Neurosyphilis refers to an infection of the brain and spinal cord caused by a microorganism, a spirochete named Treponema pallidum that is transmitted during sexual intercourse. The infection can occur at any stage of the disease process and one third of patients in the tertiary stage develop neurosyphilis. The imaging findings of neurosyphilis vary and are most commonly presented as a cerebral infarction, nonspecific white matter lesions or meningitis (1, 2). We present a case of neurosyphilis with mesiotemporal involvement mimicking herpes simplex encephalitis or paraneoplastic limbic encephalitis. Although a few cases of mesiotemporal abnormalities in neurosyphilis have been reported, it is still a relatively rare finding and, to our knowledge, is the first in the radiology literature in Korea.
CASE REPORT
A previously healthy 35-year-old man visited our hospital with a 1-month history of short-term memory difficulties and disorientation. The patient had a history of alcohol abuse for one year and tobacco abuse for ten years. A general physical examination identified whitish patches and a fissured ulcer on the left lateral side of the patient's tongue. A punch biopsy was performed. In addition, a Mini-Mental State Examination score was 26/30 due to deficits in orientation, calculation and recall. A neurological examination revealed otherwise unremarkable findings. A lumbar puncture performed on the first day revealed 48 WBCs·mm-3 (92% lymphocytes) and elevated protein levels (88 mg·dL-1). Gram stain, KOH mount, India ink method and AFB stain did not reveal any organisms.
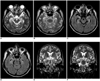
However, a brain MRI performed upon admission showed high signal changes in the bilateral mesial temporal lobes including both hippocampi and amygdalae on a spin echo (T2) and fluid-attenuated inversion recovery (FLAIR) sequences (Fig. 1). Diffusion weighted image (DWI) sequences revealed no definite abnormalities. In addition, no enhancement, evidence of areas of petechial hemorrhages or mass effect was noted. The patient was suspected of having herpes encephalitis, and was thus placed on acyclovir empirically. However, the cerebrospinal fluid (CSF) results of IgG, IgM and polymerase chain reaction (PCR) for herpes simplex virus were all negative. The CSF bacterial, fungal and AFB cultures revealed no growth. Subsequently, the results of the quantitative serum venereal disease research laboratory (VDRL) were 16.3 RU and found to be reactive. Further CSF analyses yielded repeated positive results for the CSF VDRL test (titer, 1:8) and the fluorescent treponemal antibody absorption (FTA-ABS) test. On the 7th day after admission, the result of the punch biopsy on the tongue was diagnosed as a syphilitic chancre, a characteristic skin lesion of primary syphilis. Consequently, the diagnosis of neurosyphilis was made and the treatment with penicillin was initiated. One month after the discharge, the patient returned for a follow-up evaluation and was found to have improved cognitive function.
DISCUSSION
Neurosyphilis is a slow progressive, destructive infection of the brain and spinal cord. It can occur at any stage of syphilis, although symptomatic early neurosyphilis is a rare manifestation (3). Most neurologic symptoms of early neurosyphilis result from acute or subacute meningitis, abnormalities in cranial nerve function and inflammatory vasculitis (3). The radiologic findings of neurosyphilis include cerebral infarctions (typically lacunar or middle cerebral artery in distribution) or nonspecific white matter lesions in meningovascular syphilis, cerebral gummas, or arteritis (1, 2). Cortical atrophy has been reported in patients with general paresis (1). In the present study, a MRI revealed high signal changes in the bilateral mesial temporal lobes, including both the hippocampi and amygdalae. Typically, these findings are considered as a characteristic radiologic manifestation of the herpes simplex encephalitis (4) or paraneoplastic limbic encephalitis (5). A few reports have described the mesiotemporal involvement in neurosyphilis (5-10). Similar to our case, Bash et al. (6) reported a patient with bilateral hyperintensity in the mesial temporal lobes on T2-weighted MR images. The authors found slight temporal lobe atrophy with compensatory dilation of the temporal horn after treatment. Another recent report by Vieira Santos et al. (7) presented a case showing a hyperintense signal on DWI and the high apparent diffusion coefficient (ADC) values, although DWI was not performed in our case.
The involvement of herpes simplex encephalitis initially tends to appear unilateral and is typically followed by contralateral disease. In addition, subtle temporal atrophy with slight enlargement of the temporal horns has been reported in neurosyphilis rather than the mild mass effect by profound cortical and subcortical edema in acute herpes simplex encephalitis (6). Furthermore, gyral enhancement and foci of subacute hemorrhage can be shown occasionally in herpes encephalitis cases (4). These imaging findings may be of help in distinguishing between neurosyphilis and herpes simplex encephalitis.
The etiology of signal change in the mesial temporal lobe is still uncertain. However, it is presumed that a combination of edema and gliosis related to the multiple mechanisms is responsible for the abnormality (6, 7). The authors suggest that the possible increase in the permeability of the blood-brain barrier, and meningeal inflammatory reaction from small vessel involvement lead to vasogenic edema and cytotoxic edema. They go on to describe that gliosis may be present as a secondary to infection-induced small-vessel ischemic changes.
Early diagnosis of neurosyphilis and appropriate antibiotic treatment make notable clinical improvement. However, the clinical diagnosis of neurosyphilis is often difficult because most patients are asymptomatic or present with nonspecific symptoms such as memory disturbance, disorientation, mental confusion, or seizures (6-10). An imaging diagnosis of neurosyphilis also may be challenging, because the radiographic manifestation of neurosyphilis is also nonspecific. Because syphilis serology is not routinely tested in patients with seizures or amnesia, radiologists should raise suspicion of neurosyphilis as well as herpes encephalitis or limbic encephalitis when mesiotemporal signal changes are seen on MRI.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download