Abstract
Objective
To evaluate the effectiveness of uterine artery embolization (UAE) for treating symptomatic fibroids with high signal intensity (SI) on magnetic resonance (MR) T2-weighted imaging (T2WI).
Materials and Methods
A total of 537 cases, consisting of 14 patients with high SI fibroids on T2WI (T2 high group), were retrospectively included and compared with 28 randomly selected patients with low SI fibroids on T2WI (control group). High SI of a predominant fibroid on T2WI was defined as having the same or higher SI than the myometrium. Patient ages ranged from 28 to 52 years (mean, 38.1 years). All patients underwent MRI before and after UAE. Predominant fibroid and uterine volumes were calculated with MR images. Symptom status in terms of menorrhagia and dysmenorrhea was scored on a scale of 0-10, with 0 being no symptoms and 10 being the baseline, or initial symptoms.
Results
Of the patients in the T2 high group, 13 out of 14 (92.9%) patients demonstrated complete necrosis of the predominant fibroids. The mean volume reduction rates of the predominant fibroids in the T2 high group was 61.7% at three months after UAE, which was significantly higher than the volume reduction rates of 42.1% noted in the control group (p < 0.05). Changes in symptom scores for menorrhagia and dysmenorrhea after UAE (baseline score minus follow-up score) were 4.9 and 7.5 in T2 high group and they were 5.0 and 7.7 in control group, suggesting a significant resolution of symptoms (p < 0.01) in both groups but no significant difference between the two groups.
Uterine artery embolization (UAE) has recently been applied to the management of symptomatic leiomyomas and is rapidly gaining acceptance as an effective alternative to a hysterectomy and myomectomy (1, 2). Despite extensive clinical experience in UAE, patient selection is a complex process influenced by presenting symptoms, physical examination, imaging findings, and patient preferences. Therefore, it is important to verify the presence of uterine leiomyomas to confirm whether the leiomyomas are causing the main symptoms, and to determine specific anatomic criteria, such as leiomyoma size, location, morphology, degeneration and vascularity, which may affect patient outcomes (3).
Signal intensity (SI) of leiomyomas on T2-weighted imaging (T2WI) is a major factor in predicting responsive or unresponsive tumors depending on the treatment modality (4-6). However, the study of UAE effectiveness with respect to leiomyomas with high SI on T2WI is scant, where a high SI fibroid on T2WI can be defined as having the same or higher SI than that of the myometrium or skeletal muscle (7). A high SI of the fibroid on T2WI may represent high cellularity, proliferative activity as well as increased vascularity, and those fibroids may demonstrate a better response to UAE (8-10).
The purpose of the current study was to evaluate the effectiveness of UAE for treating symptomatic high SI fibroids on T2WI.
The institutional review board gave approval for the entire study, and each patient gave written informed consent. All patients who underwent UAE for symptomatic fibroids between August 2007 and July 2010 were analyzed. Among the 537 cases, a total of 14 patients with high SI fibroids on T2WI (T2 high group) were retrospectively enrolled in the study. A computerized random number generator was used to select two times as many patients from the control group than the T2 high group. A total of 28 patients with low SI fibroids on T2WI (control group) were randomly selected for comparison. A high SI predominant fibroid on T2WI was defined as having the same or higher SI than that of the myometrium, a low SI; lower SI than that of the normal myometrium. Patients who demonstrated high SI on T2WI without contrast enhancement, which is considered indicative of a degenerative fibroid and is contraindicated for UAE, were excluded from the study. Patient ages ranged from 28 to 52 years (mean 38.1 years). The median follow-up period was 7.5 months (range; 3-30 months).
All magnetic resonance (MR) images were analyzed by two experienced radiologists, by consensus. All patients underwent a preprocedural MRI (1.5-T Signa HD/HDx; GE Healthcare, Waukesha, WI, USA) of the pelvis. Axial and sagittal fast spin echo T2WI (TR/effective TE, 4400/120; matrix size, 384 × 224; field of view, 300 × 300 mm; section thickness, 5 mm) and contrast-enhanced sagittal T1-weighted imaging were performed in all cases. Enhanced MRI (TR/TE, 766/9; flip angle 90°; matrix size, 256 × 160; field of view, 300 × 300 mm; section thickness, 5 mm) was performed 2 minutes after intravenous infusion of 10 mL gadolinium (Dotarem, Guerbet, Auckland, New Zealand). Necrosis was defined as the absence of contrast enhancement on T1-weighted imaging. The total volume of the predominant fibroids and uterus was determined by measuring the length, height, and width and calculating the volume with use of the equation for a prolate ellipse: length × width × height × 0.5233 (11).
