Abstract
Objective
To investigate the role of lumbosacral radiculography using 3-dimentional (3D) magnetic resonance (MR) rendering for diagnostic information of symptomatic extraforaminal stenosis in lumbosacral transitional vertebra.
Materials and Methods
The study population consisted of 18 patients with symptomatic (n = 10) and asymptomatic extraforaminal stenosis (n = 8) in lumbosacral transitional vertebra. Each patient underwent 3D coronal fast-field echo sequences with selective water excitation using the principles of the selective excitation technique (Proset imaging). Morphologic changes of the L5 nerve roots at the symptomatic and asymptomatic extraforaminal stenosis were evaluated on 3D MR rendered images of the lumbosacral spine.
Results
Ten cases with symptomatic extraforaminal stenosis showed hyperplasia and degenerative osteophytes of the sacral ala and/or osteophytes at the lateral margin of the L5 body. On 3D MR lumbosacral radiculography, indentation of the L5 nerve roots was found in two cases, while swelling of the nerve roots was seen in eight cases at the exiting nerve root. Eight cases with asymptomatic extraforaminal stenosis showed hyperplasia and degenerative osteophytes of the sacral ala and/or osteophytes at the lateral margin of the L5 body. Based on 3D MR lumbosacral radiculography, indentation or swelling of the L5 nerve roots was not found in any cases with asymptomatic extraforaminal stenosis.
Conclusion
Results from 3D MR lumbosacral radiculography Indicate the indentation or swelling of the L5 nerve root in symptomatic extraforaminal stenosis. Based on these findings, 3D MR radiculography may be helpful in the diagnosis of the symptomatic extraforaminal stenosis with lumbosacral transitional vertebra.
A lumbosacral transitional vertebra (LSTV) is one in which the last lumbar vertebra shows elongation of its transverse process, with varying degrees of fusion to the first sacral segment and is common in the general population, with a reported prevalence of 4-30% (1, 2). The clinical significance of LSTVs has been controversial. In 1917, Bertolotti described the assimilation of the fifth lumbar vertebra into the sacrum and its association with lower back pain. Since then, the term Bertolotti's syndrome has been used to define the presence of a transverse mega-apophysis in a lumbar vertebra with transitional characteristics associated with lower back pain (3, 4). In 1984, Wiltse et al. (5) first demonstrated that the spinal nerve root could be compressed between the L5 transverse process and the sacral ala. In 1997, a case of extraforaminal stenosis at the intervertebral space below a lumbosacral transitional vertebra was reported by Abe et al. (6). Such a radiculopathy originating from the encroaching foramen below a transitional vertebra has been rarely observed. Hashimoto et al. (7) reported that in nine patients with LSTV, affected roots were compressed between the transverse process of the last lumbar segment and the sacral ala. In their study, coronal MR images demonstrated the root impingement directly in the far lateral zone in all patients. They concluded that a transitional vertebra was the cause of extraforaminal stenosis and that MR images using the coronal plane were useful in the assessment of extraforaminal stenosis. Moon et al. (8) studied changes in the size of the anterior primary division of the L5 nerve root with computed tomography (CT) in the presence of foraminal/extraforaminal entrapment of the L5 nerve root. They indicated that an asymmetric enlargement of the anterior primary division on the L5 nerve root on CT scans was meaningfully associated with a foraminal or extraforaminal entrapment of the L5 nerve root on the lumbosacral junction. If the acquisition of axial images is not perpendicular to the L5 nerve root, the diameter of the bilateral L5 nerve roots at the sacral alar level in asymptomatic cases can have different sizes.
Detection of the morphologic changes in the nerve root for use as diagnostic information in symptomatic extraforaminal stenosis is very important. Unfortunately, conventional axial, sagittal, and coronal images often have not been useful in the evaluation of detailed morphologic changes of the lumbosacral nerve root caused by extraforaminal stenosis. Also, the relationship between the radiologic measurements and the clinical symptoms is not straightforward. Some studies estimated that at least 20% of the pain-free elderly population has radiologic spinal stenosis (9, 10).
The purpose of this study was to investigate the significance of lumbosacral radiculography using three dimensional (3D) MR rendering to obtain diagnostic information of symptomatic extraforaminal stenosis in the lumbosacral transitional vertebra.
