Abstract
Objective
To evaluate the therapeutic efficacy of a new liquid embolic material, Embol, in embolization of the renal artery.
Materials and Methods
Embol is a new embolic material obtained by partial hydrolysis of polyvinyl acetate mixed in absolute ethanol and Iopromide 370 and manufactured by Schering Korea, Kyonggido, Korea. Six patients who underwent embolization of the renal artery using Embol were evaluated. Four were male and two were female and their ages ranged from 11 to 70 (mean, 53) years. Clinical and radiologic diagnoses referred for renal artery embolization were renal cell carcinoma (n = 3), renal angiomyolipoma (n = 2) and pseudoaneurysm of the renal artery (n = 1). After selective renal angiography, Embol was injected through various catheters, either with or without a balloon occlusion catheter. Changes in symptoms and blood chemistry which may have been related to renal artery embolization with Embol were analyzed.
Results
The six patients showed immediate total occlusion of their renal vascular lesions. One of the three in whom renal cell carcinoma was embolized with Embol underwent radical nephrectomy, and the specimen thus obtained revealed 40% tumor necrosis. In the two patients with angiomyolipomas, the tumors decreased in size and abdominal pain subsided. Bleeding from pseudoaneurysm of the renal artery was successfully controlled. Four patients showed symptoms of post-embolization syndrome, and one of these also showed increased levels of blood urea nitrogen and creatinine. One patient experienced transient hypertension.
Since the first introduction of percutaneous transcatheter renal artery embolization in 1964 (1), the devices used in interventional radiology have made rapid progress and super-selective catheterization is now possible. For successful renal artery embolization, both the selection of appropriate embolic material and adequate operator experience are prerequisites. The embolic materials used in renal vascular lesions include absolute ethanol, ethibloc, gelfoam, polyvinyl alcohol, coils and detachable balloons (2). Some of these are, however, hard to prepare and/or difficult to use in super-selective embolization and may result in incomplete occlusion and/or recanalization. Embol (Department of Biomedical Engineering, Seoul Health College, Kyonggido, Korea) is a new embolic material obtained by partial hydrolysis of polyvinyl acetate mixed in absolute ethanol and Iopromide 370, and manufactured by Schering Korea, Kyonggido, Korea. Portal vein embolization using Embol has been reported (3, 4). We describe the results of six cases of endovascular treatment for renal vascular lesions using this new liquid embolic material.
Embol is prepared in a polymerized state and is insoluble in water. When it comes into contact with blood, ethanol is washed out, resulting in precipitation of the embolic material and obstruction of the vessel. Partial hydrolysis of polyvinyl acetate increases the hydrophilic property of the polymer, making it soluble in a larger amount of angiographic contrast medium and increasing the radiopacity of the solution. We retrospectively reviewed the angiographic findings and medical records of six patients with renal vascular lesion who had undergone endovascular treatment with Embol. Four were male and two were female, and their ages ranged from 11 to 70 (mean, 53) years. Clinical or radiological diagnoses referred for endovascular treatment were renal cell carcinoma in three patients, angiomyolipoma in two and pseudoaneurysm of the renal artery with retroperitoneal hematoma which developed after renal biopsy in one. Analysis of adverse reactions resulting from renal artery embolization with Embol continued until the date of discharge.
For angiographic evaluation, percutaneous transfemoral catheterization using Seldinger s method was employed. Diagnostic aortography and selective renal angiography involved the use of a 5-Fr Cobra catheter (Cook, Bloomington, Ind.) and the digital subtraction technique. When the proximal main renal artery was embolized, an iliac sheath and balloon occlusion catheter were used to exclude possible regurgitation. In these cases, Embol was injected through the catheter. Where embolization was performed superselectively at the segmental artery, various coaxial catheters were used, without a balloon occlusion catheter. In one patient with pseudoaneurysm of the renal artery, stenosis of the proximal renal artery was combined and Embol was injected percutaneously under sonographic guidance.
After embolization, the catheter was flushed with 35% ethanol, and 15 to 20 minutes were allowed for Embol to precipitate. Post-embolization angiography was then performed. Patient characteristics and the devices used are summarized in Table 1.
In all cases the procedures were performed in a single step, and embolization was performed immediately after selective renal angiography. During embolization, Embol was clearly visualized fluoroscopically. Total occlusion of renal vascular lesions was achieved immediately in all six patients, although in one, a stainless steel coil (Cook, Bloomington, Ind.) was also used (Fig. 1). No renal parenchymal infarction was seen in non-embolized kidney segments.
