Abstract
Objective
To evaluate the spectrum, prevalence, and significance of incidental non-cardiac findings (INCF) in patients referred for a non-invasive coronary angiography using a 128-slice multi-detector CT (MDCT).
Materials and Methods
The study subjects included 1,044 patients; 774 males (mean age, 59.9 years) and 270 females (mean age, 63 years), referred for a coronary CT angiography on a 128-slice MDCT scanner. The scans were acquired from the level of the carina to just below the diaphragm. To evaluate INCFs, images were reconstructed with a large field of view (> 300 mm) covering the entire thorax. Images were reviewed in the axial, coronal, and sagittal planes, using the mediastinal, lung, and bone windows. The INCFs were classified as severe, indeterminate, and mild, based on their clinical importance, and as thoracic or abdominal based on their locations.
Results
Incidental non-cardiac findings were detected in 56% of patients (588 of 1,044), including 435 males (mean age, 65.6 years) and 153 females (mean age, 67.9 years). A total of 729 INCFs were observed: 459 (63%) mild (58% thoracic, 43% abdominal), 96 (13%) indeterminate (95% thoracic, 5% abdominal), and 174 (24%) severe (87% thoracic, 13% abdominal). The prevalence of severe INCFs was 15%. Two severe INCFs were histologically verified as lung cancers.
Conclusion
The 128-slice MDCT coronary angiography, in addition to cardiac imaging, can provide important information on the pathology of the chest and upper abdomen. The presence of severe INCFs is not rare, especially in the thorax. Therefore, all organs in the scan should be thoroughly evaluated in daily clinical practice.
Over the past few years, the multi-detector CT (MDCT) has been used with increasing frequency as a non-invasive method for coronary artery assessment (1). Current CT technology enables imaging of the coronary arteries with the development of the last generation MDCT scanners that have submillimeter slice collimation and high temporal resolution (2). Although a coronary computed CT angiography (CCTA) is mainly focused on the assessment of the coronary, aortic, and cardiac structures, portions of the non-cardiac structures are visible on the scan as well (2, 3). Lesions depicted incidentally during CCTA can often be clinically significant and present a challenge to physicians.
The study of the coronary arteries requires a small field of view (FOV) in order to ensure optimal spatial resolution. However, for the evaluation of non-cardiac structures, reconstructions with a larger FOV can additionally be acquired to encompass the entire thorax. Estimation of non-cardiac structures during CCTA is an issue of controversy in the literature. Several authors support that incidental non-cardiac findings (INCFs) should be reported in CCTA examinations, since their prevalence ranges between 15-58% (4-10). Others support that the detection of incidental findings is likely to cause additional costs and anxiety to the patients without any proven benefit (11). In the present study, we retrospectively assess the spectrum, prevalence, and significance of INCFs in an outpatient population referred for clinically indicated CCTA using a 128-slice MDCT scanner.
This retrospective study included 1,044 patients (774 males, mean age of 59.9 years and 270 females, mean age of 63.0 years) referred for CCTA, between February 2008 to March 2009. The indications for CCTA were an abnormal, equivocal or non-diagnostic stress test, chest pain, evaluation of cardiomegaly and congestive heart failure, as well as the evaluation of cardiac aetiology of syncope. Patients with a intermediate probability of coronary artery disease (CAD) were also referred for a CCTA as a first test. The above are considered appropriate indications for CCTA, based on the criteria of the American College of Cardiology (ACC) (12) and the recent American Heart Association Scientific Statement on Cardiac CT (13). Exclusion criteria for CCTA included the presence of multiple ectopic beats, atrial fibrillation, renal failure, and a history of allergic reaction to iodine-containing contrast agents. The cardiovascular risk factors of the study group were recorded. Smoking was the most frequent risk factor for CAD (72%), followed by hypertension (68%), hyperlipidemia (60%), and diabetes mellitus (11%). The pre-test probability of CAD was defined based on clinical symptoms, age, and gender according to the Diamond and Forrester classification (14). Of the 1,044 patients analyzed, 279 (27%) had a low probability (<30%) and 765 (73%) had an intermediate probability (30-70%) of CAD. There were no high-risk patients for CAD in this study, as they were referred directly for a conventional coronary angiography. Informed consent was obtained from each participant.
