Abstract
Objective
Imaging methods that use ionizing radiation have been more frequent in various medical fields with advances in imaging technology. The aim of our study was to make residents be aware of the radiation dose they are subjected to when they conduct radiological imaging methods, and of cancer risk.
Materials and Methods
A total of 364 residents participated in this descriptive study which was conducted during the period between October, 2008 and January, 2009. The questionnaires were completed under strict control on a one-to-one basis from each department. A χ2-test was used for the evaluation of data obtained.
Results
Only 7% of residents correctly answered to the question about the ionizing radiation dose of a posteroanterior (PA) chest X-ray. The question asking about the equivalent number of PA chest X-rays to the ionizing dose of a brain CT was answered correctly by 24% of residents; the same question regarding abdominal CT was answered correctly by 16% of residents, thorax CT by 16%, thyroid scintigraphy by 15%, intravenous pyelography by 9%, and lumbar spine radiography by 2%. The risk of developing a cancer throughout lifetime by a brain and abdominal CT were 33% and 28%, respectively.
Medical applications form the majority of the artificial radiation sources that the human beings are being exposed to (1-3), with radiological imaging procedures leading the way (3). X-rays are used in radiography, fluoroscopy, angiography, and computed tomography (CT) (1) and the dose depends on patient factors (age and size), technical factors (equipment settings and procedure length), and equipment model (4).
In recent years, faster and higher resolution studies with dynamic contrast, like the CT angiography, cardiac CT, and virtual CT colonoscopy have become available in parallel to the development of high technology devices like the multidetector CT (5). This has lead to a crescendo in the demands for radiological studies for clinicians in an effort to redesign their diagnostic approaches and treatment plans, which has also given rise to an increase in the exposure of patients to ionizing radiation (1, 2, 6, 7). In England, CT formed 4% of the radiological applications in 1990, compared to USA for which CT made up 10% of the radiological applications in 2000. However, these procedures were found to be responsible for the large majority of ionizing radiation exposure to patients (40% in England; 65% in the USA) (3).
The increasing amount of ionizing radiation that is received from controllable artificial radiation resources gives rise to possible risks of developing cancer over the course of a lifetime and hence constitutes a threat to public health (6, 8, 9). Studies performed during recent years have attempted to drive attention to the potential risks and awareness of physicians to the doses of radiation exposure during the radiological studies used for medical purposes (10-18).
As candidates become specialists, residents are included in this study due to the fact that they often make use of radiological imaging techniques during their training periods and their future professional lives so that they can contribute to the process of diagnosis and treatment. This study aims to illustrate the residents' awareness of ionizing radiation doses and the associated cancer risks to which the patients are exposed to due to radiological imaging techniques.
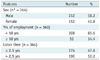
This descriptive study was conducted at the 19 Mayıs University Faculty of Medicine Hospital between October 17th, 2008 and January 12th, 2009. In total, 364 of the 376 (96.8%) residents employed in 26 clinical departments were included in this study. The questionnaires (Table 1) have been completed in the wards and the outpatient wards under strict control on a one to one basis for each department.
In this study, the answers provided to the questions corresponded to the radiation doses received by patients during diagnostic radiological imaging procedures relative to the number of Posteroanterior (PA) chest X-rays evaluated according to the latest data accepted by the European Commission (19).
The questionnaire consisted of easily answered questions about the ionizing radiation doses that the patients are being exposed to during the frequently ordered radiological imaging procedures in terms of the equivalent numbers of one PA chest X-rays. When a PA chest X-ray was compared, radiation doses of 300 times more for the abdominal and thoracic CTs, a dose interval of 50-200 times more for a brain CT, lumbar spine radiography, and thyroid scintigraphy, and ultrasonography (US) and magnetic resonance imaging (MRI) would not emit ionizing radiation, were accepted to be correct (19). Based on the data published in the bulletin of radiological protection, number 231 of National Radiological Protection Board in 2001, the contribution of a brain CT study to cancer development throughout a lifetime has been accepted to be between 1/10000-1/100000 and the contribution of an abdominal CT study have been accepted to be between 1/1000-1/10000 (20).