We retrospectively reviewed 300 consecutive lumbar spine MRI studies performed from October 2010 to August 2011 on patients presenting with lumbar radiculopathy or back pain. Eighteen patients with morphologic unilateral extraforaminal stenosis in lumbosacral transitional vertebra were selected. The study population consisted of 18 patients (age range, 56-80 years; mean ages, 66.7 years; 7 men, 11 women) with unilateral symptomatic (n = 10) and asymptomatic extraforaminal stenosis (n = 8) in lumbosacral transitional vertebra. All diagnoses were confirmed by observation at surgery (n = 3), as well as by provocative selective nerve root injection and clinical symptoms (n = 15). Diagnosis of symptomatic extraforaminal stenosis on the operation field was confirmed by a little space between sacral ala and L5 transverse process, as well as by complete pain relief after decompression surgery. Provocative selective nerve root injection for confirmation of the radiculopathy was performed in the ipsilateral L5 nerve root. Symptomatic extraforaminal stenosis was evaluated by pain reproduction on injection of the contrast medium during selective nerve root injection. In two of three cases that underwent surgical treatment, provocative selective nerve root injection was performed before surgery. However, a relapse of symptoms occurred within six months after provocative selective nerve root injection was developed. All patients had histories of unilateral radicular pain (n = 14) or back pain (n = 4). Inclusion criteria for the diagnosis of extraforaminal stenosis in lumbosacral junction were: 1) lumbosacral transitional vertebra, 2) lateral osteophytes at the L5 lower body, transverse process of L5 and/or sacral ala, and 3) narrow lumbosacral bony tunnel. Nakao et al. (11) coined the term "lumbosacral bony tunnel". They defined this bony tunnel as the transverse process of L5, sacral ala, and the bony spur of the vertebral body of L5. The narrow lumbosacral bony tunnel was identified by visual observation without quantitative measurements. Two radiologists reviewed the images in consensus and without knowledge of the patients' symptoms. Patients were excluded if they had a history of spinal trauma, infection, or previous lumbar spine surgery.
In all cases with symptomatic and asymptomatic extraforaminal stenosis, MR imaging was performed. Further, CT scans were performed in five patients. Magnetic resonance imaging was performed using a 1.5-T scanner (Interna, Philips Medical System, Best, The Netherlands) with a spine array coil. With respect to spin-echo sequences, axial and sagittal T1-(583/12 [repetition time msec/echo time msec]) and turbo-T2-weighted images (3800/128) were obtained. 3D coronal fast-field echo (FFE) sequences with selective water excitation were acquired using the principles of the selective excitation technique (Proset imaging) with the following acquisition parameters: 1 mm section thickness without an overlapping section gap; 250 mm FOV; 256 × 256 matrix; TR, 27.8 ms; TE, 13.8 ms; 8° flip angle, and 2 signal intensity acquisitions. Forty coronal source FFE images for each subject were obtained. In order to obtain images of all lumbosacral nerve roots and dorsal root ganglia (DRG), we set the imaging plane to be parallel to the longitudinal axis of the lumbar spinal canal and centered on the level of the L3 vertebral body. One parallel regional saturation slab was added to suppress the signal intensity from the vessels. The resultant whole-imaging slab had an anteroposterior thickness of 4 cm, which could fully cover the intervertebral foramina region and extraforaminal zone from the anterior two-thirds of the vertebral body to the anterior margin of the spinous process. For image processing, Aquarius 3D workstation equipped with commercially available automated analysis 3D rendering software (TeraRecon Inc, San Mateo, CA, USA) was used.
The spindle-shaped nerve root in the extraforaminal or foraminal zones was defined as DRG on Proset source images or 3D MR radiculography. In general, the nerve root that exited the spine at a particular level is referred to as the exiting nerve root. Another segment of the nerve root goes across the disc and exits the spine at the next level below and is called the traversing nerve root. On 3D MR radiculography, the nerve root in the extraforaminal zone beyond the DRG was defined as the exiting nerve root. The proximal nerve segment between the thecal sac and DRG was defined as the traversing nerve root (Fig. 1A).