Follow-up consisted of an outpatient visit, where a questionnaire interview was conducted followed by an MRI; 3 months after UAE in all patients. Patients were assessed for the extent of fibroid volume reduction as well as fibroid necrosis after UAE by a 3-month follow-up MRI.
Unilateral right femoral artery access was used in all cases. A 5.0 Fr RHR catheter (Cook, Bloomington, IN, USA) was placed in the internal iliac artery, and a coaxial 3 Fr microcatheter (MicroFerret; Cook, Bloomington, IN, USA) was advanced distally into the uterine artery. Embolization was performed with the catheter tip beyond the origin of the cervicovaginal branch. The primary embolic agent was non-spherical polyvinyl alcohol (PVA) particles (Contour; Boston Scientific, Natick, MA, USA) mixed with 60 mL of 1 : 1 saline solution : contrast agent mixture. The choice of PVA size was based on operator preference; 250 to 355 µm or 355 to 500 µm of PVA particles were used initially, followed by 355 to 500 µm or 500 to 710 µm particles. Embolization was performed until complete cessation of blood flow was achieved in the ascending uterine artery during ten cardiac beats. Intravenous administration of 30 mg of ketorolac tromethamine was performed at the moment the first uterine artery was catheterized. Pain after UAE was managed via an intravenous patient-controlled analgesic pump containing 500 µg of fentanyl sulfate and 90 mg of ketorolac tromethamine mixed with 50 mL of normal saline.
A symptom severity questionnaire was administered in order to assess the severity of menstrual bleeding and dysmenorrhea during and between menstrual periods on a scale from 0 (no impact) to 10 (severe impact) at the time of the three-month follow-up MR imaging study.
A t test and Fisher's exact test were used to compare the effects of UAE on volumes of predominant fibroids and clinical outcomes between the two groups. A paired t test was used to determine the effects of UAE in each group. Differences were considered to be statistically significant at p < 0.05.
Data analyses were performed with the SPSS statistical software (SPSS, version 12; SPSS, Chicago, IL, USA).
The baseline characteristics of the leiomyomas are summarized in Table 1.
Among the 537 patients who underwent UAE, 14 (2.6%) had fibroids with high SI on T2WI; there were no technical failures resulting from an inability to catheterize the uterine artery. Moreover, there were no statistically significant differences with respect to age or mean diameters and volumes of predominant fibroids before UAE between the T2 high group and the control group. In the T2 high group, only one patient had a fibroid with a SI equal to that of the myometrium, while the remaining 13 demonstrated fibroids with a higher SI than normal myometrium.
Cramping pain occurred in all patients after UAE and was managed via an intravenous patient-controlled analgesic pump. Pain began to subside approximately 8-10 hours after UAE, and all patients were able to be discharged the next day and completely recovered after 1-2 weeks.
With regard to treatment effects, 13 (92.9%) of 14 patients from the T2 high group demonstrated complete necrosis of predominant fibroids (Fig. 1), which was not statistically significant when compared with 27 (96.4%) of 28 patients in the control group. Two patients showed incomplete necrosis of the fibroids, one in each group, respectively. One patient in the control group had a 4.5 cm submucosal myoma, which was reduced to 1.3 cm after UAE. However, the viability of the fibroid was still seen, and a hysteroscopic resection was recommended, but the patient refused any further procedure. The other patient in the T2 high group had multiple myomas, and the predominant fibroid was located in the lower uterine segment. Multiple myomas in the uterine body revealed complete necrosis after UAE, but a predominant fibroid in the lower uterine segment was not devascularized. Surgery was recommended, but the patient refused. One patient who had undergone a myomectomy three times before UAE demonstrated an 80% volume reduction after UAE, where the pathologic exam before UAE revealed extensive edema and increased vascularity in a specimen of myomectomy (Fig. 2). Spontaneous vaginal expulsion of the predominant fibroid occurred in one patient in the T2 high group and in two patients from the control group. The pathologic exam performed on the patient in the T2 high group revealed infarcted leiomoyma (Fig. 3).