One of the three patients with renal cell carcinoma (patient 1) underwent radical nephrectomy three days after embolization, and a pathologic specimen revealed 40% tumor necrosis. Nine months after surgery, this patient was doing well, without tumor recurrence (Fig. 1). One patient with renal cell carcinoma (patient 2) refused further treatment and was discharged, but was still alive six months after embolization. The one remaining patient with advanced renal cell carcinoma (T4) at the time of diagnosis (patient 3) expired three months after embolization due to deterioration in his general condition. In both patients with angiomyolipoma, right lower quadrant abdominal pain was successfully controlled. Follow-up sonography revealed that the angiomyolipomas had decreased in size from 7.5 to 6 cm in one patient (Fig. 2) and from 3.1 to 2.3 cm in the other. In the patient with pseudoaneurysm of the renal artery and retroperitoneal hematoma, bleeding stopped immediately after embolization. Serial follow-up sonograms indicated that retroperitoneal hematoma resolved gradually and no recurrent pseudoaneurysm was found (Fig. 3).
Elevated blood urea nitrogen and creatinine levels were seen after embolization in one patient with renal cell carcinoma (patient 2). This patient refused further treatment, however, and was discharged. The patient with pseudoaneurysm of the renal artery (patient 6) experienced renal failure before embolization and had elevated levels of blood urea nitrogen and creatinine, though no changes in these were observed before or after embolization. Transient elevated blood pressure was also seen in this patient, but the pressure decreased to normal within three days, without medication. Post-embolization syndrome of fever, nausea, vomiting, flank pain and/or leukocytosis occurred in four of six patients (Table 2). At the end of the procedure, transtumoral shunting of Embol to the renal vein occurred in one patient (patient 3) with advanced renal cell carcinoma (T4). Embolization was stopped immediately and balloon occlusion of the proximal renal artery was performed. Follow-up chest radiographs revealed no subjective chest symptoms or consolidation.
Since Edling first introduced renal artery embolization in 1964 (1), the applications of renal intervention have rapidly extended. Current indications for transcatheter renal artery embolization include hemorrhage resulting from trauma or renal tumor, renal arteriovenous malformation, end-stage renal disease, severe hypertension refractory to other methods of treatment, and recurrent infected hydronephrosis in a hemophilic patient (5).
There is little support for routine embolization of renal cell carcinoma during the immediate preoperative period (2, 6, 7). It is, rather, performed for conservative purposes in cases of solitary kidney, bilateral tumors, inoperable cases and tumor bleeding. Indications for the embolization of angiomyolipomas are a tumor larger than 4 cm or any tumor with continuous symptoms (8, 9). Renal arteriovenous fistulas and pseudoaneurysms are common complications occuring at a rate of 0.2 to 2% after renal biopsy (10), and for these lesions, transscatheter embolization is an effective method of treatment (10, 11). In all our cases, Embol was also effective, providing immediate total occlusion of the renal vascular lesion.
The development of co-axial catheters has facilitated super-selective embolization, with less trauma to unwanted segments of renal parenchyma (12). In addition, newer embolic materials are still being developed and tested (3, 4, 13-16). Embolic materials used in renal vascular lesions include absolute ethanol, ethibloc, gelfoam, polyvinyl alcohol, isobutyl-2-cyanoacrylate, coils, detachable balloons and autologous tissues. Some of these materials, however, involve tedious preparation, unequal suspension, high friction, difficulty in injecting through a microcatheter, incomplete occlusion and recanalization. Since the beginning of the 1980s, absolute ethanol or a mixture of absolute ethanol and oidized oil has been the recommended agent for embolization of renal vascular lesions (2, 7, 9). Absolute ethanol is fluoroscopically radiolucent, and unintentional embolization of non-target organs can occur. Embol, on the other hand, is radiopaque and unintentional embolization of the non-target organs can be prevented. Intratumoral arteriovenous shunt occurred in our series, at the end of the procedure, in a patient with renal cell carcinoma. Embolization was stopped immediately and balloon occlusion of the proximal renal artery was performed. After embolization, no pulmonary complication was noted either clinically or on chest radiographs.
A demerits noted during embolization with Embol is its high viscosity, and high pressure is thus required for injection, especially when coaxial microcatheters are used. In addition, there is a waiting time of 15 to 20 minutes for Embol to precipitate, and persistent pain occurs during embolization, though this is less than when absolute alcohol is used. A further disadvantage of Embol is the fact that it is difficult to ascertain the exact point before termination of the procedure at which precipitation actually occurs.
The reported complications of renal artery embolization include renal failure, post-infarction syndrome, gas formation in necrotic tissue and unintentional embolization of non-target organs (5, 17). Post-infarction syndrome was seen in four of six patients in our study, but the symptoms subsided with conservative care.
In conclusion, Embol is an effective embolic material which offers immediate and total occlusion of renal vascular lesions. It also appears to be safe to use, since it is adequately radiopaque during embolization, and no significant changes in blood pressure, body temperature, or blood urea nitrogen and creatinine levels occur after embolization. To avoid reflux of Embol to non-target organs, balloon occlusion catheters should be used during embolization of the proximal main renal artery. When embolization is performed after super-selection of the segmental branch, balloon occlusion will not be necessary.
Figures and Tables
Fig. 1
A 46-year-old female with renal cell carcinoma.
