Abstract
Objective
We wanted to evaluate the image quality, diagnostic accuracy and radiation exposure of 64-slice dual-source CT (DSCT) coronary angiography according to the heart rate in symptomatic patients during daily clinical practice.
Materials and Methods
We performed a retrospective search for the DSCT coronary angiography reports of 729 consecutive symptomatic patients. For the 131 patients who underwent invasive coronary angiography, the image quality, the diagnostic performance (sensitivity, specificity, positive predictive value [PPV] and negative predictive value [NPV] for detecting significant stenosis ≥ 50% diameter) and the radiation exposure were evaluated. These values were compared between the groups with differing heart rates (HR): mean HR < 65 or ≥ 65 and HR variability (HRV) < 15 or ≥ 15.
Results
Among the 729 patients, the CT reports showed no stenosis or insignificant coronary artery stenosis in 72%, significant stenosis in 26% and non-diagnostic in 2%. For the 131 patients who underwent invasive coronary angiography, 95% of the patients and 97% of the segments were evaluable, and the overall per-patient/per-segment sensitivity, the perpatient/per-segment specificity, the per-patient/per-segment PPV and the per-patient/per-segment NPV were 100%/90%, 71%/98%, 95%/88% and 100%/97%, respectively. The image quality was better in the HR < 65 group than in the HR ≥ 65 group (p = 0.001), but there was no difference in diagnostic performance between the two groups. The mean effective radiation doses were lower in the HR < 65 or HRV < 15 group (p < 0.0001): 5.5 versus 6.7 mSv for the mean HR groups and 5.3 versus 9.3 mSv for the HRV groups.
The recent 64-slice dual-source computed tomography (DSCT) scanners are equipped with two tubes and corresponding detectors in a 90° geometry, and this provides a heart-rate-independent temporal resolution of 83 msec. Such improved temporal resolution allows for great improvement in the image quality of noninvasive CT coronary angiography (1-18). The diagnostic accuracy of 64-slice DSCT for the detection of coronary artery stenosis has also improved and even in patients with a high heart rate, as compared to that of 16-slice or 64-slice CT (1, 9, 10). Yet in clinical practice, perception errors due to fatigue can develop more often than in controlled studies in which the readers examine the images under ideal conditions. In addition, it is still unknown whether the diagnostic performance of 64-slice DSCT for detecting coronary artery stenosis can be reproduced in daily clinical settings.
With the advances in temporal resolution of 64-slice DSCT, a narrow range of ECG pulsing and heart-rate adaptive pitch are now available for clinical practice and this has resulted in a great reduction of the dose of radiation exposure (16, 19-21). DSCT also allows for more powerful ECG pulsing by limiting the minimum tube current to 4% of the maximum current level (MinDose, Siemens Healthcare, Forchheim, Germany), while the minimum level of tube current is defined as 20% for 16- and 64-slice MDCT scanners (20).
In this study, we evaluated whether the high diagnostic performance, good image quality and decrease in radiation exposure of 64-slice DSCT coronary angiography can be reproduced in the daily clinical setting in symptomatic patients. We also wanted to evaluate the effect of heart rate on the diagnostic accuracy, image quality and radiation exposure.
The Institutional Review Board of our hospital approved this retrospective study and the requirement for informed consent was waived.
From June 2008 to November 2008, 729 consecutive symptomatic patients suspected of or with known coronary artery disease (M:F = 366:363; mean age, 60.5 years ± 11.0; age range, 23-89 years) underwent 64-slice DSCT coronary angiography in our hospital: those patients with Kawasaki disease, previous coronary artery bypass surgery or percutaneous coronary intervention, and those patients without any cardiac symptoms were excluded. Among the 729 patients, 131 patients (M:F = 85:46; mean age, 64.5 years ± 8.9; age range, 38-83 years) had undergone invasive coronary artery angiography with a mean time interval between DSCT and invasive coronary angiography of 26.4 ± 23.7 days (range: 0-122 days).
