Abstract
Objective
We aimed to describe the imaging findings of multidetector CT coronary angiography (MDCTA) in cases of vasospastic angina (VA) and to determine the accuracy of MDCTA in the identification of VA as compared with invasive coronary angiography with an ergonovine provocation test (CAG with an EG test).
Materials and Methods
Fifty-three patients with clinically suspected VA were enrolled in this study. Two radiologists analyzed the stenosis degree, presence or absence of plaque, plaque composition, and a remodeling index of the related-segment in CAG with an EG test, which were used as a gold standard. We evaluated the diagnostic performances of MDCTA by comparing the MDCTA findings with those of CAG with an EG test.
Results
Among the 25 patients with positive CAG with an EG test, all 12 patients with significant stenosis showed no definite plaque with the negative arterial remodeling. Of the six patients with insignificant stenosis, three (50%) had non-calcified plaque (NCP), two (33%) had mixed plaque, and one (17%) had calcified plaque. When the criteria for significant stenosis with negative remodeling but no definite evidence of plaque as a characteristic finding of MDCTA were used, results showed sensitivities, specificities, positive predictive values (PPV), and negative predictive values (NPV) of 48%, 100%, 100%, and 68%, respectively.
The term coronary vasospastic angina (VA) denotes chest discomfort with classic features of angina pectoris that occurred at rest, usually at night, or during the early morning. The pain is often associated with a transient elevation of the ST segment greater than 2 mm on the electrocardiogram (1). Its cause is well known as vasospasm, a narrowing of the coronary arteries caused by the contraction of smooth muscle tissue in the vessel walls. Vasospasm is confirmed by conventional coronary angiography with provocation using acetylcholine or ergonovine (2). Several intravascular ultrasound (IVUS) studies have shown that early atherosclerosis with high incidence of negative arterial remodeling at the site of the focal spasm is a characteristic finding of VA (3, 4).
Multidetector CT coronary angiography (MDCTA) is a newly emerging alternative technique for noninvasive detection of coronary artery diseases. MDCTA allows assessment of the severity of coronary artery stenosis with high diagnostic accuracy (5-7), and offers additional information, including plaque composition and arterial remodeling (8-10). Therefore, MDCTA is a promising emerging modality for the evaluation of acute chest pain syndrome in the emergency department (11-13).
However, as far as we know, there has been no report of assessing imaging findings or diagnostic accuracy of MDCTA in patients with VA. Therefore, the aim of this study is to describe the imaging findings of MDCTA in VA and to determine the accuracy of MDCTA in identification of VA with invasive coronary angiography with an ergonovine provocation test (CAG with an EG test) as a gold standard.
Among the registry of 21,365 patients who underwent 64-slice MDCTA between January 2006 and December 2009 at our institute, we retrospectively selected patients according to following criteria; (a) clinically suspected as VA, and (b) underwent both MDCTA and CAG with an EG test within one month because of suspected VA. Patients were excluded if they had not undertaken both MDCTA and CAG with an EG test or if the MDCTA image showed poor quality. Two patients were excluded due to poor images on MDCTA. Finally, 53 patients were included in this study.
We investigated symptomatic status whether patients presented with acute chest pain in the emergency department or not (i.e. outpatient clinic). Institutional Review Board approval was obtained for this retrospective study and informed consent was waived.
Multidetector CT was performed using of a 64-slice MSCT scanner with a 0.42-s rotation time (Brilliance 64; Philips Medical Systems, Best, The Netherlands). A standard scanning protocol was applied, with a 64 × 0.625 mm section collimation, 420-msec rotation time, 120 kV tube voltage, and 600 mAs. A bolus of 80 mL (Iomeprol, Iomeron 400; Bracco, Milan, Italy) was intravenously injected at a rate of 4 mL/sec. Using a bolus tracking method with a power injector (CT Stellant, Medrad Inc. Indianola, IA), a region of interest was placed in the descending thoracic aorta and the scan was automatically initiated once a selected threshold (150 Hounsfield unit [HU]) was reached. The ECG of the patient was saved concurrently with the acquisitions for retrospective segmental data reconstruction. Patients with a heart rate > 70 beats/min received a 10 to 30 mg dose of intravenous esmolol (Brevibloc, Jeil Pharm. Co., Ltd., Seoul, Korea), before MDCTA imaging.
