routine CT (5, 16), so it is prohibited for pregnant women and children.
In our study, the number of patient cases was so small that we could evaluate only the primary effectiveness of GSI and MRI. Further studies should properly classify the injury lesions detection of GSI.
In summary, we consider that GSI with monochromatic images at 65 keV improves the image quality. GSI can show tendons' whole shape, stop points and many conditions, such as tendon thickening, compression, absence and rupture more directly than MRI. So it is well-suited to patients with acute external injuries, extremity malformation, mental disorders and other patients who are contraindicated for MRI examination. But GSI has less sensitivity in displaying tendon adherence, degeneration and tendinous sheath diseases than MRI. Therefore, the examination method should be chosen in line with condition type and individual situation.
Figures and Tables
 | Fig. 1Optimal CNR for hand and foot tendons.
A. Normal tendon and surrounding muscles as regions of interest. B. According to spectral curve, monochromatic images at about 65 keV were found to provide best CNR. CNR = contrast-to-noise ratio
|
 | Fig. 2Normal tendons (volume rendering images).
A. Normal hand tendons, 1. Musculus flexor digitorum sublimis/profundus tendon, 2. Flexor pollicis longus muscle tendon, 3. Flexor carpi radialis muscle tendon, 4. Musculus flexor carpi ulnaris tendon. B. Normal foot tendons, 1. Extensor pollicis longus muscle tendon, 2. Long extensor muscle digits tendon, 3. Long fibular muscle tendon, 4. Musculus fibularis brevis tendon, 5. Musculus fibularis tertius tendon.
|
 | Fig. 3Comparison with different imaging modalities.
A. Monochramatic images at 65 keV. B. Conventional polychromatic images. Though image noise in former image was larger, edge of tendons was displayed more sharply and image contrast was better (window width/level: 185/55).
|
 | Fig. 4Tendon adherence after trauma in left hand.
A. Gemstone spectral imaging volume rendering images can clearly display whole relationship of adhesive flexor tendon and phalanges (arrow). B. MRI coronal T1WI cannot present whole relationship of tendons and phalanges in two-dimensional image (arrow). T1WI = T1 weighted image
|
 | Fig. 5
Stretching function of thumb is constrained after left external wrist and hand injuries. Absence of extensor pollicis longus tendon, extensor pollicis brevis tendon, extensor carpi radialis longus and brevis were displayed in left hand with gemstone spectral imaging volume rendering image. We could not find any tendon tissues in original area and radialis soft tissues were thickening (arrow). Opposite hand tendons were normal: 1. Extensor pollicis longus tendon, 2. Extensor pollicis brevis tendon, 3. Extensor carpi radialis longus and brevis. |
 | Fig. 6
Achilles tendon rupture after trauma. Gemstone spectral imaging volume rendering image showed that superior part of achilles tendon's continuity was broken (arrow). Broken ends of ruptured tendons were contractural and circumambient soft tissues wereswollen. |
 | Fig. 7
Compression of tendon. Oblique sagittal MPR of gemstone spectral imaging found mass located in proximal phalanx bottom of little finger. Vicinal flexor tendon was compressed with shape change, but tendon itself was normal (arrow). Enchondroma with tendon compression were comfirmed by operation. MPR = multiplanar reconstryction |
 | Fig. 8Fiftysix year old male patient experienced slight claudication for fifteen years but no pain after surgery for fracture of left lower leg.
A. Achilles tendon was not found abnormal in gemstone spectral imaging images. B. In MRI FS PDWI images, high signal in strip can be seen (arrow). Combined with disease history and clinical signs, degenerative changes of achilles tendon were considered.
|
Acknowledgements
The authors thank Dr. Zeng-tao Wang (hand-and-foot surgeon) for help with patients' provision.
References
1. Jacobson JA. Musculoskeletal ultrasound and MRI: which do I choose? Semin Musculoskelet Radiol. 2005. 9:135–149.
2. Clavero JA, Alomar X, Monill JM, Esplugas M, Golanó P, Mendoza M, et al. MR imaging of ligament and tendon injuries of the fingers. Radiographics. 2002. 22:237–256.
3. Zhang D, Li X, Liu B. Objective characterization of GE discovery CT750 HD scanner: gemstone spectral imaging mode. Med Phys. 2011. 38:1178–1188.
4. Yang WJ, Chen KM, Pang LF, Guo Y, Li JY, Zhang H, et al. High-definition computed tomography for coronary artery stent imaging: a phantom study. Korean J Radiol. 2012. 13:20–26.
5. Deng K, Sun C, Liu C, Ma R. Initial experience with visualizing hand and foot tendons by dual-energy computed tomography. Clin Imaging. 2009. 33:384–389.
6. Bencardino JT. MR imaging of tendon lesions of the hand and wrist. Magn Reson Imaging Clin N Am. 2004. 12:333–347. vii
7. Sunagawa T, Ochi M, Ishida O, Ono C, Ikuta Y. Three-dimensional CT imaging of flexor tendon ruptures in the hand and wrist. J Comput Assist Tomogr. 2003. 27:169–174.
8. Santiago FR, Plazas PG, Fernández JM. Sonography findings in tears of the extensor pollicis longus tendon and correlation with CT, MRI and surgical findings. Eur J Radiol. 2008. 66:112–116.
9. Lin XZ, Miao F, Li JY, Dong HP, Shen Y, Chen KM. High-definition CT Gemstone spectral imaging of the brain: initial results of selecting optimal monochromatic image for beam-hardening artifacts and image noise reduction. J Comput Assist Tomogr. 2011. 35:294–297.
10. Goo HW, Yang DH, Kim N, Park SI, Kim DK, Kim EA. Collateral ventilation to congenital hyperlucent lung lesions assessed on xenon-enhanced dynamic dual-energy CT: an initial experience. Korean J Radiol. 2011. 12:25–33.
11. Hur S, Lee JM, Kim SJ, Park JH, Han JK, Choi BI. 80-kVp CT using Iterative Reconstruction in Image Space algorithm for the detection of hypervascular hepatocellular carcinoma: phantom and initial clinical experience. Korean J Radiol. 2012. 13:152–164.
12. Soni P, Stern CA, Foreman KB, Rockwell WB. Advances in extensor tendon diagnosis and therapy. Plast Reconstr Surg. 2009. 123:52e–57e.
13. Sun C, Miao F, Wang XM, Wang T, Ma R, Wang DP, et al. An initial qualitative study of dual-energy CT in the knee ligaments. Surg Radiol Anat. 2008. 30:443–447.
14. Sunagawa T, Ishida O, Ishiburo M, Suzuki O, Yasunaga Y, Ochi M. Three-dimensional computed tomography imaging: its applicability in the evaluation of extensor tendons in the hand and wrist. J Comput Assist Tomogr. 2005. 29:94–98.
15. Ohashi K, Restrepo JM, El-Khoury GY, Berbaum KS. Peroneal tendon subluxation and dislocation: detection on volume-rendered images--initial experience. Radiology. 2007. 242:252–257.
16. Dalrymple NC, Prasad SR, Freckleton MW, Chintapalli KN. Informatics in radiology (infoRAD): introduction to the language of three-dimensional imaging with multidetector CT. Radiographics. 2005. 25:1409–1428.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download