Abstract
Objective
To investigate the clinical feasibility of dual energy subtraction (DES) imaging to improve the delineation of the vocal cord and diagnostic accuracy of vocal cord paralysis as compared with the anterior-posterior view of flat panel detector (FPD) neck radiography.
Materials and Methods
For 122 consecutive patients who underwent both a flexible laryngoscopy and conventional/DES FPD radiography, three blinded readers retrospectively graded the radiographs during phonation and inspiration on a scale of 1 (poor) to 5 (excellent) for the delineation of the vocal cord, and in consensus, reviewed the diagnostic accuracy of vocal cord paralysis employing the laryngoscopy as the reference. We compared vocal cord delineation scores and accuracy of vocal cord paralysis diagnosis by both conventional and DES techniques using κ statistics and assessing the area under the receiver operating characteristic curve (AUC).
Results
Vocal cord delineation scores by DES (mean, 4.2 ± 0.4) were significantly higher than those by conventional imaging (mean, 3.3 ± 0.5) (p < 0.0001). Sensitivity for diagnosing vocal cord paralysis by the conventional technique was 25%, whereas the specificity was 94%. Sensitivity by DES was 75%, whereas the specificity was 96%. The diagnostic accuracy by DES was significantly superior (κ = 0.60, AUC = 0.909) to that by conventional technique (κ = 0.18, AUC = 0.852) (p = 0.038).
Vocal cord paralysis is a relatively common sign of disease, most commonly resulting from the paralysis of the recurrent laryngeal nerve. A paralysis of the recurrent nerve, serving as an adductor, most often leads to a paramedian position of the vocal cord. The symptoms include hoarseness, dysphonea, and dyspnea. Although the flexible laryngoscopy is currently the diagnostic modality of choice for vocal cord paralysis, there is issue with patient discomfort, intolerance to its insertion and the necessity of ear-nose-throat (ENT) specialists with sufficient experience and skills. Radiological examinations, including conventional laryngeal radiography, tomography, contrast laryngography, and computed tomography (CT) can overcome these disadvantages (1-5). The classic findings of vocal cord paralysis on these examinations are secondary to atrophy of the thyroarytenoid muscle (1-3). As the muscle atrophies, the cord becomes thinner and more pointed, with loss of the subglottic arch. As the muscle diminishes in size, the ventricle enlarges. The pyriform sinus also enlarges on the ipsilateral side. These changes in the shape of the vocal cord can be well visualized on coronal images that eliminate various shadows superimposed on the cord.
The dual energy subtraction (DES) technique has been applied to chest radiography, and has been demonstrated to improve the detection of pulmonary nodules by reducing overlying bony opacities (6, 7). This technique uses two different energy X-ray exposures, and produces an image of soft-tissue only, by exploiting the difference between the energy-dependent attenuation of bone and soft tissue to eliminate bone contrast. Likewise, overlapping cervical spine opacity often impairs the visualization of vocal cord shadow on the anterior-posterior (AP) view in laryngeal radiography. However, the DES technique can improve the delineation of the vocal cord and diagnostic accuracy of vocal cord paralysis by eliminating the bony opacity. Furthermore, DES laryngeal radiography easily allows for the evaluation of the vocal cord during phonation and inspiration since it involves a shorter examination time than tomography and no contrast medium is required to perform the laryngography. The lack of motion of the paralyzed vocal cord compared to the normal motion of the contralateral side can be seen by comparing laryngeal radiographs acquired during phonation and inspiration. In addition, the DES technique can improve the delineation of the pyriform sinus and subglottis, which, as mentioned above, should be thoroughly evaluated for the diagnosis of vocal cord paralysis.
Recently, radiography systems based on full-field, amorphous silicon, flat-panel cesium iodine, and amorphous silicon detectors, have become commercially available. These systems promise rapid access to the image for diagnosis, improved image quality relative to screen-film and storage phosphor systems, and the potential for reduced radiation exposure. The development of a fast, high-efficiency flat panel detector (FPD) enables the DES technique to be integrated into the traditional workflow. Furthermore, this system provides a high detective quantum efficiency for obtaining high quality images as well as reducing patient radiation dose. FPD chest radiography has been shown to enable a significant dose reduction compared to computed radiography or film-screen radiography systems (8-11). Specifically, image quality and visibility of the anatomic structures were comparable between those modalities, even if the radiation dose was approximately 50% with the FPD system. In addition, speed optimization can lead to the further dose reduction and decreased motion artifact. However, the DES technique using FPD, to our knowledge, has not been applied in laryngeal radiography.