All MDCTA data sets were analyzed by two experienced cardiac radiologists (14 and 5 years) who were blinded to the clinical information, using a dedicated workstation (Brilliance, Philips Medical Systems, Best, The Netherlands). After making independent evaluations, a consensus interpretation was arrived at in order to obtain a final MDCTA diagnosis. Coronary artery stenosis was assessed with multiplanar reconstruction, maximum intensity projections, 3D volume rendered reconstruction, as well as image data sets with a 1-mm reconstructed slice thickness. LV function was assessed with 5-mm stacks by multiplanar reconstructions including 2-chamber, 4-chamber, and short-axis orientations.
We evaluated the following parameters by consensus: 1) stenosis degree (none, insignificant, and significant) of the related-segment in CAG with an EG test, 2) presence or absence of plaque, 3) plaque composition, and 4) remodeling index. Significant stenosis is defined as stenosis in more than 50% of the coronary artery diameter. Plaques were reported as non-calcified, calcified, or mixed plaques. Based on data from Leber et al. (14), we defined the noncalcified plaque, which is < 130 HU. Calcification was recognized as plaque with a density of > 130 HU on curved MPR images. Mixed plaque was characterized if the plaque area consisted of > 50% of non-calcified plaque. The remodeling index (RI) was the cross-sectional vessel area within the lesion divided by the reference vessel (non-diseased vessel immediately proximal to the lesion) cross-sectional area (15).
Coronary angiography was performed according to the conventional Judkins or Sones technique by an experienced cardiologist. Patients stopped calcium antagonists and oral nitrates for at least 48 hour prior to the performance of a coronary angiography. Patients with a significant fixed atherosclerotic stenosis (≥ 50% lumen diameter) were excluded from the spasm provocation test. A pharmacologic provocation test was performed using intracoronary ergonovine, according to methods described elsewhere (16). The appearance of total or subtotal occlusion of a major coronary artery, a greater than 2 mm depression or elevation of the ST segment on the ECG, or typical chest pain or both, was considered to be a manifestation of coronary artery vasospasm. CAG with EG tests were assessed by two experienced cardiologists who were blinded to clinical information. After making independent evaluations in the analysis of CAG with an EG test, a consensus interpretation was arrived at for a final diagnosis. If the stenotic segment was different between MDCTA and CAG with an EG test, this segment was regarded as a false lesion.
We determined the diagnostic performances of MDCTA findings for VA using CAG with an EG test as a reference standard. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy were evaluated. We also analyzed the diagnostic performances of MDCTA findings to determine whether or not they can be affected by the status of a patient's symptoms. We divided two acute chest pain cases to the emergency department or outpatient clinic.
Data were shown as absolute values and percentages. Results are expressed as the mean ± standard deviation.
The chi-square test was used for categorical and ordinal variables. A two-tailed p value < 0.05 was considered to be statistically significant. SPSS 16.0 (SPSS Inc., Chicago, IL) was used to performance of data analysis.
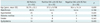
The characteristics of all 53 patients are shown in Table 1. They were divided into two groups depending on the result of the CAG with an EG test. No statistically significant differences in a demographic data and coronary risk factor were observed between the two groups. Considering the active state of chest pain, the prevalence of patients was 18 of 53 (34%) in the emergency room and 35 of 53 (66%) patients in the outpatient clinic.
A definitive diagnosis of VA was made by CAG with an EG test in 25 of 53 (47%) patients. Among the 25 patients with positive CAG with the EG test, 12 (48%) showed significant stenosis at the related segment on MDCTA, whereas six (24%) showed insignificant stenosis and seven (28%) were found to be normal. Of the 28 (53%) patients with a negative CAG with an EG test, 24 of 28 (86%) were normal and four of 28 (14%) showed insignificant stenosis (Table 2). There was no significant stenosis at the related segment of VA in patients with negative CAG with an EG test.
