Abstract
Objective
To assess the diagnostic performance of MR arthrography in the diagnosis of the various types of partial-thickness rotator cuff tears by comparing the MR imaging findings with the arthroscopic findings.
Materials and Methods
The series of MR arthrography studies included 202 patients consisting of 100 patients with partial-thickness rotator cuff tears proved by arthroscopy and a control group of 102 patients with arthroscopically intact rotator cuffs, which were reviewed in random order. At arthroscopy, 54 articular-sided, 26 bursal-sided, 20 both articular- and bursal-sided partial-thickness tears were diagnosed. The MR arthrographies were analyzed by two radiologists for articular-sided tears, bursal-sided tears, and both articular- and bursal-sided tears of the rotator cuff. The sensitivity and specificity of each type of partial-thickness tears were determined. Kappa statistics was calculated to determine the inter- and intra-observer agreement of the diagnosis of partial-thickness rotator cuff tears.
Results
The sensitivity and specificity of the various types of rotator cuff tears were 85% and 90%, respectively for articular-sided tears, 62% and 95% for bursal-sided tears, as well as 45% and 99% for both articular- and bursal-sided tears. False-negative assessments were primarily observed in the diagnosis of bursal-sided tears. Conversely, both articular- and bursal-sided tears were overestimated as full-thickness tears. Inter-observer agreement was excellent for the diagnosis of articular-sided tears (k = 0.70), moderate (k = 0.59) for bursal-sided tears, and fair (k = 0.34) for both articular- and bursal-sided tears, respectively. Intra-observer agreement for the interpretation of articular- and bursal-sided tears was excellent and good, respectively, whereas intra-observer agreement for both articular- and bursal-sided tears was moderate.
Conclusion
MR arthrography is a useful diagnostic tool for partial-thickness rotator cuff tears, but has limitations in that it has low sensitivity in bursal- and both articular- and bursal-sided tears. In addition, it shows only fair inter-observer agreement when it comes to predicting both articular- and bursal-sided tears.
Partial-thickness rotator cuff tears are known to have a more significant role than previously recognized in shoulder pathology. Since partial-thickness tears have increasingly been regarded as a source of surgically treatable shoulder pain, the identification of even small tears has recently become more important (1). Partial-thickness tears are classified as articular-sided, bursal-sided, intra-tendinous or a combination of these patterns such as the involvement of both sides of the rotator cuff. Around 50% of the patients with bursal-sided tear also have an associated articular-sided tear (2).
The accuracy of conventional MR imaging for diagnosing partial-thickness tears is lower than that for full-thickness tears, although MR arthrography improves the sensitivity of diagnosing partial-thickness tears of the articular surface (3-6). Since results on the performance of MR arthrography in the diagnosis of partial-thickness tears were predominantly obtained in the series with articular-sided tears, further investigations are required to verify and analyze detection of different types of partial-thickness tears and limitation of this imaging modality. To our knowledge, there are few reports (7, 8) that document the comparison of accuracy and observer variability in the interpretation of MR arthrography for each type of partial-thickness rotator cuff tears.
The purpose of our study was to assess the diagnostic performance as well as the inter- and intra-observer variation of MR arthrography in the diagnosis of each type of partial-thickness rotator cuff tears by comparing them with arthroscopic findings.
This study was approved by our Institutional Review Board, and patient informed consent was waived for this retrospective study.
Surgical records of 294 patients with MR arthrography who had been referred to the department of orthopedic surgery for evaluation of shoulder pain over three years were reviewed in order to select patients for this study. The study included 202 patients (110 men and 92 women; mean age 51 years) including 100 patients (52 men and 48 women; mean age 54 years) with partial-thickness rotator cuff tears proved by arthroscopy and a control group of 102 patients (58 men and 44 women; mean age 47 years) with arthroscopically intact rotator cuffs. Inclusion criteria were: 1) a partial-thickness rotator cuff tear with information on the tear type as stated in the surgical record or 2) the description of a rotator cuff without pathologic findings as stated in the surgical records, 3) preoperative MR arthrography performed at our institution according to a standardized protocol, and 4) no history of previous shoulder surgery.