The purpose of the present study was to investigate the clinical feasibility of DES using FPD to improve the delineation of the vocal cord, the pyriform sinus, and subglottis, as well as to determine the effect of eliminating the overlap of cervical spine opacities on the diagnostic accuracy of vocal cord paralysis on AP neck DES radiography compared to conventional FPD radiography, using flexible laryngoscopy results as the reference standard.
From April to December 2007, 122 consecutive patients (66 male, 56 female, mean age 59 ± 19 years, range 4-98 years) underwent an AP view of FPD laryngeal radiography, with and without DES, as well as a flexible laryngoscope examination at our institution. All of the patients visited the ENT department with the following chief complaints: abnormal throat sensation (n = 55), hoarseness (n =33), sore throat (n = 13), sleep apnea (n = 5), dyspnea (n = 4), cough (n = 3), sputum (n = 3), dysphagea (n = 2), neck pain (n = 2), dysphonea (n = 1), and neck swelling (n = 1). The radiographic examinations of each patient were performed on the same day as the assessment by ENT specialists at the department. We initially performed a retrospective evaluation of the radiographs, followed by a review of the medical records of these patients regarding their clinical information and results of the laryngoscope examination including vocal cord paralysis.
We obtained laryngeal radiographs using a FPD radiography system (Definium 8000, GE-Yokogawa Medical Systems, Tokyo, Japan). This system includes a cesium iodide scintillator and an amorphous silicon photodiode-transistor array. The detector has an image size of 41 × 41 cm and a pixel dimension of 0.2 × 0.2 mm. The DES technique included the standard digital AP radiograph and the soft-tissue only image. DES images were acquired using a dual-exposure method with less than 150 msec between the high- and low-energy exposures (12). The imaging parameters included a 140-kV image at a speed equivalent to approximately 250, and a 60-kV image at a speed equivalent of approximately 250. The radiation dose of the FPD radiography system at a speed of 250 is nearly equal to that of the computed radiography system.
Specifically, our radiology technicians first positioned the patients facing straight toward the X-ray tube in an upright position with their mandible upwards and neck extended. Second, the patients were directed to keep uttering 'eh' clearly and loudly, and acquired the dual energy high and low tube kilovoltage image pair successively during the sustained phonation. Third, the patients were directed to inhale from their nose with their mouth closed to once again successively acquire the dual energy high and low tube kilovoltage image pair during inspiration. Finally, after subtracting the image dual energy, we obtained, for each patient, a standard and a soft-tissue only image of the AP view of the larynx during phonation and inspiration. The standard and soft-tissue only images were printed using a laser imager (Dry Pix 7000, Fuji Film Medical, Tokyo, Japan). We regarded this standard image as a conventional radiograph. Three blinded readers retrospectively reviewed these images in this order for the delineation of the vocal cord, as well as for the pyriform sinus and subglottis using an independent grading scale from 1 (poor) to 5 (excellent) and, in consensus, the diagnosis of vocal cord paralysis was based on the following findings: 1) poor mobility of the paralyzed vocal cord, 2) thinning and pointing of the paralyzed vocal cord, 3) loss of the subglottic arch on the paralyzed side, 4) elevation of the paralyzed cord, and 5) enlargement of the ventricle and/or pyriform sinus on the paralyzed side using the laryngoscopy as a reference (1-3).
Data were expressed as the mean ± standard deviation (SD). We compared the delineation of vocal cord as well as the pyriform sinus and subglottis between the standard and the soft-tissue only image using the average delineation scale of each anatomy from the three readers, and performed by the Wilcoxon signed-ranks test to compare the results. We assessed inter-observer agreements of those delineation scales using Cohen's κ-statistics. We calculated the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of vocal cord paralysis diagnosis by both the conventional and DES techniques. We assessed the diagnostic accuracy of vocal cord paralysis by both images and quantified the diagnostic agreement between both the conventional and DES technique by using the laryngoscopy as the reference and using κ-statistics as well as the area under the receiver operating characteristic (ROC) curve (AUC) calculated with the dedicated software, ROCKIT (Metz CE, Department of Radiology, University of Chicago, IL) (13). A p value of less than 0.05 was regarded as statistically significant.