All the CT examinations were performed using a dual-source scanner (Somatom Definition; Siemens Medical Solutions, Forchheim, Germany). Among the 729 enrolled patients, 588 patients with a prescanning heart rate of 65 beats per minute (bpm) or higher were given 50-100 mg of oral metoprolol (Betaloc; AstraZeneca, Sweden) 45-60 min prior to the CT examination unless the subject had a contraindication to beta-blockers: 50 mg of beta-blocker in 184 patients with a prescanning heart rate of 65 to 69 bpm, and 100 mg in 404 patients with a prescanning heart rate of 70 bpm or higher. However, additional beta-blockers were not given to any patients who underwent CT scanning 45-60 min after administration of the first dose of betablocker, and even if the heart rate did not decrease below 65 bpm. Among the 131 patients who underwent invasive coronary angiography, 102 patients took beta-blockers.
Precontrast scanning for calcium scoring was performed using a prospective ECG-gating protocol with 80% of the R-R interval (3-mm section thickness and collimation, 120 kVp, tube current-time: 100 mAs, collimation: 32 × 0.6 mm, section acquisition: 64 × 0.6 mm with the z-flying focal spot technique, gantry rotation time: 330 msec, pitch: 0.2-0.5, depending on the heart rate).
Sublingual nitroglycerin (0.6 mg) (Nitroquick; Ethex, St. Louis, MO) was administered for coronary vasodilation after completion of the calcium scoring scanning in all patients, except nineteen who had a contraindication to nitroglycerin. Sixty mL of a nonionic contrast medium (Ultravist 370; Bayer Schering Pharma, Berlin, Germany) was injected into an antecubital vein at 5 mL/sec, followed by additional 20 mL of a nonionic contrast medium and 50 mL of an 8:2 mixture of normal saline and contrast medium and both at a flow rate of 4 mL/sec with the use of a dual power injector (Stellant; Medrad, Indianola, PA). The bolus triggering method was used to determine the beginning of CT acquisition by monitoring the signal density of the contrast medium in the mid ascending aorta. CT scans were started 8 seconds after a threshold trigger of 150 HU above the baseline was reached. In general, cardiac CT scans were performed using the retrospective ECG-gated mode with ECG pulsing. The ECG-pulsing window for radiation dose reduction was applied: 65-75% of the R-R interval in patients with ≤ 65 bpm and 25-80% for the patients with > 65 bpm. Outside the ECG-pulsing window, the tube current was reduced to 4% of the full current (Mindose; Siemens Healthcare). The pitch was automatically adapted to the heart rate: 0.20 (40 bpm), 0.26 (60 bpm), 0.32 (70 bpm), 0.37 (80 bpm), 0.43 (90 bpm) and 0.50 (100 bpm). The scanning parameters used in our study were as follows: a detector collimation of 32 × 0.6 mm, a section collimation of 64 × 0.6 mm with a z-flying focal spot, a gantry rotation time of 330 msec, a tube voltage of 100 or 120 kVp, and a maximum tube current of 320 mAs per rotation. Scans were usually performed from the diaphragm to the level of the tracheal bifurcation in the caudocranial direction. The mean heart rate and range of the heart rate during CT scanning were recorded for all the patients.
Standard reconstruction algorithms were applied using the absolute reverse or percentage technique to obtain data sets during end systole and/or mid- to end diastole according to the heart rate. In the cases for which the standard reconstruction algorithm provided data sets with insufficient image quality of one or more coronary segments, additional data sets were manually reconstructed. If necessary, multiple data sets of a single patient were used separately to obtain optimal image quality for all the coronary segments. Image reconstruction windows were manually repositioned to achieve high image quality for the patients with arrhythmia, as was previously described (8).
The parameters used for image reconstruction for DSCT coronary angiography included a slice thickness of 0.6 mm, increments of 0.4 mm and a kernel value of B26f. The parameters used for image reconstruction for calcium scoring included a slice width of 3 mm and a kernel of B35f. The DSCT data sets were transferred to an offline workstation (Wizard, Siemens Medical Solutions Software, Germany) with cardiac post-processing three-dimensional software (Rapidia; INFINITT, Seoul, Korea). In addition to the axial images and the oblique multiplanar reconstructions (MPR), the curved MPRs (CMPRs), maximum intensity projections (MIPs) and three-dimensional volume rendering technique (VRT) reconstructions were created for the visualization and analysis of the data.