Statistical analysis was conducted using SPSS version 12 (Chicago, IL, USA). Descriptive statistics were expressed as the median (minimum-maximum). The Chi-Square test was used to determine the factors affecting residents' awareness of the doses that patients are being subjected to during the radiological imaging procedures. Statistical significance was set at p < 0.05.
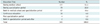
A total of 364 residents participated in this study. The median age of the participants was 29.0 (24.0-41.0) years, while the median employment duration after graduation was 5.0 (0.1-16.0) years. The median employment duration as a resident was found to be 3.0 (0.1-7.0) years. The sociodemographic features of the study group are provided in Table 2.
It has been found out that 147 residents (40.4%) received education about the doses of radiation that patients are being subjected to and their potential hazards, whereas 217 residents (59.6%) did not. Furthermore, 109 (74.1%) from the educated group received this education during medical school years, while 31 (21.1%) were educated during the specialization period, and 7 (4.8%) were educated both during medical school and the specialization period.
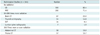
The question which stated "Should education be given on this topic?" was answered affirmatively by 345 (94.8%) and negatively by 19 (5.2%) of the participants. Table 3 demonstrates the wishes of the residents about the timing of the intended education.
Residents (n = 338) stated that they made their preferences in accordance with the algorithm (59.8%), availability (6.8%), convenience with diagnosis (4.4%), availability and algorithm (4.4%), cost and algorithm (3.6%), and radiation content (2.4%). In addition, 18.6% of the residents have marked more than one choice. Residents of the Radiology Department did not answer this question as they do not order these studies themselves and one of the residents in another clinical branch did answer this question.
The residents were asked to answer the question denoting the radiation dose that the patients are being subjected to during the shooting of a PA chest X-ray and 26 (7.2%) out of 359 chose the correct option of 0.02 millisieverts (mSv), while 52 (14.5%) chose 0.2 mSv, 24 (6.7%) chose 2 mSv, 16 (4.5%) chose 20 mSv and 241 (67.1%) chose the option denoting "I have no idea".
The most commonly ordered imaging methods of the residents (n = 331) were brain CT (36.9%), thorax CT (21.8%) and abdominal CT (12.7%). The residents of the Radiology and Nuclear Medicine Departments did not answer this question as they do not order CT studies for patients.
For the question about whether information is given to patients who are scheduled for a CT about the dose of radiation that they will be subjected to and its potential risks, 291 (81.8%) of the 356 participants replied that they did not inform the patients, 40 (11.2%) replied as they did and 25 (7.0%) replied as "sometimes".
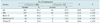
Table 4 presents the distribution of the correct answers of the residents given to the question asking the corresponding number of PA chest X-rays in terms of received radiation doses during radiological studies.
Some of the residents stated that US (5.8%) and MRI (14.8%) involved radiation whereas some of them did not have an idea about whether or not US (11.8%) and MRI (13.8%) inhibited radiation.
When years of employment was taken into consideration for the comparison of the correct answers concerning the equivalent number for one PA chest X-ray in terms of received radiation doses during the frequently ordered radiological studies; the difference between the correct answers given to brain CT, abdominal CT and thorax CT were not statistically significant (p > 0.05), while the frequency of the correct answers in the group which were employed for more than 10 years was observed to be less and was statistically significant in terms of the correct answers given for US and MRI (p < 0.05) (Table 5).
The correct answers given by the residents about radiation doses that patients are being exposed to and the possible risks of cancer, whether educated or not about the imaging studies that use ionizing radiation, did not reach to statistical significance (p > 0.05).