Among the 25 patients with positive CAG with an EG test, all 12 patients with significant stenosis showed no definite plaque with negative arterial remodeling in the related segment of the coronary artery (Figs. 1, 2). Of the six patients with insignificant stenosis (24%), three (50%) had noncalcified plaque (NCP), two (33%) had mixed plaque, and one (17%) had calcified plaque. However, negative remodeling was not observed in any of the patients with insignificant stenosis in the related segment of the coronary artery.
The sensitivity, specificity, positive predictive value, and negative predictive value for MDCTA on the basis of significant stenosis of the related segment were 52% (13 of 25 patients), 96% (27 of 28 patients), 93% (13 of 14 patients), and 69% (27 of 39 patients), respectively.
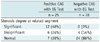
However, using criteria with significant stenosis using negative remodeling but no definite evidence of plaque as a characteristic finding on MDCTA provided sensitivities, specificities, positive predictive values, and negative predictive values of 48% (12 of 25 patients), 100% (28 of 28 patients), 100% (12 of 12 patients), and 68% (28 of 41 patients) were observed, respectively. According to the status of the patient's symptoms, sensitivity, specificity, positive predictive value, and negative predictive value of MDCTA for the depiction of VA in the emergency room were 78% (7 of 9 patients), 100% (9 of 9 patients), 100% (7 of 7 patients), and 82% (9 of 11 patients), respectively. Sensitivity, specificity, positive predictive value, and negative predictive value of MDCTA in the outpatient clinic were 31% (5 of 16 patients), 100% (19 of 19 patients), 100% (5 of 5 patients), and 63% (19 of 30 patients), respectively (Table 3).
The main findings of the present study include the following: 1) Significant stenosis of the related segment with negative remodeling but no definite evidence of plaque is the characteristic finding on MDCTA of VA. 2) The diagnostic accuracy of the above criteria had high specificity and PPV, but low sensitivity and NPV. 3) When considering the activity of the patient's symptoms, the MDCTA finding of VA had a better diagnostic performance in the emergency room compared to the outpatient clinic.
Vasospastic angina shows a decrease in the luminal diameter in association with clinical symptoms and/or ECG changes on the conventional CAG with an EG test; however, there were no data on imaging findings by MDCTA in the assessment of VA. This report is the first to show significant stenosis with negative arterial remodeling but no definite plaque is a characteristic finding of VA on MDCTA. A prior study using virtual histology-intravascular ultrasound analysis reported that VA patients have less plaque and more negative arterial remodeling compared with unstable angina patients (4); this finding supports our characteristic MDCTA finding. Recently, using intravascular optical coherence tomography, Morikawa et al. (17) also found that coronary artery segments involved in VA are characterized by diffuse intimal thickening without lipid or calcium content. However, another prior study using intravascular ultrasound reported on the frequent presence of non-calcified atherosclerotic lesions at the sites of focal coronary spasm (18). In this study, morphological appearance of involved coronary segments in patients with VA mainly showed no discernable plaque on MDCTA. This discrepancy may be due to the difference in spatial resolution between MDCTA and IVUS or optical coherence tomography.
Coronary vasospasm is transient, often lasting only a few seconds, and is unpredictable. Although the CAG-EG test for VA is usually safe, a number of complications may occur. These include various arrhythmias, hypertension, hypotension, abdominal cramps, nausea, vomiting, and other non-specific complications. In rare cases, serious complications such as ventricular fibrillation, myocardial infarction, or even death may occur (2, 16). Therefore, the tests should be conducted in a setting where appropriate resuscitation and other measures can promptly be performed. Furthermore, the diagnosis of coronary vasospasms must be made on the basis of coronary angiographic findings during the attack. However, it is not possible to perform conventional angiography during the attack in every patient (2). Conversely, MDCTA is frequently used in the evaluation of acute chest pain. In this study, significant stenosis was a prevalent finding without provocation on MDCTA in patients with VA. We speculate that the acquisition of an MDCTA image during an attack is a possible mechanism of significant stenosis without provocation, especially in patients with active VA.