At arthroscopy, 54 articular-sided (Fig. 1), 26 bursal-sided (Fig. 2), and 20 both articular- and bursal-sided (Fig. 3) partial-thickness tears of the supraspinatus tendon were diagnosed. Arthroscopic diagnoses of the control group included 36 patients with superior labrum, to anterior posterior (SLAP) lesions, 25 with adhesive capsulitis, 17 with labral injuries, 13 with coexisting SLAP lesions and antero-inferior labral injuries, and 11 without any pathologic findings.
All arthroscopies were performed by one experienced orthopedic surgeon who knew the results of the MR imaging. The average interval between the MR imaging and arthroscopy of the 202 patients was three months (range, 20 days to 5 months).
Under fluoroscopic guidance a 20-22 gauge spinal needle was inserted through the medial border of the middle and lower third of the humeral head and placed into the glenohumeral joint. All patients had received 12-20 mL of an intra-articular contrast mixture via an anterior approach. The contrast mixture was obtained by combining 0.1 mL of gadopentetate dimeglumine (Magnevist; Schering, Berlin, Germany), 5 mL of iopromide (Ultravist 300; Schering, Berlin, Germany), 5 mL of 1% lidocain and 10 mL of saline. MR imaging was obtained within 30 min after contrast injection with a 1.5T system (Magnetom Avanto; Siemens Medical Solutions, Erlangen, Germany) and a dedicated shoulder array coil. Patients underwent imaging with their arm in a neutral position. Fat-suppressed T1-weighted spin-echo images (TR/TE 500-800/12-20) were obtained in the transverse plane, sagittal oblique plane (parallel to the glenohumeral joint), and coronal oblique plane (perpendicular to the glenohumeral joint space). T2-weighted fast spin-echo images (TR/TE 3000-4200/90-120) were obtained in the coronal oblique plane. Fat-suppressed T1-weighted images with an abduction external rotation view were performed, if the patient was able to tolerate this position. The parameters for all sequences were a section thickness of 3 mm with an intersection gap of 0.3 mm, matrix size of 256×192, and field of view ranging from 14-16 cm.
For imaging analysis, all MR images were placed in random order. Examinations were analyzed by two radiologists with more than 10 years' experience who were blinded to clinical and arthroscopic findings. Partial-thickness tears can be classified into three subtypes: articular-sided tears, bursal-sided tears, and both articular- and bursal-sided tears. Articular-sided tears were diagnosed on images if the focal disruption on the undersurface of the tendon or defect of the cuff fiber was filled with high signal contrast material, but did not extend to the bursal surface. Bursal-sided tears were diagnosed when focal fluid or near-fluid signal intensity with disruption of integrity of the subacromial bursal fat stripe extended to the inferior surface, but did not follow from one surface to the other. Both articular- and bursal-sided tears were defined as showing a defect of the cuff fiber along both the articular and bursal surfaces, which did not communicate between the two surfaces. All imaging sequences were concerned with the diagnosis of each tear. This study did not include an intratendinous tear as a type of partial-thickness tear because it could not be confirmed by arthroscopy. In each case, observers recorded their types of partial-thickness rotator cuff tears and the degree of confidence for a given type (equivocal, fairly confident, or confident). After at least a 3-week interval, MR images were reviewed in the same random order for intra-observer agreement.
With arthroscopy as the standard of reference, the sensitivity, specificity, and the negative and positive predictive values for the detection of each type of partial-thickness tears were determined. In the calculation of sensitivity and specificity for a particular type of partial-thickness tears, the MR imaging and arthroscopy were divided into two groups; the type we were concerned with and the other types. Thus, for example, in articular-sided tears, the two groups are 'articular-sided tear' and 'not articular-sided tear'. The sensitivity is the proportion of true-positive diagnoses of an 'articular side tear'; whereas, the specificity is the proportion of true-negative diagnosis of 'not articular-sided tear'.