In total, 120 (33%) of the residents have given the correct answer, which was 1/10000 to 1/100000, to the question denoting the risk of developing cancer throughout a lifetime with a brain CT, whereas incorrect answers included 101 (27.7%) for "200000-500000", 76 (20.9%) for "1000-5000", 38 (10.4%) for "no risk at all" and 29 (8.0%) for "I have no idea".
The risk of developing cancer throughout a lifetime as a result of radiation exposure from an abdominal CT was answered correctly as 1000-10000 by 100 (27.5%) of the residents, while 119 (32.7%) replied "50000-100000", 81 (22.2%) replied "20000-50000" 33 (9.1%) replied as "I have no idea" and 31 (8.5%) replied as "there were no risks".
The additional question that was posed to residents in the radiology department, being the executors of the tests, about whether there were any differences in the study modalities between the adults and children during a CT imaging was answered correctly by (n = 25) 24 (96%) of the residents, while 1 (4%) did not provide an answer. The question about the approximate difference in percents between the effective dose that the patient would have been exposed to when, for a given area of CT investigation, a pediatric dose adjusted optimal image quality was to be compared with an adolescent CT study was answered correctly as 50% by 5 (21.7%) out of 23 (92.0) residents, while 18 (78.3%) gave an incorrect answer.
Exposure to ionizing radiation as a result of a radiologic examination is associated with the risk of induction of malignancy. For comparison of radiation exposure levels from different sources, the concept of effective dose equivalent was developed, and used to assess an individual's risk of developing malignancy. Effective dose equivalents range from 0.06 to 0.25 mSv with a chest radiography in 2 views, 3-27 mSv with CT using conventional examination parameters, and 0.3-0.55 mSv using low dose CT settings. Based on considerations by the International Commission on Radiological Protection, it can be expected that radiation exposure with an effective dose equivalent of 1 mSv would lead to 5 additional malignancies in 100000 individuals exposed (21).
The use of CT has increased by a factor of 12 in the United Kingdom and a factor of 20 in the USA between the years 1980-2005 (9). In a study conducted by Fazel et al. (22) between the years 2005 and 2007, it has been demonstrated that 665613 out of 952420 patients (68.8%) have undergone a radiological study containing ionizing radiation at least once, and that 1.9 of every 1000 patients receives 50 mSv or more radiation every year and the cumulative effective dose arises mainly from the CT and nuclear imaging studies by 75.4-81.8%.
Studies put forward that the ratio of unnecessary or inappropriate radiological studies performed attained 10-40% (7, 23, 24). The preferences of the residents denoting algorithm and convenience with the diagnosis when ordering radiological imaging methods is meaningful for our study in an effort to lower the radiation dose that the patients will be exposed to. However standardized algorithm schemes should be present for this. Furthermore, 2.4% of the residents who ordered imaging procedures without taking into consideration the radiation emission and 6.8% who would order according to ease of availability may lead to patients being unnecessarily exposed to ionizing radiation.
In our study, the dose of radiation that the patients are being exposed to during the shooting of a PA chest X-ray was answered correctly by 7.2% of residents. In studies by Jacob et al. (10) and Heyer et al. (11) 22.5% and 39.5% of the doctors, respectively, gave correct answers for the dose exposure to patients during the shooting of a PA chest X-ray, whereas a study by Shiralkar et al. (12) found that none of the doctors gave a correct answer to this question.
Furthermore, 81.7% of the residents have answered that they did not inform patients about the radiation dose they would receive from a CT study, nor for the potential risks associated with the radiation exposure. Lee et al. (13) study put forward that 78.0% of the doctors in the emergency service provided no explanation at all to patients before a CT imaging was performed.
The radiation doses for a brain CT, abdominal CT, thorax CT, intravenous pyelography, thyroid scintigraphy and lumbar spine radiography were asked to be matched with the corresponding number of PA chest X-rays in terms of ionizing radiation doses and 23.9%, 15.9%, 15.7%, 9.3%, 14.8% and 1.9% of the residents answered correctly to the question, respectively. An investigation of the literature revealed that the ratio of the correct answers to these questions were as low as we found in this study (10-18).