In this study, cardiac MDCTA showed low sensitivity and NPV in the assessment of VA, but good diagnostic accuracy with high specificity and PPV was revealed. In addition, we demonstrated that the diagnostic accuracy of MDCTA in the emergency room was much higher than that of the outpatient setting. On the basis of a good diagnostic accuracy by MDCTA in this study, we suggest that cardiac MDCTA might be helpful in the differentiation of the cause of acute chest pain, especially in the emergency room. Furthermore, the possibility of VA should be considered in patients with acute chest pain if characteristic findings of VA on cardiac MDCTA will be shown. We speculate that a positive MDCTA finding can support clinical diagnosis and lower the frequency of further evaluation gestures.
A number of limitations are present in this study. First, bias cofactors such as the use of a vasodilator, time gap between symptom onset and MDCTA exam, vasoactive medication history before a MDCTA exam, and symptom status at the moment of MDCTA scanning, are potential limitations to the overall results. Because we could not normalize these bias factors, the results should be underestimated compared to reality. Second, this study is a retrospective, single center study in a relatively limited number of subjects. Therefore, further study will be needed with large clinical trials in a prospective manner. Finally, for the diagnostic accuracy of the reference standard in this study, consideration should be given to daily, monthly and yearly as well as circadian variations in the attack of coronary spasm and the sensitivity of the CAG-EG test depends on the disease activity of the time. Therefore, even though the CAG-EG test was used as gold standard in this study, a false negative CAG-EG test may often be obtained in patients with established coronary spasms when the disease activity is low (2).
In conclusion, we suggest that significant stenosis with negative remodeling but no definite evidence of plaque is the characteristic finding on a MDCTA of VA. Cardiac MDCTA shows good diagnostic performance with high specificity and PPV, but low sensitivity and NPV in the assessment of VA. We suggest that positive MDCTA findings may decrease the prevalence of CAG with EG test.
Figures and Tables
Fig. 1
41-year-old man with acute chest pain.
Significant discrete stenosis is noted in middle segment of left anterior descending artery (arrows) on volume rendering image (A), short-axis multiplanar image (B), and curved multiplanar multidetector CT coronary angiography images (C). However, there is no discernable atheroma in related segment, suggesting coronary spasm (B). Mild luminal irregularity is shown at corresponding segment of left anterior descending artery (arrow) on invasive coronary angiography (D). However, provoked tight stenosis occurs at same site (arrow) on invasive coronary angiography after intracoronary administration of ergonovine (E).

Fig. 2
55-year-old woman with acute chest pain.
Curved multiplanar multidetector CT coronary angiography image (A) demonstrating significant discrete stenosis with internal low attenuated area at middle segment of right coronary artery (arrow). Insignificant stenosis is shown at corresponding segment (arrow) on invasive coronary angiography (B). Provoked severe stenosis is revealed at same site (arrow) on invasive coronary angiography after intracoronary administration of ergonovine (C).

References
1. Prinzmetal M, Kennamer R, Merliss R, Wada T, Bor N. Angina pectoris. I. A variant form of angina pectoris; preliminary report. Am J Med. 1959. 27:375–388.
2. Yasue H, Nakagawa H, Itoh T, Harada E, Mizuno Y. Coronary artery spasm--clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 2008. 51:2–17.
3. Hong MK, Park SW, Lee CW, Ko JY, Kang DH, Song JK, et al. Intravascular ultrasound findings of negative arterial remodeling at sites of focal coronary spasm in patients with vasospastic angina. Am Heart J. 2000. 140:395–401.
4. Hong YJ, Jeong MH, Choi YH, Ma EH, Ko JS, Lee MG, et al. Plaque components at coronary sites with focal spasm in patients with variant angina: virtual histology-intravascular ultrasound analysis. Int J Cardiol. 2010. 144:367–372.