Inter- and intra-observer agreements for the detection of each type of partial-thickness tears were calculated using Kappa statistics. The Kappa values can be interpreted as poor (k = 0-0.20), fair (k = 0.21-0.40), moderate (k = 0.41-0.60), good (k = 0.61-0.80), and excellent (k = 0.81-1.00). Proportions of studies in which a confident diagnosis was made were calculated for each reader and each type of partial-thickness tears. The significance the difference was determined by way of a Chi-square test.
All analyses were performed with the MedCalc software program (version 11.2.1. Mariakerke, Belgium).
On MR arthrography, 61 articular-sided, 24 bursal-sided, and 11 both articular- and bursal-sided partial-thickness tears were interpreted. Considering all types of partial-thickness tears, MR arthrography had an overall sensitivity of 88% (88 of 100 cases), a specificity of 82% (84 of 102 cases), a negative predictive value of 88% (84 of 96 cases), and a positive predictive value of 83% (88 of 106 cases) for the detection of tears.
The results of the diagnostic efficacy of MR arthrography in the diagnosis for each type of partial-thickness tears are presented in Table 1. Eight articular-sided tears were missed or incorrectly diagnosed at MR arthrography, whereas 15 articular-sided tears described on MR arthrography were described as another type of tear or tendon without tear on arthroscopy. In 11 of the 15 false-positive findings, synovitis, tendinosis or degenerative fraying of the tendons without tears was described in the corresponding arthroscopic reports.
Considering bursal-sided tears separately, 10 false-negative and eight false-positive assessments were observed on MR arthrography (Fig. 4).
In the detection of both articular- and bursal-sided tears, there were 11 false-negative findings (Fig. 5) and only two false-positive findings. In eight of 20 cases, both articular- and bursal-sided tears were overestimated as full-thickness tears on MR arthrography (Fig. 6). In two cases with both articular- and bursal-sided tears on MR arthrography, one case was an articular-sided tear, while the other case was of a patient with bursal-sided tear at arthroscopy.
Overall agreement for detection of partial-thickness tears between the two readers was good (k = 0.77) when all diagnoses were considered. Inter-observer agreements were good (k = 0.70) for the identification of articular-sided tear, moderate (k = 0.59) for bursal-sided tear, and fair (k = 0.34) for both articular- and bursal-sided tears. Exact agreement between arthroscopic and MR arthrographic classifications for the overall detection of partial-thickness tears occurred in 77% (155 of 202) cases.
Intra-observer agreement for each reader was excellent (k = 0.87, reader 1) and good (k = 0.80, reader 2) for the overall interpretation of partial-thickness tears. Intra-observer agreement for the interpretation of articular-sided tears were excellent (k = 0.86, reader 1) and good (k = 0.78, reader 2), whereas intra-observer agreement for bursal-sided tears were good (k = 0.68, reader 1; k = 0.70, reader 2). For both articular- and bursal-sided tears, intra-observer agreement was moderate (k = 0.51, reader 1; k = 0.43, reader 2).
The two readers were more confident in the diagnosis of articular-sided tears (confident in 80% and 75% of cases diagnosed) than the diagnosis of bursal-sided or both articular- and bursal-sided tears (p < 0.05).
The two readers were confident in the diagnosis of bursal-sided tears in 54% and 47% of cases; of both articular- and bursal-sided tears in 43% and 36%; and of normal tendons in 85% and 76%, respectively.
Although the incidence of partial-thickness rotator cuff tears has not been well researched, articular-sided tears were found to be more common than bursal-sided tears, and this is partially due to the hypovascularity which has been observed near the insertion of the rotator cuff tendon, especially on its articular surface (9-11). MR arthrography has been described as having variable accuracy for the diagnosis of partial-thickness tears as well as being more sensitive to articular-sided tears because intra-articular contrast outlines the undersurface of the rotator cuff (3, 5, 10, 12). In our study, diagnoses of articular-sided tears were made with accuracy consistent with previous studies.