Indentation or swelling of the nerve roots and DRG at the side of both symptomatic and asymptomatic extraforaminal stenosis were evaluated on 3D MR rendering images of the lumbosacral spine. Morphologic changes in the nerve root caused by symptomatic extraforaminal stenosis were compared with those of the contralateral nerve root on 3D MR lumbosacral radiculography. In all cases, we measured the tilting angle of the nerve root using a line parallel to the thecal sac and another line passing through the center of the nerve root and parallel to its long axis. The tilting angle of the nerve root was defined as abnormal if the nerve shifted upward with the angle offset more cephalad compared with the contralateral nerve root. Subsequently, the tilting angle of the nerve root on the symptomatic side was compared with the asymptomatic contralateral side on 3D MR rendered images. Axial Proset multi-planar reconstruction (MRP) images were selected for quantitative analysis of the L5 nerve root width (Fig. 1B). The width of the transversing nerve root was measured at the midpoint perpendicular to the longitudinal axis. The width of the exiting nerve was measured at just 1 cm caudal from the distal end of the DRG. The width of the DRG was measured vertically at the midpoint perpendicular to the longitudinal axis of the DRG. The widths of the symptomatic nerve root were compared with those in the contralateral asymptomatic nerve root on axial Proset MPR images. The relationship between morphologic changes in the symptomatic nerve root on 3D MR lumbosacral radiculography and surgical results or a selective nerve root block for confirmation of the radiculopathy was subsequently analyzed.
Inter-and intra-observer variability related to findings on 3D MR radiculography was assessed using kappa statistics. A kappa value of less than 0.40 indicated poor agreement; 0.41 to 0.60, moderate agreement; 0.61 to 0.80, substantial agreement; and 0.81 or greater, almost perfect agreement. A paired t test was used to determine whether there was a statistically significant difference between widths of symptomatic and asymptomatic contralateral nerve roots in symptomatic extraforaminal stenosis. Differences in width in both sides of the L5 nerve roots in the control groups was evaluated. A p value less than 0.05 was considered as statistically significant. Analyses were performed with SPSS Version 12.0 (SPSS, Chicago, IL, USA). Our study was approved by the institutional review board of our hospital.
The left side was involved in eight cases while the right side was in two cases. A CT and conventional MR scan showed hyperplasia and degenerative osteophytes of the S1 ala and the lateral margin of the L5 body in three cases (Fig. 2B-D). Another three cases showed hyperplasia and degenerative osteophytes of the sacral ala. Osteophytes at the lateral margin of the L5 body were demonstrated in four cases (Fig. 3B-D). On 3D MR lumbosacral radiculography, indentation of the L5 nerve roots was found in two cases, while swelling of the nerve roots was seen in eight cases (Fig. 2E) and the location of the indentation was the exiting nerve root (Fig. 3E). Tilting angle abnormality of the L5 nerve root was observed in five cases. The L5 nerve root shifted upward with the angle offset more cephalad compared with the contralateral nerve root. The mean width of the exiting nerve root with indentation was 1.09 mm. Widths of the symptomatic nerve roots with swelling were significantly larger than those of the asymptomatic nerve roots on axial Proset MPR images paired t test, p < 0.05 (Table 1).
Initial treatment included provocative selective nerve root injection in nine patients and surgical decompression in one case. Pain reproduction during selective nerve root injection showed concordant pain. Selective nerve root block for treatment was performed and although it showed concordant pain, a relapse of symptoms was observed within six months after treatment in two of six cases with provocative selective nerve root injection. Surgery was performed in three cases with left extraforaminal stenosis. The patient experienced complete pain relief after decompression surgery. On the operation field, there was a little space between sacral ala and the L5 transverse process; consequently, surgeons drilled out the lateral pars and upper lateral part of the L5-S1 facet and the L5 nerve root was compressed between the L5 transverse process and the sacral ala. Our study found that there was an apparent correlation between nerve root indentation and swelling on 3D MR radiculography and clinical symptoms including provocative selective nerve root block and postoperative results.
Both the left side and right side were involved in four cases of symptomatic extraforaminal stenosis, which were confirmed by provocative selective nerve root injection and clinical symptoms. Four patients with extraforaminal stenosis in L5-S1 complained of back pain without radiculopathy. In another four cases, pain reproduction during selective nerve root injection showed concordant pain at different levels and sides.
On CT and/or MR imaging, seven cases with asymptomatic extraforaminal stenosis showed hyperplasia and degenerative osteophytes of the sacral ala (Fig. 4A). Osteophytes at the lateral margin of the L5 body and sacral ala were detected in one case. On 3D MR lumbosacral radiculography, swelling or indentation of the L5 nerve roots was absent in all cases (Fig. 4B). Tilting angle abnormality of the L5 nerve root was observed in three cases. No statistically significant difference was observed between the widths of the right L5 nerve root and those of the left L5 nerve root (paired t test).