The frequency of false answers about US and MR radiation content was found to be higher among the doctors whose graduation dates were more than 10 years ago (p < 0.004, p < 0.013). This might stem from the fact that MRI is a relatively newer radiological technique, and in this respect, sufficient training was not provided. The answers about the radiation doses of the radiological examinations and cancer risks showed no statistical difference for the comparison of theeducated and not educated groups being educated or not (p > 0.05). This indicates that the residents do not receive adequate and effective education either during medical school or afterwards. The findings of the study performed by Arslanoğlu et al. (14) are concordant with ours with respect to denoting a higher frequency of false answers for the presence of ionizing radiation in US and MRI among the participants with employment times greater than 10 years (p < 0.05). Further, there was no statistically significant correlation found between the correct answers and the period of employment in Heyer et al. (11) and Gümüş et al. (15) studies. The frequency of the correct answer, "US and MRI does not contain ionizing radiation" in the literature was in the range of 71.6-92% and 89.2-96%, respectively (10, 12, 14, 15, 17).
Recent studies declared that low doses of ionizing radiation is bringing forward an extra risk of developing cancer throughout a lifetime, hence leading to an increase in the number of studies focusing on this subject (2, 7-9, 25-30). Pediatric patients are thought to be affected more from the radiation as they are still in the development period and have lower body mass indexes. Various studies have put forward that although life expectancy is longer in children, the risk of developing cancer is expected to be higher (6, 8, 23, 26, 31-35). An estimated contribution of a CT study that would add to the risk of developing cancer in a 1 year old child due to radiation was estimated to be 0.18% for an abdominal CT and 0.07% for a brain CT according to Brenner et al. (8), which is much higher than the adolescent values.
In this study, the frequency of added risk for developing cancer throughout a lifetime due to a brain CT and an abdominal CT was answered correctly by 33% of the participating residents for brain CT and by 27.5% for abdominal CT. Rice et al. (16) and Gümüş et al. (15) found that the ratio of the doctors who answered correctly to the questions about the contribution to the risk of developing cancer throughout a lifetime as a result of radiation doses from an abdominal CT and a pelvic CT were 31.0% and 15.7%, respectively. In contrast, Lee et al. (13) found that only 47.0% of the radiologists and 9.0% of the emergency clinic doctors have mentioned that a single abdominopelvic CT would have a contribution to developing cancer throughout a lifetime.
Prompt dosage adjustments are indicated to be mandatory during radiological studies, especially when the evaluation method exposes residents to ionizing radiation like the various CT methods (2, 6, 7, 36-40). In the Alara Conference Public Health Declaration, The American Food and Drug Administration have pointed out that the attenuation in the doses resulting from pediatric and adolescent CT applications, the CT application parameters should be optimized and orders for contrast-enhanced multiphasic CT studies should be minimized (41).
For the CT studies ordered by residents, the belief is that the radiation dose that the patients are being exposed to is less than their anticipation. This leads to ordering CT studies that contain more ionizing radiation to be easier as well as higher numbers of unnecessarily ordered procedures. Nevertheless, the presence of residents with the thoughts that US and MRI contains ionizing radiation may have an unfavorable effect on the priorities for directing the patients to these study methods.
As a result, in order to increase the awareness of physicians about the radiological imaging methods that contain ionizing radiation, this subject should be taught during the basic training in medical schools and then updated protocols should adequately and effectively be taught after graduation.
The presence of the easily visible documents within the working offices of the physicians, emphasizing the content of the ionizing radiation over the course of radiological imaging procedures, may be a practical solution when ordering radiological studies.
Figures and Tables
References
1. Tuncel E. Klinik Radyoloji. Genişletilmiş 2. Baskı. 2008. Nobel&Güneş Tıp Kitabevleri;3–105.
2. Nickoloff LE, Alderson PO. Radiation Exposures to Patients from CT: Reality, Public Perception, and Policy. AJR Am J Roentgenol. 2001. 177:285–287.
