Abstract
We report here on a rare case of an ectopic pancreatic tissue in the anterior mediastinum. A 32-year-old woman without any symptoms was transferred to our hospital because of an abnormal large mediastinal shadow on her chest radiograph during a checkup. The computed tomography (CT) scan revealed a giant cystic-solid mass that measured 16 × 13 × 8 cm and it was located in the center of the anterior mediastinum and it symmetrically grew to two sides. On enhanced CT scans, the solid component of the mass showed marked enhancement. We performed total surgical resection of the mass and complete pancreatic tissues were verified on the pathological examination.
An ectopic pancreas is a rare congenital anomaly that is generally found in the gastrointestinal tract (1). An ectopic pancreas arising from the mediastinum is extremely rare. To the best of our knowledge, only 10 cases (1-9) of this kind of heterotopia have been reported in the English medical literature since it was first reported in 1957 by Shillitoe and Wilson (2). Furthermore, all the previously reported lesions were less than 13 cm in the maximal diameter and most of them grew to the side, and none of them had marked enhancement reported on contrast CT. Herein, we present a case of a mediastinal ectopic pancreas that was surgically and histologically proven to be different and have different CT findings from those in the previous reports.
A 32-year-old woman was transferred to our hospital for a giant tumor in the mediastinum, which was detected during a health checkup. She had no overt signs or symptoms and the results of the laboratory tests were unremarkable. The abdominal ultrasonography and electrocardiography were normal. The posteroanterior chest radiography (Fig. 1A) demonstrated a huge mediastinal shadow with well defined margins that extended to the two lung fields and there was no calcification and ossification. The pre-contrast CT scan revealed a giant cystic-solid mass that measured 16 × 13 × 8 cm and it was located in the center of the anterior mediastinum and it symmetrically grew toward the two lung fields; the mass was well-circumscribed and compressed next to the aorta and the superior vena cava. The cystic lesion with a mean CT attenuation value of 15 Hounsfield unit (HU) had a slightly thickened wall. Most of the solid components that were found in the backside of the mass obscured the aorta, superior vena cava and main pulmonary trunk, and the solid components had an inhomogeneous density with a mean CT attenuation value of 42 HU (Fig. 1B). On the post-contrast CT scan, the solid part demonstrated marked enhancement with a mean CT attenuation value of 130 HU and the cystic wall of the lesion showed moderate enhancement (Fig. 1C). A provisional diagnosis of cystic teratoma with cancerization was made. No metastatic lesions were found on the preoperative staging, and surgical exploration and resection were then performed.
The patient underwent a complete surgical resection of the giant mass via a median sternotomy. A mass posterior to the sternum and chest wall was observed in the anterior mediastinum. It had adhesions to the adjacent vascular structures and the mediastinal pleura. Pathological examination during the surgical procedure indicated no malignancy, and so no further dissection was performed. The gross pathology revealed a 16 × 13.5 × 7.8 cm cystic-solid mass, and about 1,500 ml of brownish, turbid fluid was found in the cyst. Microscopically, the solid components presented as complete pancreatic tissue with a normal acinar structure and islets of pancreas (Fig. 1D). Therefore, the pathologic diagnosis was an ectopic pancreas in the mediastinum with cystogenesis. Postoperatively, the patient recovered uneventfully and no recurrence or metastasis was found during the three months follow-up.
An ectopic pancreas is a rare congenital anomaly, and this is defined as an abnormal localization of a pancreas or isolated pancreas tissue that has no anatomic and vascular connection with the normal pancreas, and this is found on about 2% of all autopsies (3). Most ectopic pancreases are located in the gastrointestinal tract (1), yet they are occasionally encountered in other uncommon sites, including the mediastinum. The histogenesis of a mediastinal ectopic pancreas is currently not clear (4). There are two main theories on the embryogenesis of this anomalous development. The first theory is the pluripotent epithelial cells of the ventral primary foregut undergo abnormal differentiation, which can be called heteroplasia, and this may lead to the formation of ectopic pancreatic tissue in the mediastinum. The second theory is that some cells from the pancreatic bud may migrate and locate at a different site (1). Further studies on embryogenesis may shed light the ectopic localization of pancreatic tissue. The clinical presentations of these previously reported patients have been nonspecific, for example, short breath, high fever (5), chest pain (6-8) and no symptoms at all, and even pericardial effusions and tamponade by the cysts with rupture into the pericardium (7). According to the previous reports, the mediastinal ectopic pancreases have mostly occurred in young patients and the male-to-female ratio is approximately equal. The effective treatment for ectopic pancreas with symptoms is surgical resection. Tamura et al. (6) followed up a patient with a mediastinal ectopic pancreas for eight years after the operation, and no recurrence or metastasis was found. In our case, a 32-year-old woman without any symptoms had a large mass detected in the mediastinum on chest radiography that was done for a health checkup. After complete surgical resection, patient's prognosis was good and no recurrence or metastasis was found during three months of follow-up. The diagnosis of our patient's mediastinal ectopic pancreas depended mainly on its histologic appearance, and the patient was diagnosed after surgery. Pancreatic tissue with acinar structures and islets of pancreas tissue were present on the pathology exam.