In the first session, one observer classified a total of 729 patients into four categories through a database of radiologic reports made by one radiologist: (a) patients with neither calcium nor stenosis, (b) patients with insignificant stenosis, (c) patients with indeterminate stenosis and (d) patients with significant stenosis. Lesions with a stenosis of 50% or greater in diameter were considered to be significant. Indeterminate stenosis was defined when a lesion was unevaluable due to artifacts or adjacent calcification. If a patient had a coronary artery segment with significant stenosis and another coronary artery segment was indeterminate at the same time, then he/she was classified as a patient with significant stenosis. On the other hand, if a patient had one coronary artery segment with insignificant stenosis and another coronary artery segment was indeterminate, then he/she was classified as a patient with indeterminate stenosis. As routine practice, the CT data were processed using three-dimensional software (Rapidia; INFINITT, Seoul, Korea) and the CT images were interactively assessed by one experienced radiologist (with 4 years of experience in cardiovascular imaging). The contrast-enhanced dual-source CT was evaluated using 0.6 mm thick-transverse axial images, MIP, CMPR and three-dimensional VRT.
By reviewing the electronic medical records, the results of the treadmill test or myocardial single photon emission CT (SPECT) were also recorded when this was performed within one month of before or after DSCT coronary angiography. Myocardial perfusion was evaluated using dual isotopes of rest thallium SPECT (Tl-SPECT) and stress 99mTc sestamibi SPECT. The observer also checked whether patients had undergone invasive coronary artery angiography and the observer also recorded its results: lesions with a stenosis of 50% or greater in diameter were considered to be significant.
In the second session, one observer selected 131 patients who underwent further invasive coronary angiography within three months of after DSCT coronary angiography, and he recorded the presence of significant stenosis of the coronary arteries based on a modified model of the coronary tree with 15 segments (22) through a database of radiologic reports made by one radiologist: for the right coronary artery, segment 1 was considered proximal, segment 2 was considered middle, segment 3 was considered distal, segment 4 was considered the posterior descending segment and segment 5 was considered the posterolateral branches. Segment 6 was considered the left main stem artery. For the left anterior descending artery, segment 7 was considered proximal, segment 8 was considered middle, segment 9 was considered distal, segment 10 was considered the first diagonal and segment 11 was considered the second diagonal. For the left circumflex artery, 12 was considered proximal, 13 was considered distal, 14 was considered the first obtuse marginal branch and 15 was considered the second obtuse marginal branch. In routine practice, the stenoses were visually evaluated and described as the percentage of lumen diameter reduction. The observer classified each segment as significant (≥ 50% lumen diameter reduction) or nonsignificant (< 50% lumen diameter reduction) based on the radiologic reports. All the coronary artery segments with a diameter of 1 mm or larger were included.
In the third session, two readers working in consensus retrospectively evaluated the overall image quality of the CT images of 131 patients in terms of the degree of coronary or respiratory motion artifact, beam hardening artifacts due to coronary calcification, coronary artery enhancement and quantum noise on a 4-point scale as excellent: 1, good: 2, fair: 3 or poor: 4 (10).
The conventional coronary angiography was performed by three experienced cardiologists according to the standard procedure of using the transfemoral or transradial Judkins technique at our hospital. To visualize the right coronary artery, at least two projections were obtained; for the left coronary artery, at least six projections were obtained. The severity of stenosis was retrospectively evaluated, using quantitative coronary analysis (QCA, version 3.3; Philips, Eindhoven, the Netherlands), by a single observer who was blinded to the CT results. Segmental disease was analyzed in each vessel by using the same 15-segment model that was employed for the dual-source CT analysis. The severity of stenosis was classified on the projection according to the maximal luminal diameter stenosis. Lesions with a stenosis of 50% or greater in diameter were considered to be significant.
All conflicting results between the two modalities were retrospectively analyzed by two observers, and the results were investigated for the reasons for disagreement. The causes of the unevaluable segments were also evaluated. In the case of discordance between DSCT and coronary angiography in defining the coronary artery segment according to the American Heart Association classification, disagreement was resolved via a consensus reading (23).