3. UNSCEAR 2000. UNSCEAR 2000 Report to the General Assembly. Sources and Effects of Ionizing Radiation, United Nations Scientific Committee on the Effects of Atomic Radiation. 2000. New York: United Nations.
4. Brody AS, Frush DP, Huda Walter, Brent RL. Section on Radiology. Radiation risk to children from computed tomography. Pediatrics. 2007. 120:677–682.
5. Flohr TG, Schaller S, Stierstorfer K, Bruder H, Ohnesorge BM, Schoepf UJ. Multi-Detector Row CT Systems and Image-Reconstruction Techniques. Radiology. 2005. 235:756–773.
6. Donnelly LF. Reducing Radiation Dose Associated with Pediatric CT by Decreasing Unnecessary Examinations. AJR Am J Roentgenol. 2005. 184:655–657.
7. Frush PD. Review of Radiation Issues for Computed Tomography. Semin Ultrasound CT MR. 2004. 25:17–24.
8. Brenner DJ, Elliston CD, Hall EJ, Berdon WE. Estimated risks of radiation-XMLLink_XYZnduced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001. 176:289–296.
9. Hall EJ, Brenner DJ. Cancer risks from diagnostic radiology. Br J Radiol. 2008. 81:362–378.
10. Jacob K, Vivian G, Steel JR. X-ray dose training: are we exposed to enought? Clin Radiol. 2004. 59:928–934.
11. Heyer CM, Peters S, Lemburg S, Nicholas V. Awareness of radiation exposure of thoracic CT scans and conventional radiographs: what do non-radiologists know? Rofo. 2007. 179:261–267.
12. Shiralkar S, Rennie A, Snow M, Galland RB, Lewis MH, Gower-Thomas K. Doctors' knowledge of radiation exposure: questionnaire study. BMJ. 2003. 327:371–372.
13. Lee CI, Haims AH, Monico EP, Brink JA, Forman HP. Diagnostic CT scans: assessment of patient, physician, and radiologist awereness of radiation dose and possible risks. Radiology. 2004. 231:393–398.
14. Arslanoğlu A, Bilgin S, Kubalı Z, Ceyhan MN, Ilhan MN, Maral I. Doctors' and intern doctors' knowledge about patients' ionizing radiation exposure doses during common radiological examinations. Diagn Interv Radiol. 2007. 13:53–55.
15. Gümüş C, Cankorkmaz L, Erkoç MF, Öztoprak B, Atalar M, Köylüoğlu G. Turkish pediatric surgeons knowledge on the radiation exposure of patients during diagnostic imaging. Türkiye Klinikleri J Med Sci. 2008. 28:623–627.
16. Rice HE, Frush DP, Harker MJ, Farmer D, Waldhausen JH. Peer assessment of pediatric surgeons for potential risks of radiation exposure from computed tomography scans. J Pediatr Surg. 2007. 42:1157–1164.
17. Soye JA, Paterson A. A survey of radiation dose among healt profesionals in Northern Ireland. Br J Radiol. 2008. 81:725–729.
18. Quinn AD, Taylor CG, Sabharwal T, Sikdar T. Radiation protection awareness in non-radiologists. Br J Radiol. 1997. 70:102–106.
19. European Commission. Final Report to the European Commission for Grant Agreement SUBV99/134996; Luxembourg 2007. Radiation Protection 118 Update Mars 2008 Referral Guidelines For Images.
20. National Radiological Protection Board (NRPB). Radiological Protection Bulletin. 2001. No: 231. Sept 2001 Chilton, Didcot, Oxon OX11 0RQ.
21. Diederich S, Lenzen H. Radiation exposure associated with imaging of the chest: comparison of different radiographic and computed tomography techniques. Cancer. 2000. 89:2457–2460.