5. Mollet NR, Cademartiri F, Nieman K, Saia F, Lemos PA, McFadden EP, et al. Multislice spiral computed tomography coronary angiography in patients with stable angina pectoris. J Am Coll Cardiol. 2004. 43:2265–2270.
6. Nieman K, Cademartiri F, Lemos PA, Raaijmakers R, Pattynama PM, de Feyter PJ. Reliable noninvasive coronary angiography with fast submillimeter multislice spiral computed tomography. Circulation. 2002. 106:2051–2054.
7. Ropers D, Baum U, Pohle K, Anders K, Ulzheimer S, Ohnesorge B, et al. Detection of coronary artery stenoses with thinslice multi-detector row spiral computed tomography and multiplanar reconstruction. Circulation. 2003. 107:664–666.
8. Achenbach S, Giesler T, Ropers D, Ulzheimer S, Anders K, Wenkel E, et al. Comparison of image quality in contrastenhanced coronary-artery visualization by electron beam tomography and retrospectively electrocardiogram-gated multislice spiral computed tomography. Invest Radiol. 2003. 38:119–128.
9. Achenbach S, Moselewski F, Ropers D, Ferencik M, Hoffmann U, MacNeill B, et al. Detection of calcified and noncalcified coronary atherosclerotic plaque by contrast-enhanced, submillimeter multidetector spiral computed tomography: a segment-based comparison with intravascular ultrasound. Circulation. 2004. 109:14–17.
10. Leber AW, Knez A, Becker A, Becker C, von Ziegler F, Nikolaou K, et al. Accuracy of multidetector spiral computed tomography in identifying and differentiating the composition of coronary atherosclerotic plaques: a comparative study with intracoronary ultrasound. J Am Coll Cardiol. 2004. 43:1241–1247.
11. Dorgelo J, Willems TP, Geluk CA, van Ooijen PM, Zijlstra F, Oudkerk M. Multidetector computed tomography-guided treatment strategy in patients with non-ST elevation acute coronary syndromes: a pilot study. Eur Radiol. 2005. 15:708–713.
12. Ghersin E, Litmanovich D, Dragu R, Rispler S, Lessick J, Ofer A, et al. 16-MDCT coronary angiography versus invasive coronary angiography in acute chest pain syndrome: a blinded prospective study. AJR Am J Roentgenol. 2006. 186:177–184.
13. White CS, Kuo D, Kelemen M, Jain V, Musk A, Zaidi E, et al. Chest pain evaluation in the emergency department: can MDCT provide a comprehensive evaluation? AJR Am J Roentgenol. 2005. 185:533–540.
14. Leber AW, Knez A, White CW, Becker A, von Ziegler F, Muehling O, et al. Composition of coronary atherosclerotic plaques in patients with acute myocardial infarction and stable angina pectoris determined by contrast-enhanced multislice computed tomography. Am J Cardiol. 2003. 91:714–718.
15. von Erffa J, Ropers D, Pflederer T, Schmid M, Marwan M, Daniel WG, et al. Differentiation of total occlusion and high-grade stenosis in coronary CT angiography. Eur Radiol. 2008. 18:2770–2775.
16. Hackett D, Larkin S, Chierchia S, Davies G, Kaski JC, Maseri A. Induction of coronary artery spasm by a direct local action of ergonovine. Circulation. 1987. 75:577–582.
17. Morikawa Y, Uemura S, Ishigami K, Soeda T, Okayama S, Takemoto Y, et al. Morphological features of coronary arteries in patients with coronary spastic angina: assessment with intracoronary optical coherence tomography. Int J Cardiol. 2011. 146:334–340.
18. Saito S, Yamagishi M, Takayama T, Chiku M, Koyama J, Ito K, et al. Plaque morphology at coronary sites with focal spasm in variant angina: study using intravascular ultrasound. Circ J. 2003. 67:1041–1045.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download