For none of the patients, was the scale of delineation of the vocal cord as well as the pyriform sinus and subglottis with the DES technique lower than with the conventional technique. The scale of delineation for each anatomy using both methods by each reader was summarized in Table 1. Those delineation scales showed no or only slight inter-observer agreements (Table 1).
The average of the delineation scale for the vocal cord with the DES technique (mean, 4.2 ± 0.4) was significantly higher than with the conventional technique (mean, 3.3 ± 0.5) (p < 0.0001) (Fig. 1). Furthermore, the average of the delineation scale for the pyriform sinus and subglottis with the DES technique (mean, 3.9 ± 0.4 and 4.4 ± 0.3) was significantly higher than with the conventional technique (mean, 2.9 ± 0.5 and 3.6 ± 0.4) (p < 0.0001), respectively (Fig. 1).
Vocal cord paralysis was confirmed in eight patients (7%) by laryngoscopy. The sensitivity of diagnosing vocal cord paralysis with the conventional technique was 25% (2/8), whereas the specificity was 94% (107/114), PPV was 22% (2/9), NPV was 95% (107/113), and the accuracy was 89% (109/122). The sensitivity of the DES technique was 75% (6/8), whereas the specificity was 96% (109/114), PPV was 55% (6/11), NPV was 98% (109/111), and the accuracy was 94% (115/122). The diagnostic accuracy was significantly better with the DES technique (κ = 0.60, AUC = 0.909), compared to the conventional technique (κ = 0.18, AUC = 0.852) (p = 0.038) (Fig. 2).
The results of the present study indicate that the DES technique is a feasible methodology for delineating the vocal cord in addition to the pyriform sinus and subglottis, and is more accurate for the diagnoses of vocal cord paralysis than the conventional technique for FPD neck radiography. The sensitivity of the diagnosis of vocal cord paralysis was greatly improved using the DES technique by dramatically eliminating the overlap of the cervical spine opacity. In particular, the DES technique may be more beneficial for patients with increased opacity of cervical spine due to cervical spondylosis. To the best of our knowledge, this is the first study that applied the DES technique for the diagnosis of vocal cord paralysis.
The decision on whether to include patients was based on the inclusion by ENT specialists at our department. For this patient population, the prevalence vocal cord paralysis was lower than expected, resulting in low PPV and relatively large 95% confidence intervals of the ROCs at low specificity (high [1-specificity]), even when using the DES technique. For this study, the diagnostic agreement of vocal cord paralysis between the DES technique and flexible laryngoscopy was moderate; five patients were false-positive and two were false-negative. For the five false-positive and two false-negative patients, the delineation rate of the vocal cord with the DES technique was sufficiently high, five for four false-positive and two false-negative patients, as well as four for one false-positive patient.
Based on the results, it seems that DES radiography may be less sensitive for patients with bilateral vocal cord paralysis and/or slight vocal cord atrophy. Merati and colleagues (14) described that bilateral involvement occurred in 11% of patients with newly diagnosed vocal cord motion impairment. However, no bilateral involvement of vocal cord paralysis was diagnosed by laryngoscopy in the present study. The amount of cord atrophy was directly related to the duration and degree of vocal cord paralysis. In both false-negative patients, vocal cord paralysis was transient based on the patient medical records. Moreover, no definite cord atrophy was noted by laryngoscopy. Whereas the vocal cord normally abducts during inspiration, the paralyzed vocal cord may take five positions, ranging from full or gentle abduction, to median, paramedian, or intermediate (15). The paramedian position is the most common position, but sometimes an intermediate position can be taken. The latter situation may degrade the diagnostic sensitivity of DES radiography since it does not allow direct dynamic observation of vocal cord mobility and mainly depends on the asymmetry in the position of the cord during phonation and inspiration. Both false-negative patients showed an intermediate position of the paralyzed vocal cord in the present study. Thus, the false-negative diagnosis for the DES technique was probably caused by no cord atrophy and an intermediate position of the paralyzed vocal cord, or otherwise might be due to inadequate timing exposure.
In contrast, the false-positive diagnosis might be due to physiological asymmetry of the vocal cord, slight oblique X-ray projections to the patients, or failed stable condition of the patients during the radiography examination, but was most likely to result from inadequate exposure timing. In particular, obtaining adequate exposure during inspiration sometimes can require high skill and experience of the radiology technicians for both conventional and DES methods; inadequate exposure during inspiration can be largely related to the diagnostic accuracy of vocal cord paralysis.