Coronary CT angiography examinations were performed on a 128-slice MDCT (DEFINITION AS PLUS 128, Siemens, Germany) using retrospective electrocardiographic (ECG) gating with the following parameters: 128 × 0.6 collimation, 0.3 sec rotation time, pitch of 0.32, 120 kV tube voltage and 185 reference mAs. Patients with heart rates over 75 bpm with no contraindications to the use of beta-blockers received metoprolol orally 1 hour before the examination to reduce heart rate. Image acquisition was performed during inspiratory breath-hold. To familiarize the patient with the protocol, breath-holding was practiced before the examination.
The CCTA protocol was the following: at the beginning of the examination, a non-contrast localization scan was performed to plan the scan volume. The acquisition delay time was determined by injection of 20 ml test-bolus at 5 ml/sec. The peak time of test-bolus enhancement was used as a delay time. A non-ionic contrast medium (Iomeron 400 mg iodine/ml; Bracco Altana Pharma, Germany) was infused through an 18-G intravenous antecubital catheter at 5 ml/sec. The total contrast dosage for the CCTA was adapted to the calculated scan duration (5 ml/sec + 5 ml, total 65-80 ml, infusion rate 5.0 ml/sec, saline bolus 50 ml, flow 5 ml/sec). Patients were scanned in the supine position twice, first without contrast medium to calculate the calcium score and secondly after contrast medium injection. Studies were acquired in the cranio-caudal direction from the level of the carina to just below the diaphragm.
All CT datasets were transferred to a dedicated workstation (Circulation, Siemens). Images were reconstructed at an effective slice thickness of 0.6 mm and a retrospective ECG gating at 10% steps throughout the cardiac cycle. The best mid-late systolic (20-40% of RR-interval) or mid-late diastolic (50-70% of RR-interval) data set was chosen for final image interpretation. To evaluate the coronary arteries, the images were reconstructed with a small FOV (120-190 mm), which was restricted to the heart region and a medium-smooth convolution kernel (B 26f). Additionally, for the evaluation of INCFs, images were reconstructed with a large FOV (> 300 mm) at an effective slice thickness of 0.6 mm, from the outer rib to outer rib covering the entire thorax. The images were reviewed in the axial, coronal, and sagittal planes, using a mediastinal window (width: 450, level: 35), lung window (width: 1,500, level: -700), and bone window (width: 1,500, level: 450) for all examinations.
Each CT examination was retrospectively reviewed by two experienced radiologists in consensus and the INCFs were reported. The K-value for the inter-observer agreement was 0.89.
Incidental non-cardiac findings were classified as thoracic, when located above the diaphragm and abdominal, when located below the diaphragm. INCFs were also classified according to their clinical significance as severe, indeterminate, and mild. A similar classification system was used by Kirsch et al. (15). Severe findings were those of definite clinical importance, requiring immediate evaluation or intervention. Indeterminate findings were those of potential clinical importance, requiring a follow-up study or correlation with the patient's history. Finally, mild findings were those considered to be of little clinical significance with no further need of follow-up. Further work-up of patients after CCTA detection of indeterminate and severe INCFs is described in Figure 1.
For several INCFs a criterion was established. For abdominal findings, steatosis was used to describe diffuse low attenuation of the liver parenchyma. Smooth non-enhancing water attenuation lesions of the liver were described as liver cysts. Peripherally calcified liver cysts were described as echinococcus cysts. Nodular peripherally enhancing smooth liver lesions were characterized as haemangiomas. For the thoracic findings, pulmonary nodules were characterized based on their size, according to the current Fleischner criteria (16). However, if the nodules were found to be smaller than 8 mm, but with other imaging characteristics to suggest malignancy, they were classified as severe. Areas with increased attenuation in lung parenchyma were characterized as consolidations or ground glass opacities, and low attenuation areas as emphysema. A diagnosis of interstitial lung disease was given when interlobular septal thickening was present in the absence of findings of congestive heart failure. An aortic diameter at the level of the ascending aorta of > 4 cm was considered aneurysmal, while for the abdominal aorta a diameter of > 3.5 cm was considered aneurysmal. The diagnosis of pulmonary embolization was based on the presence of filling defects in the pulmonary arteries and the diagnosis of pulmonary hypertension on the presence of dilated pulmonary arteries. For the lymphadenopathy, the criterion was a diameter of the short axis > 1 cm.