Lumbosacral transitional vertebras are congenital spinal anomalies defined as either sacralization of the lowest lumbar segment or lumbarization of the most superior sacral segment of the spine. In 1984, Castellvi et al. (12) described a radiographic classification system identifying four types of lumbosacral transitional vertebrae based on their morphologic characteristics. The clinical significance of the LSTV relates to Bertolotti syndrome (lower back pain) and extraforaminal stenosis leading to nerve root entrapment.
Extraforaminal entrapment of the L5 nerve root has recently drawn attention as a cause of sciatic pain, and several cadaveric studies have been reported on lumbosacral ligaments and/or osteophytes of the L5-S1 vertebral body as possible causes of entrapment of the L5 nerve root. Transfeldt et al. (13) and Olsewski et al. (14) reported that lumbosacral ligaments could compress the L5 spinal nerve. Nathan et al. (15) conducted a study on forty-two cadavers and reported finding that a lumbosacral tunnel consisting of osteophytes of the L5 vertebral body, the lumbosacral ligaments, and the sacral ala caused entrapment of the L5 nerve root. Otani et al. (16) found that 13% of patients in the symptomatic group with radiculopathy and 11% in the asymptomatic control group had transitional vertebra. They noted that neither the presence nor type of transitional vertebra affected the incidence of such symptoms. Matsumoto et al. (17) reported that extraforaminal entrapment of the L5 nerve root in the lumbosacral tunnel could cause L5 radiculopathy, and that osteophytes of L5-S1 vertebral bodies were a major cause of the entrapment. In our study, CT and conventional MR scan of the symptomatic extraforaminal stenosis showed hyperplasia and degenerative osteophytes of the S1 ala and the lateral margin of the L5 body in three cases. Another three cases showed hyperplasia and degenerative osteophytes of the sacral ala. Osteophytes at the lateral margin of the L5 body were demonstrated in four cases. Further, seven cases with asymptomatic extraforaminal stenosis showed hyperplasia and degenerative osteophytes of the sacral ala (Fig. 2A). Osteophytes at the lateral margin of the L5 body and sacral ala were detected in one case. The relationship between the morphologic stenosis and the clinical symptoms is not straightforward. We suggest that not all of the extraforaminal stenosis caused by osteophytes of the L5-S1 in LSTV results in symptomatic extraforaminal stenosis. The degree of stenosis and morphologic changes of the affected nerve root caused by stenosis are important in the diagnosis of the symptomatic extraforaminal stenosis. In general, the diagnosis of extraforaminal stenosis has been based on the presence of neurological deficits caused by the L5 nerve root compression and on radiological findings, including CT evidence of prominent osteophytes at the posterolateral borders of the L5 and S1 bodies and radiculographic demonstration of L5 nerve root compression between these osteophytes and the sacral ala. When a selective L5 nerve root block relieves pain, the diagnosis is confirmed. In many instances, lumbar spine MRI has been reported without access to CT results, either because these have not been performed or were unavailable. A correct diagnosis using a single imaging modality may not be ideal. Morphological changes in the extraforamen have been well-demonstrated on conventional MR images; however, it is often difficult to differentiate between symptomatic and asymptomatic extraforaminal stenosis in lumbosacral transitional vertebra on conventional MRI alone. The best images are obtained on coronal MR imaging. The nerve root may be seen compressed between the hyperplastic transverse process of the lumbosacral transitional vertebra and the adjacent sacral ala (7). However, detailed morphologic changes such as indentation, swelling, and tilting angle abnormality of L5 nerve root cannot be demonstrated on coronal MR images in cases of symptomatic extraforaminal stenosis.
The Proset is a selective excitation technique used to suppress either water or fat by exploiting differences in the resonance frequencies of water and fat. Using Proset, the signal intensity of fat was completely suppressed and the details of the nerve root and DRG were delineated in the current study. The acquisition time for Proset imaging was four minutes. We found that 3D MR lumbosacral radiculography using Proset imaging revealed an excellent full view of the nerve roots.