Some diagnostic errors can still be made on MR arthrography, in which articular-sided tears are underestimated as being normal, or normal tendons with mild tendon degeneration are overestimated as tears. Upon inclusion of the abduction external rotation view in routine sequences of MR arthrography, there is an increase in the sensitivity of detection articular-sided partial-thickness tears of the rotator cuff tendon (13, 14). Some patients may not be tolerant of the abduction external rotation positioning due to the provocation of instability or pain. In our study, 13% of patients could not be evaluated in this position.
Bursal-sided tears, which are less common than articular-sided tears, are not likely to be detectable on the single T1-weighted fat-suppressed series of MR arthrography because contrast medium does not pass into the bursa. To be able to detect bursal-sided tears, it is crucial to include an oblique coronal T2-weighted image (with or without fat suppression). No difference in the detection of bursal-sided tears on MR arthrography versus conventional MR imaging was noted because the diagnosis was made based on T2-weighted images for both examinations (8). Fat-suppression techniques accentuate fluid signal contrast on T2-weighted images and have been suggested as a means of increasing sensitivity in the detection of partial-thickness tears. Clinical studies have, however, not consistently demonstrated an improved reliability with this technique (15). In routine, we prefer the non fat-suppressed T2-weighted images over fat-suppressed T2-weighted, because the rotator cuff anatomy is better depicted.
The diagnostic accuracy of MR arthrography in bursal-sided tears was low in relation to articular-sided tears as was expected in our study. The low sensitivity values can be explained by the underestimation of small bursal tear lesions on MR arthrography. Bursal-sided tears are sometimes more difficult to evaluate arthroscopically, since hypertrophic bursitis can obscure the cuff surface (16). In addition, the anatomic evaluation of the tendon contour would be obvious if additional non fat-suppressed sequences such as sagittal T2-weighted, sagittal T1-weighted, or coronal proton density-weighted images were included in our imaging protocol.
Magee (8) reported that MR arthrography sensitivity was 84% for bursal-sided tears and was higher than in our study. This difference may result from the MR imaging equipment used, which had 3-T field strength. The increase in signal-to-noise ratio of 3-T MR imaging has allowed for faster imaging with improved resolution and thinner slice thickness. MR imaging at 3-T appears particularly useful in the delineation of small full-thickness and partial-thickness tears (17).
Both articular- and bursal-sided tears are relatively uncommon compared to isolated articular- or bursal-sided tears. Ko et al. (18) examined 161 patients with different types of rotator cuff lesions and found only 10 patients with both articular- and bursal-sided tears, compared to 66 patients with either articular-sided or bursal-sided cuff tears. In our series, both articular- and bursal-sided tears consisted of 20% of all types of partial-thickness tears.
In our study, MR arthrography showed a markedly lower sensitivity in the detection of both articular- and bursal-sided tears compared with isolated articular or bursal-sided tears. This is the case because both articularand bursal-sided tears mimicked full-thickness tears in 40% of cases. Two factors can be overestimated as a full-thickness tear. First, the imbibition of contrast medium into the only remaining thin and friable tendon on both articular- and bursal-sided tears could lead to the diffusion of contrast medium along with the subdeltoid-subacromial bursa and false interpretation as a full-thickness tear. Secondly, it is possible that an additional small defect through the thin cuff not seen at arthroscopy is present. Both articular- and bursal-sided tears should be carefully inspected in arthroscopic examinations, as very often these represent full-thickness tears even if they do not appear so upon initial inspection (16).
Inter- and intra-observer agreement and kappa values were excellent in the diagnosis of articular-sided tear. In addition, both readers were confident in the diagnosis of articular-sided tears. The Kappa values indicated moderate inter-observer agreement in the diagnosis of bursal-sided tears, and only fair inter-observer agreement in both articular- and bursal-sided tears. Recently, Spencer et al. (19) have reported moderate agreement in predicting the involved side of partial-thickness tears and poor agreement in predicting the grade of tear in MR imaging.