The additional reconstructions performed for INCF detection with a large FOV, at three planes and three windows significantly increased the total time for reviewing each CCTA examination. INCFs were detected in 588 patients (56%); 435 males (mean age of 65.6 years) and 153 females (mean age of 67.9 years). In 135 patients (13%) multiple INCFs were depicted.
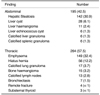
A total of 729 INCFs were found: 459 (63%) were classified as mild, 96 (13%) as indeterminate and 174 (24%) as severe. Specifically, 305 of the 459 mild INCFs (66%) were detected in men (mean age of 59.4 years), whereas the other 154 of the 459 (34%) were found in women (mean age of 59.9 years). Moreover, 71 of the 96 indeterminate INCFs (74%) were detected in men (mean age of 62.3 years), whereas 25 of the 96 (26%) were found in women (mean age of 64.1 years). Finally, 133 of the 174 severe INCFs (76%) were detected in men (mean age of 67.7 years), while 41 of the 174 (24%) were found in women (mean age of 69.1 years). The 174 severe INCFs were found in 151 patients. The prevalence of severe INCFs was 15%.
The mild findings were 58% (264 of 459) thoracic and 43% (195 of 459) abdominal, while indeterminate findings were 95% (91 of 96) thoracic and 5% (5 of 96) abdominal. Lastly, the severe findings were 87% (152 of 174) thoracic and 13% (22 of 174) abdominal.
Mild abdominal findings included hepatic steatosis, liver cyst (Fig. 2), liver haemangioma, liver echinococcus cyst, calcified liver granuloma, and calcified splenic granuloma (Table 1). Mild thoracic findings included emphysema, calcified lung granuloma, bone haemangioma, bronchiectasis, hiatus hernia (Fig. 3), calcified lymph nodes, remote fracture, and substernal thyroid (Table 1).
The only indeterminate abdominal finding was ascites (Table 2) (Fig. 2). Indeterminate thoracic findings included pulmonary nodules > 0.8 cm and < 3 cm, consolidation or ground glass opacities (Fig. 4), pleural effusion, atelectasis, interstitial lung disease, pleural thickening, mediastinal mass lesions, and thoracic adenopathy (Table 2).
Severe abdominal findings included liver masses and abdominal aortic aneurysms (Table 3). Severe thoracic findings included an ascending aortic aneurysm (Fig. 5), dilated aortic root, pulmonary embolization, pulmonary hypertension, pulmonary nodules > 3 cm, and pulmonary nodules of any size with malignant characteristics (Table 3).
A comparison with previous radiological studies was available in a number of cases, but further follow-up was possible in a limited number of cases. In 10 patients, pulmonary nodules classified as indeterminate were known from previous thorax CT examinations. No change in size was detected within 2 or more years and the nodules were considered mild. In three of these patients, pleural thickening was also noted, which remained stable and was also considered mild. For the indeterminate and severe pulmonary nodules, either a follow-up with thorax CT or further evaluation via biopsy was recommended. A pathological verification was only available for 2 of the 9 pulmonary nodules > 3 cm, which proved to be malignant (Fig. 6). All three patients with consolidation or ground glass opacities had mediastinal lymphadenopathy and received antibiotic therapy. A radiological follow-up with X-rays showed regression of the lung lesions. Three patients with pleural effusions had a known history of congestive heart failure and the effusions existed in recent previous X-rays. Hence, the effusions were attributed to the heart failure. All three patients with pulmonary emboli received anticoagulant therapy.
Overreading cardiac imaging examinations for the presence of INCFs has been a subject of study, both with CT and MRI techniques. Several studies have reported the prevalence of INCFs using electron-beam CT (EBCT). Horton et al. (17) studied 1,326 screening EBCT examinations and found significant extra-cardiac pathology in 8% of the examinations. In a similar study of 1,812 EBCT examinations, Hunold et al. (18) found INCFs in 34% of the patients examined. Although those findings included a number of clinically insignificant abnormalities, there was a need for the further testing of 9% of the 2,055 total extra-coronary findings. In the study by Schragin et al. (19) 278 of 1,356 patients (21%) undergoing EBCT had one or more INCFs.