The mean volume of the predominant fibroids in the T2 high group decreased by 61.7% at three months, from 144.4 ± 97.4 cm3 to 55.3 ± 51.3 cm3, which was significantly higher than the volume reduction rates of 42.1%, from 141.0 ± 50.8 cm3 to 81.6 ± 22.7 cm3, noted in the control group (p < 0.001).
The mean volume of the uterus in the T2 high group and in the control group decreased by 47.1% (from 399.0 cm3 ± 143.6 to 208.6 cm3 ± 87.0) and 38.8% (from 407.0 cm3 ± 239.8 to 244.7 cm3 ± 144.6), respectively, but did not decrease significantly.
Clinical outcomes are summarized in Table 2. Symptom improvements were reported with respect to menorrhagia and dysmenorrhea after UAE. Changes in symptom scores (baseline score minus follow-up score) for menorrhagia and dysmenorrhea were 4.9 and 7.5 in the T2 high group , 5.0 and 7.7 in the control group, respectively, representing a significant resolution of symptoms (p < 0.01), but no statistically significant differences between the two groups (p > 0.05). Mid-term follow-up MRI in three patients revealed persistent necrosis of the fibroids with further shrinkage of the fibroids. Symptoms were continuously relieved at mid-term follow-up. A single major complication was found in one patient with an 8-cm fibroid in the T2 high group, and was readmitted for pain control and conservative management for three days.
Since MR imaging more accurately detects and characterizes pelvic pathologies such as adenomyosis, including its soft tissue characterization, multiplanar imaging capabilities, and dynamic enhancement potential, it is now an established diagnostic modality as well as a treatment planning tool before UAE (14-16). In one study, MR imaging changed the initial diagnoses in 18% of patients, and immediate clinical management in 22% of patients (17).
Leiomyomas with the same collagen content as normal myometrium tend to have an SI almost equal to that of myometrium. When the collagen fiber content increases, the SI decreases, especially on T2WI (8). Leiomyomas with increased signal intensity on T2WI have a tendency to show a high degree of both cellularity and proliferative activity. Cellular leiomyomas, which are composed of compact smooth muscle cells, have relatively higher SI on T2WI and may demonstrate enhancement on contrast-enhanced images. Like a case in our study, extensive edema in the interstitial space is also a reason for high SI on T2WI with marked enhancement (9). In cases of rare myxoid leiomyomas, MR imaging shows that tumors contain abundant myxoid material between smooth muscle cells. The myxoid portion has high signal intensity on T2WI and enhances well except for small foci of mucinous lakes or clefts. Delayed and prolonged enhancement is seen because of the presence of a myxoid stroma (16). Degenerated leiomyomas have a variable appearance on T2WI. Leiomyomas with hyaline or calcific degeneration are generally low in SI, whereas those with cystic degeneration are generally very high in SI. However, the cystic areas do not enhance well and can be distinguished from other types of leiomyomas.
The SI of leiomyomas on T2WI has been regarded as an important factor in considering patient selection for various treatment modalities. High SI leiomyomas with high SI on T2WI are not appropriate for MR-guided focused ultrasound, in which 20% more patients with fibroids showing high SI receive reinterventional treatment at two years than those with low SI myomas (4). However, high SI fibroids are expected to be responsive to gonadotrophin-releasing hormone agonists (5, 6).
Only a few studies with UAE treatment for fibroids with high SI on T2WI with clinical outcomes have been reported to date (10, 18). Burn et al. (10) reported that leiomyomas with a high signal intensity on T2WI were predictive of a good prognosis. deSouza et al. (18) found that leiomyomas with a high SI on initial T2WI showed a significantly greater volume reduction of 55.8% than those with a low SI (32.5%). Both studies enrolled patients with multiple fibroids; 18 patients with 32 leiomyomas and 11 patients with 45 leiomyomas, respectively. However, others reported no correlation between T2WI SI and leiomyoma volume reduction after UAE (19, 20). Most studies regarding fibroids and T2WI SI have included multiple myomas in each patient.