One observer evaluated whether the optimal ECG pulsing and pitch were used according to the heart rates, whether the scan range covered only the heart or the entire thorax, as well as which tube voltage was used in the 729 CT examinations. Four hundred thirty CT examinations were selected in order to assess the effect of heart rate on the radiation dose in the dedicated routine cardiac CT protocol covering only the heart. The volume CT dose index (CTDIvol) and the dose length product (DLP), which were provided by the scanner system, were recorded. The effective dose was derived from the DLP and a conversion coefficient for the chest as the investigated anatomic region. This conversion coefficient (k = 0.017 mSv × mGy-1 × cm-1) was averaged between the male and female models.
The diagnostic performance of CT coronary angiography for making the diagnosis of significant coronary artery disease as compared with the standard of reference and the quantitative coronary angiography on conventional coronary angiography was determined by measuring the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy. The image quality and radiation dose according to the heart rate frequency and heart rate variability were compared using the Student t-test. We used 65 bpm as the cut-off value for the high heart rate group (9) and the mean heart rate difference of 15 bpm as the cut-off value for the high heart rate variability group (10).
All the statistical analyses were performed with statistical packages (SPSS for Windows, version 12.0, SPSS, Chicago, IL; GraphPad Prism, version 3.02, GraphPad Software, San Diego, CA). Differences were considered significant for p values less than 0.05.
Of the 729 patients, 301 (41%) patients had neither coronary artery calcium nor stenosis seen on CT, and 225 (31%) patients showed insignificant coronary artery stenosis on CT. DSCT coronary angiography showed a low rate of non-diagnostic cases (16 [2%] of 729 patients), and definite significant stenosis of the coronary arteries on CT was reported in 187 (26%) patients. Among the 182 patients with significant stenosis seen on CT, single-vessel disease was reported in 97 (52%) patients, two-vessel disease was reported in 52 (28%) patients and three-vessel disease was reported in 39 (21%) patients.
Of the 16 patients with indeterminate stenosis, dense calcification was the most common cause (n = 10), followed by coronary motion artifacts (n = 4) and respiratory motion artifacts (n = 2). Seven of the 16 patients with indeterminate stenosis on CT underwent further invasive coronary angiography, from which five patients showed significant coronary artery stenosis.
Figure 1 showed the clinical practice in our institution for the 729 symptomatic patients who underwent DSCT coronary angiography. Among 526 patients who showed normal or insignificant coronary stenosis on CT, 15 patients underwent invasive coronary angiography despite of negative results on CT because coronary artery disease was still clinically suspected. All 15 patients showed negative results after invasive coronary angiography. For the treadmill test or SPECT, the false positives and false negatives were substantial. Fourteen (37%) of 38 tests were positive for the patients with normal coronary CT angiography. For the indeterminate cases on CT, all four negative cases on the treadmill test or SPECT turned out to be positive after invasive coronary angiography. For the seven cases with significant stenosis seen on invasive coronary angiography, the treadmill test or SPECT showed negative results.
Invasive coronary angiography revealed 300 (15%) significant stenoses of 1987 segments in 108 (82%) of 131 patients. Single-vessel disease was present in 50 (46%) patients, two-vessel disease was present in 25 (23%) patients and three-vessel disease was present in 33 (31%) patients.
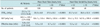
Table 1 summarizes the diagnostic performance of DSCT coronary angiography. Of the 131 patients, 124 (95%) patients were classified as evaluable. On the per-patient analysis, the sensitivity, specificity, PPV and NPV were 100%, 71%, 95% and 100%, respectively. The overall accuracy between invasive coronary angiography and DSCT on a per-patient basis was 95%.
Of the 1987 segments, 1935 (97%) segments were classified as evaluable. On the per-segment analysis, the sensitivity, specificity, PPV and NPV were 90%, 98%, 88% and 97%, respectively. The overall accuracy between invasive coronary angiography and DSCT on a per-segment basis was 97%.
Unevaluable segments on CT were present in 52 segments. There were no significant differences between any subset of the two groups according to the heart rate or the heart rate variability. On invasive angiography, 28 (54%) segments showed significant stenosis.