The imaging findings of a mediastinal ectopic pancreas have rarely been described. The chest radiography shows a widened mediastinal shadow or a mediastinal mass. A mediastinal ectopic pancreas does have some common imaging features: all these lesions show a large cystic or cystic-solid mass (2-9) that can reach 12.5 cm in the maximal diameter (8). Most of the lesions are located in the anterior mediastinum (3-8) and they grow toward the right (8). The mass, when it is enlarged, will compress and invade the surrounding tissues and organs such as the cardiovascular system and pleura (7, 8). On contrast-enhanced CT, the cyst wall and the solid portion of the lesion show mild or moderate enhancement (7). Some of the interesting CT features of our giant cystic-solid mass in the center of the anterior mediastinum were its size: the mass was 16 cm at the maximal diameter and it symmetrically grew toward two sides, and there was especially remarkable enhancement of the solid ectopic pancreatic tissues, and these features were different from those of the previous reports.
The enhancement pattern closely depends on the histopathologic findings. It has been reported (10) that the complete type ectopic pancreases in the stomach were histopathologically similar to normal pancreas and they consisted mainly of pancreatic acini with the same histologic features as the normal pancreas, and they showed strong enhancement on post-contrast CT, while for those incomplete type that mainly consisted of ducts and hypertrophied muscle, the minor pancreatic acini component showed poor enhancement. Yet our case of ectopic pancreas was located in the anterior mediastinum, and according to the characteristic of an ectopic pancreas with strong enhancement on contrast CT and the complete pancreatic tissues seen on pathologic examination, it should be classified as the complete type. Additionally, a cystic lesion is often found in the mass, which may be caused by the increase of secretion and the reduced discharge. Based on the above analysis, we speculate that the large volume of cystic fluid in our case may be related to the normal secretary function of the complete type of ectopic pancreas.
Although there are certain characteristic CT findings of a mediastinal ectopic pancreas, the disease does not have specific clinical symptoms. So, we should pay attention to differentiate it from mediastinal tumors, and especially a cystic teratoma or a dermoid cyst. Teratoma is derived from pluripotent germ cells. The benign teratoma is often cystic, whereas the malignant one is usually solid. Because it has two or three blastodermal origins, there are many kinds of tissues in a teratoma, such as lipid, bone tissues, teeth and hair. Thus, we can make a final diagnosis of teratoma if we find these tissues in the tumor.
In summary, we have presented a rare case of a complete type ectopic pancreas that arose from the anterior mediastinum, and this mass was surgically and histologically proven to be an ectopic pancreas, and we have reviewed its imaging features. As seen in this case report, the clinical presentation and the CT findings for a giant cystic-solid mass and the solid component with strong enhancement of the CT scan are nonspecific, and they are similar to those of other common tumors such as cystic teratoma or dermoid cyst. Consequently, it is better for these patients to be managed by surgery, and a definite diagnosis will depend on the pathology report.
Figures and Tables
Fig. 1
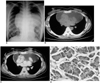
32-year-old woman without symptoms and who had mediastinal ectopic pancreas.
A. On posteroanterior chest radiography, huge shadow in mediastinum extends to two lung fields with well-defined margins.
B. Precontrast CT scan shows giant cystic-solid mass located in anterior mediastinum compresses next to aorta and superior vena cava, and solid lesion obscures aorta, superior vena cava and main pulmonary trunk.
C. On postcontrast CT scan, solid lesion demonstrates marked enhancement with mean CT attenuation value of 130 HU (arrow).
D. Solid lesion displays complete pancreatic tissues with normal acinar structures and islets of pancreas (Hematoxylin & Eosin staining; original magnification ×200).
References
1. von Schweinitz D, Wittekind C, Freihorst J. Mediastinal sequestration with ectopic pancreatic tissue. Z Kinderchir. 1990. 45:249–250.
2. Shillitoe AJ, Wilson JE. Enterogenous cyst of thorax with pancreatic tissue as a constituent. J Thorac Surg. 1957. 34:810–814.
3. Perez-Ordonez B, Wesson DE, Smith CR, Asa SL. A pancreatic cyst of the anterior mediastinum. Mod Pathol. 1996. 9:210–214.
4. Cagirici U, Ozbaran M, Veral A, Posacioglu H. Ectopic mediastinal pancreas. Eur J Cardiothorac Surg. 2001. 19:514–515.
5. Al-Salam S, Al Ashari M. Ectopic pancreatic tissue in the anterior mediastinum. Virchows Arch. 2006. 448:661–663.
6. Tamura Y, Takahama M, Kushibe K, Taniguchi S. Ectopic pancreas in the anterior mediastinum. Jpn J Thorac Cardiovasc Surg. 2005. 53:498–501.
7. Iglesias Sentis M, Belda Sanchis J, Gimferrer Garolera JM, Catalán Biela M, Rubio Garay M, Ramirez Ruz J. Mediastinal enteric cyst: unusual clinical presentation and histopathology. Arch Bronconeumol. 2004. 40:185–187.
8. Wang W, Li K, Qin W, Sun H, Zhao C. Ectopic pancreas in mediastinum: report of 2 cases and review of the literature. J Thorac Imaging. 2007. 22:256–258.
9. Carr MJ, Deiraniya AK, Judd PA. Mediastinal cyst containing mural pancreatic tissue. Thorax. 1977. 32:512–516.
10. Park SH, Han JK, Choi BI, Kim M, Kim YI, Yeon KM, et al. Heterotopic pancreas of the stomach: CT findings correlated with pathologic findings in six patients. Abdom Imaging. 2000. 25:119–123.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download