According to Harman's study, volume reduction of the fibroid after UAE was more prominent in fibroids that had a marked contrast enhancement on T1-weighted images as well as a high SI on T2WI. They concluded that the increased contrast enhancement of a fibroid is indicative of a lesion with increased vascularity and is expected to be predictive of a better response.
Recently, Hecht et al. (19) suggested that the apparent diffusion coefficient (ADC) of leiomyomas can be used to predict volumetric response following UAE. In their study of 11 patients with 28 leiomyomas, they suggested a significant correlation between the volume reduction of fibroids and ADC, but no correlation with relative T2WI SI. One possible reason for the discrepancy regarding the correlation between the volume reduction of the fibroid and T2WI SI may be that multiple fibroids including small ones in each patient were enrolled, which sometimes can lead to errors in the measurement of fibroid sizes. In contrast, our study enrolled only predominant fibroids with high SI on T2WI in each patient and compared them with low SI fibroids; this comparison demonstrated a significant volume reduction of the predominant fibroid.
Symptoms of menorrhagia and dysmenorrhea were considerably improved after UAE, indicating that UAE for fibroids with high SI on T2WI was effective for controlling symptoms as well as fibroid volume reduction. However, one limitation of our present study was the small number of patients; further studies with a larger population size are needed.
In conclusion, UAE was effective for treating fibroids with high SI on T2WI. The mean volume reduction rate three months after UAE was greater in the T2 high group than in the control group.
Figures and Tables
 | Fig. 136-year-old woman with uterine leiomyoma.
A. Sagittal T2-weighted magnetic resonance (MR) image demonstrates 6.2-cm uterine leiomyoma with high signal intensity. B. Gadolinium-enhanced T1-weighted MR image corresponding to (A) contrast enhancement of fibroid is demonstrated (arrows). C. T2-weighted MR image obtained three months after embolization reveals 40% volume reduction of leiomyoma (arrows). D. Gadolinium-enhanced T1-weighted MR image corresponding to (C) complete necrosis (arrows) of fibroid focal hemorrhage (arrowhead), which is also noted as high signal intensity on non-contrast T1-weighted image (not shown) are demonstrated.
|
 | Fig. 239-year-old woman with history of myomectomy on three previous occasions.
A. Sagittal T2-weighted magnetic resonance (MR) image demonstrates 9.2-cm uterine leiomyoma with high signal intensity. B. Gadolinium-enhanced T1-weighted MR image reveals uterine leiomyoma with contrast enhancement (arrows). C. T2-weighted MR image obtained three months after embolization reveals 80% volume reduction of fibroid (arrows). D. Histologic examination (original magnification × 100; hematoxylin-eosin stain) in specimen of myomectomy before embolization shows leiomyoma with extensive edematous stroma (arrowheads) and prominent blood vessels (arrows), suggesting increased vascularity.
|
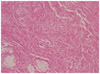 | Fig. 3Hematoxylin and eosin staining of expelled leiomyoma demonstrates extensive necrosis, which is consistent with infarcted leiomyoma (original magnification 400 ×). |
References
1. Walker WJ, Pelage JP. Uterine artery embolisation for symptomatic fibroids: clinical results in 400 women with imaging follow up. BJOG. 2002. 109:1262–1272.
2. Spies JB, Ascher SA, Roth AR, Kim J, Levy EB, Gomez-Jorge J. Uterine artery embolization for leiomyomata. Obstet Gynecol. 2001. 98:29–34.
3. Hovsepian DM, Siskin GP, Bonn J, Cardella JF, Clark TW, Lampmann LE, et al. Quality improvement guidelines for uterine artery embolization for symptomatic leiomyomata. J Vasc Interv Radiol. 2009. 20:7 Suppl. S193–S199.
4. Funaki K, Fukunishi H, Sawada K. Clinical outcomes of magnetic resonance-guided focused ultrasound surgery for uterine myomas: 24-month follow-up. Ultrasound Obstet Gynecol. 2009. 34:584–589.