In our study, using 3D MR lumbosacral radiculography, symptomatic extraforaminal stenosis revealed indentation (n = 2) or swelling (n = 8) of the L5 nerve root. However, there was not a significant swelling or indentation at the L5 nerve root in cases of asymptomatic extraforaminal stenosis. Although the number of patients was small, the most significant findings on 3D MR radiculography in patients with symptomatic extraforaminal stenosis were the indentation and swelling of the L5 nerve root. Moon et al. (8) reported that an asymmetric enlargement of the L5 nerve root on CT scans was associated with a foraminal or extraforaminal entrapment of the L5 nerve root on the lumbosacral junction. However, another study revealed that the L5 nerve roots were compressed between the transverse process of the last lumbar segment and the sacral ala in all cases (7). In cases where the acquisition of axial CT or MR images had not been parallel to the L5 nerve root, the asymmetric size of the nerve roots in cases without symptomatic extraforaminal stenosis have resulted in the incorrect diagnoses of extraforaminal stenosis. Unfortunately, in patients with degenerative or congenital scoliosis, acquisition of axial images parallel to the nerve root usually has not been easily accomplished. Axial CT or MR cannot often demonstrate morphologic change or tilting angle abnormality of the nerve root. In most studies, findings relating to variable morphologic changes of the L5 nerve root have not been mentioned. Further, in patients without radiculopathy, detection of morphologic extraforamoinal stenosis on conventional MR imaging or CT may not be uncommon. Although there was evidence of narrowed lumbosacral bony tunnels caused by osteophytes of L5-S1 on conventional MR imaging in eight asymptomatic cases, no significant abnormal findings of the nerve root were demonstrated on 3D MR lumbosacral radiculography. However, the tilting angle abnormality was detected in both symptomatic and asymptomatic extraforaminal stenosis. We suggest that nerve root displacement caused by hyperplasia or spurs of the bony structures may not be relevant to clinical symptoms.
In conclusion, 3D MR lumbosacral radiculography demonstrated indentation or swelling of the L5 nerve root in the symptomatic extraforaminal stenosis of L5-S1. Based on this, 3D MR radiculography may be helpful in the diagnosis of the symptomatic extraforaminal stenosis with LSTV.
Figures and Tables
 | Fig. 1L5 nerve root measurement by 3-dimensional magnetic resonance (3D MR) lumbosacral radiculography and axial Proset multi-planar reconstruction (MPR) images.
On 3D MR radiculography (A), proximal nerve segment between thecal sac and dorsal root ganglion (DRG) is defined as traversing nerve root (arrow). Spindle-shaped nerve root in extraforaminal or foraminal zones is defined as DRG (blanked arrow), and nerve root in extraforaminal zone beyond DRG is defined as exiting nerve root (long arrow). Tilting angle of nerve root is measured using parallel line to thecal sac (black arrow) and another line (double arrows) passing through center of nerve root and spinal nerve and parallel to its long axis. On axial Proset MPR images (B) for measurement of right L5 nerve root width, diameters of exiting nerve root (small arrow), DRG (thick arrow), and traversing nerve root (long arrow) are measured.
|
 | Fig. 275-year-old man presenting with swelling of left L5 nerve root in symptomatic extraforaminal stenosis with lumbosacral transitional vertebra.
This patient complained of severe left leg pain. Sagittal T1-weighted image (A) of lumbar spine shows transitional lumbosacral junction. Lumbosacral transitional vertebra (arrow) is positioned above transitional disk and axial T1- (B) and T2- (C) weighted images reveal left extraforaminal stenosis (arrow) due to osteophytes at lateral margin of L5 body and degenerative hypertrophy of left ala (thin arrow). Osteophytes (arrow) at right lateral margin of L5 body are noted on axial CT (D). Tilting angle abnormality, swelling of left L5 dorsal root ganglion (small arrow), and exit nerve (arrow) can be seen on 3-dimensional magnetic resonance lumbosacral radiculography (E). Patient obtained complete pain relief after decompression surgery.
|
 | Fig. 364-year-old woman presenting with indentation of right L5 nerve root in symptomatic extraforaminal stenosis with lumbosacral transitional vertebra.
This patient complained of severe right leg pain. Sagittal T1-weighted image (A) of lumbar spine shows transitional lumbosacral junction. Lumbosacral transitional vertebra (arrow) is positioned above transitional disk. Axial T1- (B) and T2- (C) weighted images reveal right extraforaminal stenosis (arrow) due to osteophytes at lateral margin of L5 body. Osteophytes (arrow) at right lateral margin of L5 body are noted on axial CT (D). Tilting angle abnormality and indentation of right L5 exit nerve (arrow) are seen on 3-dimensional MR lumbosacral radiculography (E). Pain reproduction during selective nerve root injection showed concordant pain.
|
 | Fig. 475-year-old man with asymptomatic extraforaminal stenosis.