Diagnostic image quality was found in 128 (98%) of 131 patients: diagnostic image quality was found in 101 (99%) of the 102 patients with a heart rate less than 65 bpm versus in 27 (93%) of the 29 patients with a heart rate of 65 bpm or more (p = 0.123); diagnostic image quality was found in 115 of the 116 (99%) patients with heart rate variability less than 15 bpm versus in 13 (87%) of the 15 patients with a heart rate variability of 15 bpm or more (p = 0.035). The mean scores of image quality were significantly better for the patients with a heart rate less than 65 bpm as compared to those scores for the patients with a heart rate of 65 bpm or more (p = 0.001). The mean scores of image quality for the patients with a heart rate variability less than 15 bpm showed a tendency to be better than those scores for the patients were a heart rate variability of 15 bpm or more, but this did not reach statistical significance (p = 0.395) (Table 1).
A total of 63 segments showed discrepancy between DSCT and invasive coronary angiography for the detection of coronary artery stenosis of 50% or greater in diameter. Thirty five false-positive segments and 28 false-negative segments were detected on CT.
The causes of false-positive segments were dense calcification in 16 (46%) segments, coronary motion in 10 (29%), stair-step artifact in two (6%) and disagreement in seven (20%) (Fig. 2).
The causes of the false-negative segments were subclassified into two categories: detection failure in 18 (64%) segments and underestimation of the degree of stenosis in 10 (36%) segments. Detection failure occurred due to a small branch in seven segments (39%), perception error in six (33%), calcification in two (11%), motion artifact in two (11%) and poor enhancement in one (6%) (Fig. 3). The causes of underestimation of stenosis were calcification in six segments (60%), small branch in one (10%), motion artifact in one (10%) and perception error in two (20%). A small branch, calcification and perception error were shown to be the major causes of the overall false-negative segments.
Of the 52 unevaluable segments detected on CT, the main causes of non-diagnostic segments were dense calcification in 37 (71%) segments, wall blurring due to coronary motion in seven (14%), poor enhancement in seven (14%), stair-step artifact in one (2%) and a small branch in one (2%).
Table 2 demonstrated radiation dose exposure according to the mean heart rate and heart rate variability. The mean CTDIvol and effective dose were 23.3 mGy and 5.8 mSv, respectively. The mean values of the estimated radiation dose during CT scans were significantly greater in the patients with a higher heart rate or higher heart rate variability (p < 0.0001).
This study was conducted to retrospectively evaluate the diagnostic accuracy of 64-slice DSCT coronary angiography in daily clinical practice for patients with suspected coronary artery disease and with using invasive coronary artery angiography as the standard of reference, and we evaluated the effect of heart rate on the diagnostic performance, image quality and radiation exposure of 64-slice DSCT coronary angiography. Although this retrospective study may have included possible false-positive or negative cases as all the patients didn't undergo invasive coronary angiography, the diagnostic performance of 64-slice DSCT for detecting coronary artery stenosis of 50% or greater in diameter in our study showed similar results to those of the prospective studies conducted in the past (6, 9, 10, 13, 15, 16) with a reported per-patient accuracy of 88-95%, a sensitivity of 96-100%, a specificity of 81-89%, a PPV of 79-94% and a NPV of 96-100%. Our results may suggest that DSCT has been well adapted to daily clinical settings, and it is an appropriate diagnostic tool for patients with suspected coronary artery disease.
In our study, flow-limiting coronary artery disease was revealed in only 26% of our patients on CT despite the fact that they were all symptomatic patients. The prevalence of coronary artery stenosis on CT seems to be lower than that in the previous reports. This may be because the previous reports, and even the prospective studies, had included patients who were already scheduled for invasive angiography, for which the prevalence of significant coronary artery stenosis is high (24). In fact, when we take a look at the 131 patients who underwent invasive angiography in our study, we observed a similarly high prevalence of coronary artery stenosis, which was 82% on the per-patient analysis. However, as CT has been widely used as a tool for screening patients suspected of having coronary artery stenosis due to its noninvasiveness and high negative predictive value, clinicians in our hospital order coronary CT for many patients with atypical chest pains to exclude the possibility of coronary artery disease. Therefore, had the previous studies included patients irrespective of whether or not they were to undergo invasive angiography, we can assume that their reported prevalence would also decrease.