With regard to bursal- and both articular- and bursal-sided tears, inter- and intra-observer agreement was lower than agreement of detection for articular-sided tears, suggesting that MR arthrography was a less objective interpretation. In addition, observers were less confident in the diagnosis of bursal- and both articular- and bursal-sided tears than articular-sided tears. The results of our study suggest that bursal- and both articular- and bursal-sided tears are also difficult to detect consistently with MR arthrography, in spite of the addition of a T2-weighted sequence. A more extensive study would be necessary to determine whether improvements in criteria, reader training, or MR imaging technique would improve the consistency of the diagnoses of bursal- and both articular- and bursal-sided tears. In contrast, the arthroscopic study showed excellent inter-observer agreement with regard to determining the side of involvement of partial-thickness tears (20). Therefore, a complete inspection of both articular and bursal surfaces of the cuff should be performed at arthroscopy, particularly if preoperative imaging indicates partial-thickness tears.
Our study had several limitations. Although arthroscopy was the best standard of reference, it was imperfect because it is an operator-dependent method. Arthroscopy has the potential to underestimate or overestimate tears, especially small partial-thickness tears and both articular- and bursal-sided tears. Findings at arthroscopy could have been biased by the availability of clinical MRI reports. Selection bias is also a limitation of this study. Only MR images in patients who later underwent surgery were included. Subjects were selected in such a way that there were approximately equal numbers of patents in the group of partial-thickness tears and the control group. This retrospective study was not concerned with the accuracy of identifying full-thickness tears, even though some of partial-thickness tears were misdiagnosed as full-thickness tears on MR arthrography.
In conclusion, MR arthrography is a useful diagnostic tool for partial-thickness rotator cuff tears, but has limitations in that it has low sensitivity in bursal- and both articular- and bursal-sided tears. Moreover, predicting both articular- and bursal-sided tears shows only fair inter-observer agreement.
Figures and Tables
Fig. 1
61-year-old man with articular-sided partial-thickness tear.
A. Fat-suppressed oblique coronal T1-weighted image shows defect along undersurface of supraspinatus tendon with no leakage of contrast medium into subacromial-subdeltoid bursa (arrow).
B. Fat-suppressed T1-weighted image with abduction external rotation position shows abnormal leakage of contrast medium with delaminating tendon (arrow).

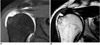
Fig. 2
47-year-old man with bursal-sided partial-thickness tear.
A. Fat-suppressed oblique coronal T1-weighted image shows that bursal surface of distal supraspinatus tendon is irregular (arrow), while articular surface is smooth. There was no contrast spilling within subacromial bursa.
B. Oblique coronal T2-weighted image shows irregular delineated high signal intensity area along bursal surface of supraspinatus tendon (arrow).

Fig. 3
46-year-old man with both articular- and bursal-sided partial-thickness tears.
A. Fat-suppressed oblique coronal T1-weighted image shows irregularity along articular surface of supraspinatus tendon (arrow), which represented articular-sided tear.
B. Oblique coronal T2-weighted image shows fluid signal in bursa with focal area of high signal intensity involving bursal surface (arrow), which is consistent with bursal-sided tear.

Fig. 4
53-year-old man with bursal-sided partial-thickness tear.
A, B. Oblique coronal fat-suppressed T1- and T2-weighted images show intact tendon. This was false-negative when compared to arthroscopy described as bursal-sided tear.

Fig. 5
62-year-old woman with both articular- and bursal-sided partial-thickness tears.
A, B. Oblique coronal fat-suppressed T1- and T2-weighted images show irregularity of undersurface of supraspinatus tendon with focal accumulation of contrast medium and smooth fat strip along bursal surface, which was interpreted as articular-sided tear. Corresponding arthroscopic record described both articular- and bursal-sided tears.
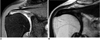
Fig. 6
54-year-old man with both articular- and bursal-sided partial-thickness tears.
A, B. Oblique coronal fat-suppressed T1- and T2-weighted images show defect of supraspinatus tendon and contrast leakage along subdeltoid-subacromial bursa, which was interpreted as full-thickness tear. Corresponding arthroscopic record described both articular- and bursal-sided tears.