5. Oguchi O, Mori A, Kobayashi Y, Horiuchi A, Nikaido T, Fujii S. Prediction of histopathologic features and proliferative activity of uterine leiomyoma by magnetic resonance imaging prior to GnRH analogue therapy: correlation between T2-weighted images and effect of GnRH analogue. J Obstet Gynaecol (Tokyo 1995). 1995. 21:107–117.
6. Takahashi K, Okada M, Imaoka I, Sugimura K, Miyazaki K. Value of magnetic resonance imaging in predicting efficacy of GnRH analogue treatment for uterine leiomyoma. Hum Reprod. 2001. 16:1989–1994.
7. Harman M, Zeteroğlu S, Arslan H, Sengül M, Etlik O. Predictive value of magnetic resonance imaging signal and contrast-enhancement characteristics on post-embolization volume reduction of uterine fibroids. Acta Radiol. 2006. 47:427–435.
8. Swe TT, Onitsuka H, Kawamoto K, Ueyama T, Tsuruchi N, Masuda K. Uterine leiomyoma: correlation between signal intensity on magnetic resonance imaging and pathologic characteristics. Radiat Med. 1992. 10:235–242.
9. Murase E, Siegelman ES, Outwater EK, Perez-Jaffe LA, Tureck RW. Uterine leiomyomas: histopathologic features, MR imaging findings, differential diagnosis, and treatment. Radiographics. 1999. 19:1179–1197.
10. Burn PR, McCall JM, Chinn RJ, Vashisht A, Smith JR, Healy JC. Uterine fibroleiomyoma: MR imaging appearances before and after embolization of uterine arteries. Radiology. 2000. 214:729–734.
11. Orsini LF, Salardi S, Pilu G, Bovicelli L, Cacciari E. Pelvic organs in premenarcheal girls: real-time ultrasonography. Radiology. 1984. 153:113–116.
12. Spies JB, Spector A, Roth AR, Baker CM, Mauro L, Murphy-Skrynarz K. Complications after uterine artery embolization for leiomyomas. Obstet Gynecol. 2002. 100(5 Pt 1):873–880.
13. Goodwin SC, Bonilla SM, Sacks D, Reed RA, Spies JB, Landow WJ, et al. Reporting standards for uterine artery embolization for the treatment of uterine leiomyomata. J Vasc Interv Radiol. 2001. 12:1011–1020.
14. Yamashiro T, Gibo M, Utsunomiya T, Murayama S. Huge uterine leiomyoma with adenomyotic cysts mimicking uterine sarcoma on MR imaging. Radiat Med. 2007. 25:127–129.
15. Hamlin DJ, Pettersson H, Fitzsimmons J, Morgan LS. MR imaging of uterine leiomyomas and their complications. J Comput Assist Tomogr. 1985. 9:902–907.
16. Ueda H, Togashi K, Konishi I, Kataoka ML, Koyama T, Fujiwara T, et al. Unusual appearances of uterine leiomyomas: MR imaging findings and their histopathologic backgrounds. Radiographics. 1999. 19 Spec No:S131–S145.
17. Rajan DK, Margau R, Kroll RR, Simons ME, Tan KT, Jaskolka JD, et al. Clinical utility of ultrasound versus magnetic resonance imaging for deciding to proceed with uterine artery embolization for presumed symptomatic fibroids. Clin Radiol. 2011. 66:57–62.
18. deSouza NM, Williams AD. Uterine arterial embolization for leiomyomas: perfusion and volume changes at MR imaging and relation to clinical outcome. Radiology. 2002. 222:367–374.
19. Hecht EM, Do RK, Kang SK, Bennett GL, Babb JS, Clark TW. Diffusion-weighted imaging for prediction of volumetric response of leiomyomas following uterine artery embolization: a preliminary study. J Magn Reson Imaging. 2011. 33:641–646.
20. Jain TP, Srivastava DN, Sahu RP, Thulkar S, Sharma S, Mittal S, et al. Uterine artery embolization for symptomatic fibroids with imaging follow up. Australas Radiol. 2007. 51:246–252.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download