22. Fazel R, Krumholz HM, Wang Y, Ross JS, Chen J, Ting HH, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med. 2009. 361:849–857.
23. Slovis TL. The ALARA Concept in Pediatric CT: Myth or Reality? Radiology. 2002. 223:5–6.
24. Cascade PN, Webster EW, Kazerooni EA. Ineffective Use of Radiology: The Hidden Cost. AJR Am J Roentgenol. 1998. 170:561–564.
25. Goske MJ, Applegate KE, Boylan J, Butler PF, Callahan MJ, Coley BD, et al. The 'Image Genty' campaign: increasing CT radiation dose awarenes throught a national education and awareness program. Pediatr Radiol. 2008. 38:265–269.
26. Huda W, Vance A. Patient radiation doses from adult and pediatric CT. AJR Am J Roentgenol. 2007. 188:540–546.
27. Lee CI, Flaster HV, Haims AH, Monico EP, Forman HP. Diagnostic CT Scans: Institutional Informed Consent Guidelines and Practices at Academic Medical Centers. AJR Am J Roentgenol. 2006. 187:282–287.
28. De Jong PA, Mayo JR, Golmohammadi K, Nakano Y, Lequin MH, Tiddens HA, et al. Estimation of Cancer Mortality Associated with Repetitive Computed Tomography Scanning. Am J Respir Crit Care Med. 2006. 173:199–203.
29. Rogers LF. Radiation Exposure in CT: Why So High? AJR Am J Roentgenol. 2001. 177:277.
30. Brenner DJ. Radiation Risks Potentially Associated with Low-Dose CT Screening of Adult Smokers for Lung Cancer. Radiology. 2004. 231:440–445.
31. Rice HE, Frush DP, Farmer D, Wadhausen JH. Review of radiation risks from computed tomography: essentials for the pediatric surgeon. J Pediatr Surg. 2007. 42:603–607.
32. Frush DP, Donnely LF, Rosen NS. Computed tomography and radiation risks: What pediatric health care providers should know. Pediatrics. 2003. 112:951–957.
33. Sadetzki S. Excess lifetime cancer mortality risk attributed to radiation exposure from pediatric computed tomography scan. IMAJ. 2007. 9:607–609.
34. Linton OW, Mettler FA. National conference on dose reduction in CT, with an emphasis on pediatric patients. AJR Am J Roentgenol. 2003. 181:321–329.
35. Pettersson HB, Falth-Magnusson K, Persliden J, Scott M. Radiation risk and cost-benefit analysis of a paediatric radiology procedure: results from a national study. Br J Radiol. 2005. 78:34–38.
36. Kalra MK, Maher MM, Toth TL, Hamberg LM, Blake MA, Shepard JA, et al. Strategies for CT radiation dose optimization. Radiology. 2004. 230:619–628.
37. Prasad SR, Wittram C, Shepard JA, McLoud T, Rhea J. Standard- dose and 50%-reduced-dose chest CT: Comparing the effect on image quality. AJR Am J Roentgenol. 2002. 179:461–465.
38. Livingstone RS, Eapen A, Dip NB, Hubert N. Achieving reduced radiation doses for CT examination of the brain using optimal exposure parameters. Ind J Radiol Ima. 2006. 16:247–251.
39. Park EA, Lee W, Kang JH, Yin YH, Chung JW, Park JH. The image quality and radiation dose of 100-kVp versus 120-kVp ECG-gated 16 slice CT coronary angiography. Korean J Radiol. 2009. 10:235–243.
40. Qi W, Li J, Du X. Method for automatic tube current selection for obtaining a consistent image quality and dose optimization in a cardiac multidetector CT. Korean J Radiol. 2009. 10:568–574.
41. FDA Public Health Notification: Reducing radiation risk from computed tomography for pediatric and small adult patients. Pediatr Radiol. 2002. 32:314–316.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download