Data on extra-cardiac findings during cardiac MRIs are limited. McKenna et al. (20) reported extra-cardiac findings in 107 of 132 (81%) elderly patients (mean age, 74 years) undergoing a cardiac MRI; 63 of 131 (48%) patients had multiple findings. A total of 224 incidental findings were visualized, including at least one potentially significant lesion in 23 of 135 (17%) patients and one moderately significant finding in 43 of 129 (33%) patients.
Mueller et al. (7), who scanned patients with a 16-MDCT scanner from the subclavian artery level, through the apex of the heart to asses graft patency after coronary artery bypass graft (CABG) surgery, found that 34 of 259 patients (13%) had INCFs, including pulmonary embolisms, lung cancer and pneumonia. Dewey et al. (5) reported an INCF incidence of 5% for clinically significant findings, and only 10% for non-significant findings in a cohort of 108 patients scanned with a 16-row MDCT. However, Gil et al. (9) reported extra-cardiac findings in 56% of the examined patients in their study, without classification by severity, in a cohort of 258 patients also scanned with a 16-row MDCT. In the study of Law et al. (10) with a 16-MCDT scanner, 56 out of 295 patients (19%) had significant extra-coronary findings on CCTAs requiring clinical or radiological follow up. There were 60 significant extra-coronary findings. A study by Onuma et al. (8) reported a 58% prevalence of INCFs among 503 patients referred for CCTA using 16-slice and 64-slice MDCT scanners. They found 23% of the patients with clinically significant non-cardiac pathology requiring additional work-up, and four cases (1%) of malignancy.
To our knowledge, this is the first study to report INCFs from a CCTA on a 128-slice MDCT scanner. Our study is also the first, to our knowledge, to include such a high number of patients examined with contrast medium-enhanced CCTA.
The significance of using a large FOV, encompassing the entire thorax, versus a small FOV, encompassing only the heart, during image reconstruction for evaluation of extra-cardiac structures, has been documented in previous reports. Aglan et al. (21) studied the prevalence of extra-coronary findings using both a full "thoracic" FOV and a small "cardiac" FOV and found a higher detection rate of clinically significant findings by using the former compared to the latter (26% versus 15%) (p < 0.001). Northam et al. (22) compared the frequency of detection of pulmonary nodules on cardiac CT scans acquired with a limited and a full FOV, and concluded that viewing cardiac CT scans at a limited FOV only can result in missing more than 67% of the nodules larger than 1 cm and more than 80% of nodules smaller than 1 cm. Haller et al. (6) measured the volumes of the displayed body structures and found that 36% of the total chest volume was displayed on a dedicated CCTA focused on the heart, whereas 70% of the chest was visible when the CCTA raw data were reconstructed with a maximal field of view (p < 0.001). In our study, a small FOV, restricted to the heart, was used for the evaluation of the coronary arteries and additional reconstruction of images with a large FOV to encompass the entire thorax was performed in order to evaluate the presence of INCFs.
The necessity to look for INCFs when practising cardiac imaging has been an issue of debate in the literature. In the study by Budoff and Gopal (11), it is suggested that reanalyzing the data set for extra-cardiac disease would lead to additional costs and anxiety to the patient, while benefits have not yet been scientifically proven. Wann et al. (3) also stated that although recommendations for image reconstruction and training in the interpretation of incidental findings continue to evolve, CCTA should be focused primarily on the coronary arteries.
Many studies, on the other hand, suggest that CCTA scans can reveal important abnormalities in extra-cardiac structures contained in the scanned volume and therefore, the entire examination should be reconstructed with the maximum field of view and should be reviewed by qualified radiologists or cardiologists for the presence of INCFs (4, 6-10, 15).
Yiginer et al. (23) stated that it is controversial whether the incidental detection of non-cardiac pathology on coronary CT is an advantage, because additional diagnostic procedures with added costs may be needed. However, they suggest that the entire thorax should be scanned on calcium score imaging for smokers over 50 years in order to detect potentially malignant pulmonary nodules, because lung cancer is the most common fatal malignancy. Kim et al. (24) report that it would be beneficial to include whole thorax low dose CT in the CCTA protocol because it enables high-risk patients to undergo simultaneous screening for lung cancer and coronary artery disease with acceptable radiation exposure. However, the benefits of screening for lung cancer itself remain questionable (25).