The advantages of the DES technique are that it can be easily and swiftly performed in the same examination time as conventional radiography. In addition, it was a less invasive technique that did not require highly skilled and experienced ENT specialists. This technique is especially useful for general physicians who examine patients presenting with a suspicion of vocal cord paralysis and could not undergo a laryngoscopic examination. Furthermore, the DES radiography can obtain images like pharyngolaryngography to evaluate the mucosal changes of the hypopharynx and larynx. As well, screening for extrinsic mass lesions can be assessed in the region to some extent, and DES can help delineate a wider field of view including the subglottic space that is difficult to assess by laryngoscopy. Although other radiological examinations for the evaluation of vocal cord paralysis include conventional radiography, tomography, contrast laryngography, and CT, DES FPD radiography readily enables this evaluation with greater diagnostic accuracy than conventional radiography, with a shorter examination time than tomography, without use of contrast medium necessary on laryngography, and with a much lower radiation dose than CT.
The use of a full-field FPD radiography system enables a fast dual-exposure technique to accurately perform the DES within the traditional workflow, and with a minimal radiation dose to the patient. Thus, given the improved diagnostic accuracy demonstrated by the DES method, the use of this FPD system and the optimization of acquisition parameters may justify the application of the DES technique to laryngeal radiography, since the clinical advantages of this examination outweigh the radiation exposure offset.
In contrast, the main disadvantages of the DES technique compared to the laryngoscopy includes the inability to assess the hue alterations and subtle morphological changes, as well as the small radiation dose rather than the inability to perform direct dynamic observation of vocal cord mobility. Furthermore, in many instances, CT is the imaging modality of choice for vocal cord paralysis because there are so many 'possibly serious' disease conditions that are not visible on laryngoscopy, conventional, or even DES radiography. Those conditions include a jugular fossa tumor, neck tumor, and aortopulmonary window lung cancer. This limits the usefulness of the DES technique. However, the DES radiography can be used for an initial imaging study for patients who are not able to undergo a CT or laryngoscopy.
In conclusion, by eliminating overlapping cervical spine opacity, the DES technique provides a better delineation of the vocal cord as well as the pyriform sinus and subglottis. It also provides a more accurate diagnosis of vocal cord paralysis than does the conventional FPD laryngeal radiography. A major limitation of the present study is the delineation scales for the anatomical features; both techniques showed no or only slight inter-observer agreement. That was presumably because the criteria of those delineation scales were not sufficiently thorough among our readers. In particular, one of those readers might have, in retrospect, lacked sufficient experience with the radiography of those regions. Nevertheless, this examination allows for an easy, swift, and noninvasive investigation of vocal cord paralysis in a routine workflow compared to the flexible laryngoscopy. Therefore, the DES technique is clinically feasible for the diagnosis of vocal cord paralysis, even in institutions without an ENT specialist. However, a further prospective investigation is suggested to increase the sample size for the results.
Figures and Tables
Fig. 1
Mean delineation scale scores for readers of pyriform sinus, subglottis, and vocal cord on conventional and dual energy subtraction radiographs. Scale of delineation with dual energy subtraction was significantly higher than with conventional technique for all these anatomical sites (p < 0.0001). Left bar: conventional method; Right bar: dual energy subtraction method. Number shown in each bar graph represents mean delineation scale of each anatomy ± estimated error of mean.
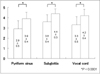
Fig. 2
Receiver operating characteristic curves for diagnosis of vocal cord paralysis by conventional (left) and dual energy subtraction (right) radiographs. Area under receiver operating characteristic curve value is shown for each technique. Area under receiver operating curve value with dual energy subtraction was significantly higher than for conventional technique (p = 0.038). On these curves, 95% confidence intervals were plotted as dotted curves. AUC = area under receiver operating characteristic curve.