In our study, DSCT demonstrated no decrease of the accessibility and diagnostic accuracy for the detection of coronary artery stenosis in patients with high heart rates and in those with high heart rate variability, which is in concordance with the previous results (7, 9, 10, 13, 16). However, our data did find significantly better image quality and there was an 18% reduction in the mean radiation dose exposure for the patients with a low heart rate, as compared to those patients with a high heart rate. Heart rate variability did not affect image quality, but the patients with low heart rate variability showed a 43% reduction of the mean radiation exposure compared to those patients with high heart rate variability. Different results have been reported for the radiation exposure of 64-slice DSCT coronary angiography with different results depending on the range of ECG pulsing, the tube voltage and the current or pitch used. In our hospital, we routinely used beta-blockers if there were no contraindications, and so we were able to perform a narrow range of ECG pulsing for a substantial proportion of the studied patients. Furthermore, we generally used a tube voltage of 100 kVp for most patients. Therefore, the DSCT coronary angiography in our study could be obtained with low radiation exposure, with a mean CTDIvol of 23.3 mGy and a mean effective dose of 5.8 mSv with ECG pulsing, which is half that of a recent report (16) using a tube voltage of 120 kV and optimal ECG pulsing.
In our study, we used 65 bpm as the cut-off value for the high heart rate group. The rationale for this cut-off value is that the resting period of the mid-diastole phase is significantly shortened above 65 bpm (25). Another reason is that the ECG-pulsing window for reducing the radiation dose was applied differently with using a heart rate of 65 bpm as a cut-off value. Although several studies have used 70 bpm as the cut-off value, we believe that there are no major differences with the use of either cut-off value.
Recent studies have focused on of the omission of beta-blocker when performing DSCT coronary angiography because the data demonstrated that DSCT without use of a beta-blocker achieved a sufficient diagnostic performance due to the high temporal resolution of 64-slice DSCT even for patients with a high heart rate (1, 3, 6, 7, 9, 10, 12, 16). However, with the reduction of the radiation exposure and the quality of the images created, the use of beta-blocker during 64-slice DSCT coronary angiography should be strongly considered in routine clinical practice. In addition, although no significant difference was observed in the diagnostic performance depending on the heart rate, acquiring good image quality would obviously enhance radiologists' diagnostic confidence in clinical practice.
This study had several limitations. First, this study was based on a retrospective design and it was a single center's experience. Thus, not all patients that underwent DSCT received invasive coronary angiography. As the patients with positive reports on DSCT coronary angiography or who had clinically significant symptoms tended to undergo further work-up, a verification bias may have influenced our results, leading to a per-patient and per-segment prevalence for coronary artery stenosis as high as 82% and 15%, respectively. Second, the patients did not undergo DSCT coronary angiography and invasive angiography within 48 hrs, and the time interval between DSCT and invasive coronary angiography varied. Third, the number of patients with a high heart rate and high heart rate variability was relatively small as beta-blockers were routinely used in this study. Fourth, the radiation exposure was estimated in 59% of the 729 patients, and the scan range was not evaluated in each patient. However, the CTDIvol can be used to compare the radiation exposure between groups because it is not affected by the scan range. Fifth, in this study, the same ECG pulsing window as was used for the patients with an intermediate heart rate applied for the patients with a high heart rate. For the patients with a heart rate of greater than 80 bpm, additional radiation reduction might have been possible by applying narrow ECG pulsing during end systole (16). Last, the image quality or diagnostic accuracy can be also affected by coronary calcium or the body mass index, in addition to the heart rates. However, in this study, we didn't evaluate the coronary calcium scores or the body mass index.
In conclusion, DSCT coronary angiography is an accurate modality that shows highly reproducible diagnostic accuracy in the clinical setting. Our study showed no difference in diagnostic accuracy according to the heart rate, but there was better image quality for the patients with a low heart rate, and a significant reduction of radiation exposure for the patients with a low heart rate or low heart rate variability.