While the detection of major abnormalities, like aortic dissection or pulmonary embolization is of obvious clinical importance, the detection of incidental abnormalities such as small pulmonary nodules less than 4 mm in diameter, has not yet been shown to positively affect patient outcomes and may lead to unnecessary testing (3). In a summary of the literature by Colletti (26) on incidental findings detected with cardiac imaging, it is reported that it is likely that depending on the cohort, one in 100 to fewer than one in 1,000 patients may benefit from serendipitous discovery of extra-cardiac lesions.
Incidental findings will always be found in medical imaging, including CCTA, and the decision of how to evaluate them as well as how to consult with the patients will continue to be an issue of discussion and probable debate. Although the benefits of evaluating INCFs have not been scientifically validated, we consider that the best approach is to view all available data in each CCTA study, report all non-cardiac findings estimating their clinical significance, and consult each patient appropriately. Specifically, the early detection of lung cancer is an issue of great importance; in our study, two patients were diagnosed with lung cancer. Accordingly, specialists who interpret CCTAs should be trained and qualified enough to recognize and evaluate extra-cardiac pathologies.
The limitations of our study include the presence of limited follow-up data, as well as the absence of histopathological verification of indeterminate and most of severe INCFs. In prior literature, limited follow-up data for INCFs during cardiac imaging have been reported (5, 8-10). The proven outcome of INCFs was reported in seven out of 617 cases in a study by Kawano et al. (4), three out of 166 cases in a study by Haller et al. (6), nine out of 259 cases in a study by Mueller et al. (7), and 15 out of 1,764 cases in a study by Northam et al. (22). In our study, 24 out of 729 INCFs had a proven outcome.
In conclusion, a review of the available non-cardiac CCTA data is advised, with the awareness that this may lead to further and sometimes unnecessary testing. The lungs, mediastinum, bones, and upper abdomen should be reviewed using appropriate mediastinal, bone, and lung windows and a large FOV to include the entire thorax. Patients should undergo clinical consultation based on the abnormalities seen in structures other than the coronary arteries during CCTA.
Figures and Tables
Fig. 1
Description of further work-up of patients with indeterminate and severe incidental non-cardiac findings detected by coronary CT angiography.

Fig. 2
Liver cyst (arrow) and ascites (asterisk) incidentally detected in 71-year-old man who was referred for coronary CT angiography for congestive heart failure.
Fig. 3
Incidentally detected hiatus hernias.
A. Hiatus hernia (arrow) is depicted in axial plane in 65-year-old man who underwent coronary CT for atypical chest pain.
B. Hiatus hernia (arrow) is depicted in sagittal reconstruction of coronary CT angiography in 67-year-old man, also complaining of atypical chest pain.

Fig. 4
Consolidation of right lung discovered in 56-year-old man with cough who underwent coronary CT angiography for atypical chest pain.
Fig. 5
Aneurysm of ascending aorta measuring 4.7×4.8 cm incidentally found in 62-year-old man who was referred for coronary CT angiography for evaluation of cardiac aetiology of syncope.

Fig. 6
Incidentally detected bronchogenic carcinoma in 65-year-old man.
A, B. Mass measuring 4.5 cm in diameter at right hilum is discovered. Pathology revealed squamous cell lung cancer (arrows) on axial plane soft tissue window (A) and coronal plane lung window (B) images.

References
1. Schoepf UJ, Becker CR, Ohnesorge BM, Yucel EK. CT of coronary artery disease. Radiology. 2004. 232:18–37.
2. Achenbach S. Current and future status on cardiac computed tomography imaging for diagnosis and risk stratification. J Nucl Cardiol. 2005. 12:703–713.
3. Wann S, Rao P, Des Prez R. Cardiac computed tomographic angiography: evaluation of non-cardiac structures. J Nucl Cardiol. 2009. 16:139–150.
4. Kawano Y, Tamura A, Goto Y, Shinozaki K, Zaizen H, Kadota J. Incidental detection of cancers and other non-cardiac abnormalities on coronary multislice computed tomography. Am J Cardiol. 2007. 99:1608–1609.
5. Dewey M, Schnapauff D, Teige F, Hamm B. Non-cardiac findings on coronary computed tomography and magnetic resonance imaging. Eur Radiol. 2007. 17:2038–2043.
6. Haller S, Kaiser C, Buser P, Bongartz G, Bremerich J. Coronary artery imaging with contrast-enhanced MDCT: extracardiac findings. AJR Am J Roentgenol. 2006. 187:105–110.