Fig. 3
75-year-old man with left vocal cord paralysis. Delineation of vocal cord with dual energy subtraction (all readers grade 5) was rated higher than by conventional technique (grades 2, 2, and 3) by three readers. Left vocal cord (arrows) was fixed more definitely at midline on soft-tissue only image during inspiration using dual energy subtraction method. DES = dual energy subtraction

Fig. 4
64-year-old woman with left vocal cord paralysis. Delineation of vocal cord by dual energy subtraction (all readers grade 5) was rated higher than by conventional technique (grades 4, 4, and 5) by three readers. Left vocal cord (arrows) was thinner and more pointed with loss of left subglottic arch compared to contralateral side and visualized more definitively on soft-tissue only image during inspiration using dual energy subtraction method. DES = dual energy subtraction

Fig. 5
71-year-old man without vocal cord paralysis. Right vocal cord appeared fixed at paramedian position on soft-tissue only image during inspiration using dual energy subtraction method. However, laryngoscope examination revealed no vocal cord paralysis. We regarded this patient as false positive case.

Fig. 6
78-year-old woman with right vocal cord paralysis. Soft-tissue only images using dual energy subtraction method could not lead to diagnosis of vocal cord paralysis. However, laryngoscope examination revealed right vocal cord paralysis. We regarded this patient as false negative case.

References
1. Carderon R, Ceballos J, McGraw JP. Tomographic aspect of paralysis of the vocal cords. Radiology. 1954. 63:407–410.
2. Isshiki N, Ishikawa T. Diagnostic value of tomography in unilateral vocal cord paralysis. Laryngoscope. 1976. 86:1573–1578.
3. Agha FP. Recurrent laryngeal nerve paralysis: a laryngographic and computed tomographic study. Radiology. 1983. 148:149–155.
4. Yumoto E, Sanuki T, Hyodo M. Three dimensional endoscopic images of vocal fold paralysis by computed tomography. Arch Otolaryngol Head Neck Surg. 1999. 125:883–890.
5. Yumoto E, Oyamada Y, Nakano K, Nakayama Y, Yamashita Y. Three-dimensional characteristics of the larynx with immobile vocal fold. Arch Otolaryngol Head Neck Surg. 2004. 130:967–974.
6. Ricke J, Fishbach F, Freund T, Teichgräber U, Hänninen EL, Röttgen R, et al. Clinical results of CsI-detector-based dual-exposure dual energy in chest radiography. Eur Radiol. 2003. 13:2577–2582.
7. McAdams HP, Samei E, Dobbins J 3rd, Tourassi GD, Ravin CE. Recent advances in chest radiography. Radiology. 2006. 241:663–683.
8. Fink C, Hallscheidt PJ, Noeldge G, Kampschulte A, Radeleff B, Hosch WP, et al. Clinical comparative study with a large-area amorphous silicon flat-panel detector: image quality and visibility of anatomic structures on chest radiography. AJR Am J Roentgenol. 2002. 178:481–486.
9. Strotzer M, Gmeinwieser JK, Völk M, Fründ R, Seitz J, Feuerbach S. Detection of simulated chest lesions with normal and reduced radiation dose: comparison of conventional screen-film radiography and a flat-panel X-ray detector based on amorphous silicon. Invest Radiol. 1998. 33:98–103.
10. Bacher K, Smeets P, Bonnarens K, De Hauwere A, Verstraete K, Thierens H. Dose reduction in patients undergoing chest imaging: digital amorphous silicon flat-panel detector radiography versus conventional film-screen radiography and phosphor-based computed radiography. AJR Am J Roentgenol. 2003. 181:923–929.
11. Tagashira H, Arakawa K, Yoshimoto M, Mochizuki T, Murase K. Detectability of lung nodules using flat panel detector with dual energy subtraction by two shot method: evaluation by ROC method. Eur J Radiol. 2007. 64:279–284.
12. Sabol JM, Avinash GB, Nicolas F, Claus B, Zhao J, Dobbins JT III. Antonuk LE, Yaffe MJ, editors. Development and characterization of a dual-energy subtraction imaging system for chest radiography based on CsI: T1 amorphous silicon flat-panel technology. Medical Imaging 2002: physics of medical imaging -- proceedings. 2001. vol. 4320. Bellingham, WA: Society of Photo-Optical Instrumentation Engineers;399–408.
13. Metz CE, Herman BA, Shen JH. Maximum-likelihood estimation of receiver operating characteristic (ROC) curves from continuously-distributed data. Stat Med. 1998. 17:1033–1053.
14. Merati AL, Shemirani N, Smith TL, Toohill RJ. Changing trends in the nature of vocal fold motion impairment. Am J Otolaryngol. 2006. 27:106–108.
15. Hagan PJ. Vocal cord paralysis. Ann Otol Rhinol Laryngol. 1963. 72:206–222.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download