A. CT scan of the kidneys shows a huge heterogeneous mass replacing almost the entire right kidney, with thrombosis of the renal vein and inferior vena cava.
B. After balloon occlusion, 10 mL of Embol was injected into the proximal right renal artery. Stainless steel coil embolization was also performed.
C. Post-embolization aortogram reveals occlusion of the right renal artery.
Fig. 2
A 66-year-old male with angiomyolipoma.
A. CT scan shows a huge fatty mass, 7.5 cm in diameter, at the inferior pole of the right kidney.
B. Selective renal angiogram shows a hypervascular mass supplied from the inferior segmental branch of the right kidney. Using a Cobra catheter, 2.5 mL of Embol was injected.
C. Near-total occlusion of renal arterial branches supplying the angiomyolipoma is seen.

Fig. 3
An 11-year-old male with pseudoaneurysm of the renal artery after renal biopsy.
A. CT scan shows retroperitoneal hematoma with anteriorly displaced left kidney.
B. Selective renal angiogram shows pseudoaneurysm of the inferior segmental branch of the left kidney, about 1 cm in size. Stenosis of approximately 45% at the proximal side of the inferior segmental branch, with post-stenotic dilatation, is also seen.
C. Under sonographic guidance, the pseudoaneurysm was directly punctured with a 22-gauge biopsy needle. Five mL of Embol was injected.
D. The pseudoaneurysm was occluded.
Table 2
Adverse Reactions After Embolization with Embol
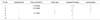
Note.-Patient numbers are the same as in Table 1
References
1. Edling NP, Ovenfors CO. Interventional embolization in selective renal arteriography: an experimental study in dogs. Acta Radiol Diagn. 1964. 2:316–320.
2. Kalman D, Varenhorst E. The role of arterial embolization in renal cell carcinoma. Scand J Urol Nephrol. 1999. 33:162–170.
3. Sung KB, Park SS, Yoon HK, et al. Study on effectiveness and safety of portal vein embolization using a new liquid embolic material (Embol-78-12) in pigs. J Korean Radiol Soc. 1999. 40:237–246.
4. Park SS, Yoon HK, Lee NS, et al. Portal vein embolization with use of a new liquid embolic material: An experimental study. J Vasc Interv Radiol. 1999. 10:339–345.
5. Segni RD, Young AT, Qian Z, Castaneda-Zuniga WR. Castaneda-Zuniga WR, Tadavarthy SM, Qian Z, Ferral H, Maynar M, editors. Embolotherapy: agents, equipment, and techniques. Interventional radiology. 1997. Baltimore: Williams and Wilkins;29–103.
6. Lanigan D, Jurriaans E, Hammonds JC, Wells IP, Choa RG. The current status of embolization in renal cell carcinoma-A survey of local and national practice. Clin Radiol. 1992. 46:176–178.
7. Park JH, Kim SH, Han JK, Chung JW, Han MC. Transcatheter arterial embolization of unresectable renal cell carcinoma with a mixture of ethanol and iodized oil. Cardiovasc Intervent Radiol. 1994. 17:323–327.
8. Dickinson M, Ruckle H, Beaghler M, Hadley HR. Renal Angiomyolipoma: Optimal treatment based on size and symptoms. Clin Nephrol. 1998. 49:281–286.
9. Lee W, Kim TS, Chung JW, Han JK, Kim SH, Park JH. Renal angiomyolipoma: Embolotherapy with a mixture of alcohol and iodized oil. J Vasc Interv Radiol. 1998. 9:255–261.
10. Perini S, Gordon RL, LaBerge JM, et al. Transcatheter embolization of biopsy-related vascular injury in the transplanted kidney: Immediate and long-term outcome. J Vasc Interv Radiol. 1998. 9:1011–1019.
11. Phadke RV, Sawlani V, Rastogi H, et al. Iatrogenic renal vascular injuries and their radiological management. Clin Radiol. 1997. 52:119–123.
12. Beaujeux R, Saussine C, Al-Fakir A, et al. Superselective endovascular treatment of renal vascular lesions. J Urol. 1995. 153:14–17.
13. Sadato A, Taki W, Ikada Y, et al. Experimental study and clinical use of polyvinyl acetate emulsion as liquid embolisation material. Neuroradiology. 1994. 36:634–641.
14. Hamada J, Ushio Y, Kazekawa K, Tsukahara T, Hashimoto N, Iwata H. Embolization with cellulose porous beads, I: An experimental study. Am J Neuroradiol. 1996. 17:1895–1899.
15. Miller DL, Bacher JD, O'Leary TJ, Maxwell M. Comparison of hot contrast material and hot saline for renal ablation in a canine model. Invest Radiol. 1986. 21:56–63.
16. Irie T, Kusano S. Fragmented platinum microcoils as embolization material. Acta Radiol. 1996. 37:696–699.
17. Lammer J, Justich E, Schreyer H, Pettek R. Complications of renal tumor embolization. Cardiovasc Intervent Radiol. 1985. 8:31–35.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download