7. Mueller J, Jeudy J, Poston R, White CS. Cardiac CT angiography after coronary bypass surgery: prevalence of incidental findings. AJR Am J Roentgenol. 2007. 189:414–419.
8. Onuma Y, Tanabe K, Nakazawa G, Aoki J, Nakajima H, Ibukuro K, et al. Noncardiac findings in cardiac imaging with multidetector computed tomography. J Am Coll Cardiol. 2006. 48:402–406.
9. Gil BN, Ran K, Tamar G, Shmuell F, Eli A. Prevalence of significant noncardiac findings on coronary multidetector computed tomography angiography in asymptomatic patients. J Comput Assist Tomogr. 2007. 31:1–4.
10. Law YM, Huang J, Chen K, Cheah FK, Chua T. Prevalence of significant extracoronary findings on multislice CT coronary angiography examinations and coronary artery calcium scoring examinations. J Med Imaging Radiat Oncol. 2008. 52:49–56.
11. Budoff MJ, Gopal A. Incidental findings on cardiac computed tomography. Should we look? J Cardiovasc Comput Tomogr. 2007. 1:97–105.
12. Hendel RC, Patel MR, Kramer CM, Poon M, Hendel RC, Carr JC, et al. ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American College of Radiology, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, American Society of Nuclear Cardiology, North American Society for Cardiac Imaging, Society for Cardiovascular Angiography and Interventions, and Society of Interventional Radiology. J Am Coll Cardiol. 2006. 48:1475–1497.
13. Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P, et al. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006. 114:1761–1791.
14. Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med. 1979. 300:1350–1358.
15. Kirsch J, Araoz PA, Steinberg FB, Fletcher JG, McCollough CH, Williamson EE. Prevalence and significance of incidental extracardiac findings at 64-multidetector coronary CTA. J Thorac Imaging. 2007. 22:330–334.
16. MacMahon H, Austin JH, Gamsu G, Herold CJ, Jett JR, Naidich DP, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005. 237:395–400.
17. Horton KM, Post WS, Blumenthal RS, Fishman EK. Prevalence of significant noncardiac findings on electron-beam computed tomography coronary artery calcium screening examinations. Circulation. 2002. 106:532–534.
18. Hunold P, Schmermund A, Seibel RM, Gronemeyer DH, Erbel R. Prevalence and clinical significance of accidental findings in electron-beam tomographic scans for coronary artery calcification. Eur Heart J. 2001. 22:1748–1758.
19. Schragin JG, Weissfeld JL, Edmundowicz D, Strollo DC, Fuhrman CR. Non-cardiac findings on coronary electron beam computed tomography scanning. J Thorac Imaging. 2004. 19:82–86.
20. McKenna D, Laxpati M, Colletti PM. The prevalence of incidental findings at cardiac MRI. Open Cardiovasc Med J. 2008. 2:20–25.
21. Aglan I, Jodocy D, Hiehs S, Soegner P, Frank R, Haberfellner B, et al. Clinical relevance and scope of accidental extracoronary findings in coronary computed tomography angiography: a cardiac versus thoracic FOV study. Eur J Radiol. 2009. [Epub ahead of print].
22. Northam M, Koonce J, Ravenel JG. Pulmonary nodules detected at cardiac CT: comparison of images in limited and full fields of view. AJR Am J Roentgenol. 2008. 191:878–881.
23. Yiginer O, Bas S, Pocan S, Yildiz A, Alibek S. Incidental findings of cardiac MSCT: who might benefit from scanning the entire thorax on Ca score imaging? Int J Cardiol. 2008. [Epub ahead of print].
24. Kim JW, Kang EY, Yong HS, Kim YK, Woo OH, Oh YW, et al. Incidental extracardiac findings at cardiac CT angiography: comparison of prevalence and clinical significance between precontrast low-dose whole thoracic scan and postcontrast retrospective ECG-gated cardiac scan. Int J Cardiovasc Imaging. 2009. 25:75–81.
25. Bach PB, Jett JR, Pastorino U, Tockman MS, Swensen SJ, Begg CB. Computed tomography screening and lung cancer outcomes. JAMA. 2007. 297:953–961.
26. Colletti PM. Incidental findings on cardiac imaging. AJR Am J Roentgenol. 2008. 191:882–884.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download