Figures and Tables
Fig. 1
Flow chart for routine work-up for 729 patients who underwent 64-slice dual-source CT coronary angiography.
Treadmill test or myocardial single photon emission CT (SPECT) was performed within one month before or after dual-source CT coronary angiography. Invasive coronary angiography was performed within three months after dual-source CT coronary angiography.

Fig. 2
Coronary angiography in 65-year-old male with mean heart rate of 48 beats per minute (bpm) and his heart rate variability was 15 bpm. Volume CT dose index (CTDIvol) and effective dose were 21.1 mGy and 5.4 mSv, respectively.
CT volume-rendered reconstruction (A, B) and conventional angiogram (D) show significant stenosis of right coronary artery (arrows). Mild degree of severe stair-step artifacts (white arrowheads) was observed on volume-rendered reconstruction (A) and curved multiplanar reconstruction (C). Of note, severe stenosis of posterior descending coronary artery (black arrowhead) was also seen on volume-rendered reconstruction (B). Conventional angiogram (D) taken on same day does not show stenosis of posterior descending artery (arrowhead). This is false positive case.

Fig. 3
Coronary angiography in 54-year-old male with mean heart rate of 63 beats per minute (bpm) and his heart rate variability was 5 bpm. Volume CT dose index (CTDIvol) and effective dose were 18.0 mGy and 4.5 mSv, respectively.
CT volume-rendered reconstruction (A, B) and conventional angiogram (D, E) show significant stenosis of proximal left anterior descending artery (black arrows) and diagonal branch (white arrows). Radiologist well detected these lesions and they were mentioned on radiologic report. At same time, total segmental occlusion of distal left circumflex artery (arrowheads) was noted (B, E). Mixed plaque occluding lumen of left circumflex artery (white arrowheads) was well depicted on curved multiplanar reconstruction (F). However, in clinical practice, there was no mention of this on radiologic report. Unenhanced left circumflex artery (white arrowhead) is slightly enlarged and it may have been missed since it looks like cardiac vein on axial transverse image (C).

References
1. Achenbach S, Ropers D, Kuettner A, Flohr T, Ohnesorge B, Bruder H, et al. Contrast-enhanced coronary artery visualization by dual-source computed tomography--initial experience. Eur J Radiol. 2006. 57:331–335.
2. Johnson TR, Nikolaou K, Wintersperger BJ, Leber AW, von Ziegler F, Rist C, et al. Dual-source CT cardiac imaging: initial experience. Eur Radiol. 2006. 16:1409–1415.
3. Scheffel H, Alkadhi H, Plass A, Vachenauer R, Desbiolles L, Gaemperli O, et al. Accuracy of dual-source CT coronary angiography: first experience in a high pre-test probability population without heart rate control. Eur Radiol. 2006. 16:2739–2747.
4. Burgstahler C, Reimann A, Drosch T, Heuschmid M, Brodoefel H, Tsiflikas I, et al. Cardiac dual-source computed tomography in patients with severe coronary calcifications and a high prevalence of coronary artery disease. J Cardiovasc Comput Tomogr. 2007. 1:143–151.
5. Heuschmid M, Burgstahler C, Reimann A, Brodoefel H, Mysal I, Haeberle E, et al. Usefulness of noninvasive cardiac imaging using dual-source computed tomography in an unselected population with high prevalence of coronary artery disease. Am J Cardiol. 2007. 100:587–592.
6. Johnson TR, Nikolaou K, Busch S, Leber AW, Becker A, Wintersperger BJ, et al. Diagnostic accuracy of dual-source computed tomography in the diagnosis of coronary artery disease. Invest Radiol. 2007. 42:684–691.
7. Leber AW, Johnson T, Becker A, von Ziegler F, Tittus J, Nikolaou K, et al. Diagnostic accuracy of dual-source multi-slice CT-coronary angiography in patients with an intermediate pretest likelihood for coronary artery disease. Eur Heart J. 2007. 28:2354–2360.
8. Oncel D, Oncel G, Tastan A. Effectiveness of dual-source CT coronary angiography for the evaluation of coronary artery disease in patients with atrial fibrillation: initial experience. Radiology. 2007. 245:703–711.