This patient complained of lower back pain without radiculopathy. Axial T1-weighted image (A) shows left extraforaminal stenosis (small arrow) due to hyperplasia and osteophytes (arrow) of sacral ala. 3-dimensional magnetic resonance lumbosacral radiculography (B) revealed no significant morphologic change at left L5 nerve root.
|
Table 1
Comparison of Quantitative Measurements between Symptomatic and Asymptomatic Extraforaminal Stenosis on Axial Proset MPR images
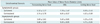
Note.- Difference between widths of ipsilateral symptomatic spinal L5 nerve and those of contralateral spinal L5 nerve are statistically significant in transverse and exit nerve roots (paired t test, p < 0.05). There is no statistically significant difference between widths of ipsilateral L5 nerve and those of contralateral L5 nerve in asymptomatic extraforaminal stenosis (paired t test, p > 0.05). DRG = dorsal root ganglion, Ipsilateral = side of extraforaminal stenosis, Contralateral = contralateral side of extraforaminal stenosis, MPR = multi-planar reconstruction
References
1. Bron JL, van Royen BJ, Wuisman PI. The clinical significance of lumbosacral transitional anomalies. Acta Orthop Belg. 2007. 73:687–695.
2. O'Driscoll CM, Irwin A, Saifuddin A. Variations in morphology of the lumbosacral junction on sagittal MRI: correlation with plain radiography. Skeletal Radiol. 1996. 25:225–230.
3. Elster AD. Bertolotti's syndrome revisited. Transitional vertebrae of the lumbar spine. Spine (Phila Pa 1976). 1989. 14:1373–1377.
4. Quinlan JF, Duke D, Eustace S. Bertolotti's syndrome. A cause of back pain in young people. J Bone Joint Surg Br. 2006. 88:1183–1186.
5. Wiltse LL, Guyer RD, Spencer CW, Glenn WV, Porter IS. Alar transverse process impingement of the L5 spinal nerve: the far-out syndrome. Spine (Phila Pa 1976). 1984. 9:31–41.
6. Abe E, Sato K, Shimada Y, Okada K, Yan K, Mizutani Y. Anterior decompression of foraminal stenosis below a lumbosacral transitional vertebra. A case report. Spine (Phila Pa 1976). 1997. 22:823–826.
7. Hashimoto M, Watanabe O, Hirano H. Extraforaminal stenosis in the lumbosacral spine. Efficacy of MR imaging in the coronal plane. Acta Radiol. 1996. 37:610–613.
8. Moon KH, Jang JS, Lee SH, Lee SC, Lee HY. The role of computed tomography in the presurgical diagnosis of foraminal entrapment of lumbosacral junction. J Korean Neurosurg Soc. 2010. 47:1–6.
9. Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990. 72:403–408.
10. Deyo RA, Ciol MA, Cherkin DC, Loeser JD, Bigos SJ. Lumbar spinal fusion. A cohort study of complications, reoperations, and resource use in the Medicare population. Spine (Phila Pa 1976). 1993. 18:1463–1470.
11. Nakao S, Yoshida M, Yamada H, Hashizume H. A new 3-dimensional computed tomography imaging method to diagnose extraforaminal stenosis at the lumbosacral junction. J Spinal Disord Tech. 2010. 23:e47–e52.
12. Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976). 1984. 9:493–495.
13. Transfeldt EE, Robertson D, Bradford DS. Ligaments of the lumbosacral spine and their role in possible extraforaminal spinal nerve entrapment and tethering. J Spinal Disord. 1993. 6:507–512.
14. Olsewski JM, Simmons EH, Kallen FC, Mendel FC. Evidence from cadavers suggestive of entrapment of fifth lumbar spinal nerves by lumbosacral ligaments. Spine (Phila Pa 1976). 1991. 16:336–347.
15. Nathan H, Weizenbluth M, Halperin N. The lumbosacral ligament (LSL), with special emphasis on the "lumbosacral tunnel" and the entrapment of the 5th lumbar nerve. Int Orthop. 1982. 6:197–202.
16. Otani K, Konno S, Kikuchi S. Lumbosacral transitional vertebrae and nerve-root symptoms. J Bone Joint Surg Br. 2001. 83:1137–1140.
17. Matsumoto M, Chiba K, Nojiri K, Ishikawa M, Toyama Y, Nishikawa Y. Extraforaminal entrapment of the fifth lumbar spinal nerve by osteophytes of the lumbosacral spine: anatomic study and a report of four cases. Spine (Phila Pa 1976). 2002. 27:E169–E173.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download