References
1. Matava MJ, Purcell DB, Rudzki JR. Partial-thickness rotator cuff tears. Am J Sports Med. 2005. 33:1405–1417.
2. Finnan RP, Crosby LA. Partial-thickness rotator cuff tears. J Shoulder Elbow Surg. 2010. 19:609–616.
3. Meister K, Thesing J, Montgomery WJ, Indelicato PA, Walczak S, Fontenot W. MR arthrography of partial thickness tears of the undersurface of the rotator cuff: an arthroscopic correlation. Skeletal Radiol. 2004. 33:136–141.
4. Stetson WB, Phillips T, Deutsch A. The use of magnetic resonance arthrography to detect partial-thickness rotator cuff tears. J Bone Joint Surg Am. 2005. 87:81–88.
5. Waldt S, Bruegel M, Mueller D, Holzapfel K, Imhoff AB, Rummeny EJ, et al. Rotator cuff tears: assessment with MR arthrography in 275 patients with arthroscopic correlation. Eur Radiol. 2007. 17:491–498.
6. Robertson PL, Schweitzer ME, Mitchell DG, Schlesinger F, Epstein RE, Frieman BG, et al. Rotator cuff disorders: interobserver and intraobserver variation in diagnosis with MR imaging. Radiology. 1995. 194:831–835.
7. Ferrari FS, Governi S, Burresi F, Vigni F, Stefani P. Supraspinatus tendon tears: comparison of US and MR arthrography with surgical correlation. Eur Radiol. 2002. 12:1211–1217.
8. Magee T. 3-T MRI of the shoulder: is MR arthrography necessary? AJR Am J Roentgenol. 2009. 192:86–92.
9. Sano H, Ishii H, Trudel G, Uhthoff HK. Histologic evidence of degeneration at the insertion of 3 rotator cuff tendons: a comparative study with human cadaveric shoulders. J Shoulder Elbow Surg. 1999. 8:574–579.
10. Palmer WE. MR arthrography of the rotator cuff and labral-ligamentous complex. Semin Ultrasound CT MR. 1997. 18:278–290.
11. Vahlensieck M. MRI of the shoulder. Eur Radiol. 2000. 10:242–249.
12. Vanhoenacker FM, Van der Woude HJ, Vanhoenacker PK, De Praeter G. MR arthrography of the rotator cuff. JBR-BTR. 2007. 90:338–344.
13. Jung JY, Jee WH, Chun HJ, Ahn MI, Kim YS. Magnetic resonance arthrography including ABER view in diagnosing partial-thickness tears of the rotator cuff: accuracy, and inter- and intra-observer agreements. Acta Radiol. 2010. 51:194–201.
14. Schreinemachers SA, van der Hulst VP, Willems WJ, Bipat S, van der Woude HJ. Detection of partial-thickness supraspinatus tendon tears: is a single direct MR arthrography series in ABER position as accurate as conventional MR arthrography? Skeletal Radiol. 2009. 38:967–975.
15. Quinn SF, Sheley RC, Demlow TA, Szumowski J. Rotator cuff tendon tears: evaluation with fat-suppressed MR imaging with arthroscopic correlation in 100 patients. Radiology. 1995. 195:497–500.
16. McConville OR, Iannotti JP. Partial-thickness tears of the rotator cuff: evaluation and management. J Am Acad Orthop Surg. 1999. 7:32–43.
17. Magee T, Williams D. 3.0-T MRI of the supraspinatus tendon. AJR Am J Roentgenol. 2006. 187:881–888.
18. Ko JY, Huang CC, Chen WJ, Chen CE, Chen SH, Wang CJ. Pathogenesis of partial tear of the rotator cuff: a clinical and pathologic study. J Shoulder Elbow Surg. 2006. 15:271–278.
19. Spencer EE Jr, Dunn WR, Wright RW, Wolf BR, Spindler KP, McCarty E, et al. Interobserver agreement in the classification of rotator cuff tears using magnetic resonance imaging. Am J Sports Med. 2008. 36:99–103.
20. Kuhn JE, Dunn WR, Ma B, Wright RW, Jones G, Spencer EE, et al. Interobserver agreement in the classification of rotator cuff tears. Am J Sports Med. 2007. 35:437–441.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download