9. Ropers U, Ropers D, Pflederer T, Anders K, Kuettner A, Stilianakis NI, et al. Influence of heart rate on the diagnostic accuracy of dual-source computed tomography coronary angiography. J Am Coll Cardiol. 2007. 50:2393–2398.
10. Brodoefel H, Burgstahler C, Tsiflikas I, Reimann A, Schroeder S, Claussen CD, et al. Dual-source CT: effect of heart rate, heart rate variability, and calcification on image quality and diagnostic accuracy. Radiology. 2008. 247:346–355.
11. Donnino R, Jacobs JE, Doshi JV, Hecht EM, Kim DC, Babb JS, et al. Dual-source versus single-source cardiac CT angiography: comparison of diagnostic image quality. AJR Am J Roentgenol. 2009. 192:1051–1056.
12. Fang XM, Chen HW, Hu XY, Bao J, Chen Y, Yang ZY, et al. Dual-source CT coronary angiography without heart rate or rhythm control in comparison with conventional coronary angiography. Int J Cardiovasc Imaging. 2010. 26:323–331.
13. Meng L, Cui L, Cheng Y, Wu X, Tang Y, Wang Y, et al. Effect of heart rate and coronary calcification on the diagnostic accuracy of the dual-source CT coronary angiography in patients with suspected coronary artery disease. Korean J Radiol. 2009. 10:347–354.
14. Rixe J, Rolf A, Conradi G, Moellmann H, Nef H, Neumann T, et al. Detection of relevant coronary artery disease using dual-source computed tomography in a high probability patient series: comparison with invasive angiography. Circ J. 2009. 73:316–322.
15. Tsiflikas I, Brodoefel H, Reimann AJ, Thomas C, Ketelsen D, Schroeder S, et al. Coronary CT angiography with dual source computed tomography in 170 patients. Eur J Radiol. 2010. 74:161–165.
16. Weustink AC, Neefjes LA, Kyrzopoulos S, van Straten M, Neoh Eu R, Meijboom WB, et al. Impact of heart rate frequency and variability on radiation exposure, image quality, and diagnostic performance in dual-source spiral CT coronary angiography. Radiology. 2009. 253:672–680.
17. Flohr TG, McCollough CH, Bruder H, Petersilka M, Gruber K, Suss C, et al. First performance evaluation of a dual-source CT (DSCT) system. Eur Radiol. 2006. 16:256–268.
18. Burgstahler C, Reimann A, Brodoefel H, Daferner U, Herberts T, Tsiflikas I, et al. Quantitative parameters to compare image quality of non-invasive coronary angiography with 16-slice, 64-slice and dual-source computed tomography. Eur Radiol. 2009. 19:584–590.
19. McCollough CH, Primak AN, Saba O, Bruder H, Stierstorfer K, Raupach R, et al. Dose performance of a 64-channel dual-source CT scanner. Radiology. 2007. 243:775–784.
20. Stolzmann P, Scheffel H, Schertler T, Frauenfelder T, Leschka S, Husmann L, et al. Radiation dose estimates in dual-source computed tomography coronary angiography. Eur Radiol. 2008. 18:592–599.
21. Weustink AC, Mollet NR, Pugliese F, Meijboom WB, Nieman K, Heijenbrok-Kal MH, et al. Optimal electrocardiographic pulsing windows and heart rate: effect on image quality and radiation exposure at dual-source coronary CT angiography. Radiology. 2008. 248:792–798.
22. Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, et al. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975. 51:5–40.
23. Gouya H, Varenne O, Trinquart L, Touze E, Vignaux O, Spaulding C, et al. Coronary artery stenosis in high-risk patients: 64-section CT and coronary angiography--prospective study and analysis of discordance. Radiology. 2009. 252:377–385.
24. Hamon M, Morello R, Riddell JW. Coronary arteries: diagnostic performance of 16- versus 64-section spiral CT compared with invasive coronary angiography--meta-analysis. Radiology. 2007. 245:720–731.
25. Wang Y, Vidan E, Bergman GW. Cardiac motion of coronary arteries: variability in the rest period and implications for coronary MR angiography. Radiology. 1999. 213:751–758.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download