1. Zachos NC, Tse M, Donowitz M. Molecular physiology of intestinal Na
+/H
+ exchange. Annu Rev Physiol. 2005; 67:411–443. PMID:
15709964.
2. Fliegel L. The Na
+/H
+ exchanger isoform 1. Int J Biochem Cell Biol. 2005; 37:33–37. PMID:
15381146.
3. Schultheis PJ, Clarke LL, Meneton P, Miller ML, Soleimani M, Gawenis LR, Riddle TM, Duffy JJ, Doetschman T, Wang T, Giebisch G, Aronson PS, Lorenz JN, Shull GE. Renal and intestinal absorptive defects in mice lacking the NHE3 Na
+/H
+ exchanger. Nat Genet. 1998; 19:282–285. PMID:
9662405.
4. Aronson PS. Ion exchangers mediating NaCl transport in the renal proximal tubule. Cell Biochem Biophys. 2002; 36:147–153. PMID:
12139400.

5. Woo AL, Noonan WT, Schultheis PJ, Neumann JC, Manning PA, Lorenz JN, Shull GE. Renal function in NHE3-deficient mice with transgenic rescue of small intestinal absorptive defect. Am J Physiol Renal Physiol. 2003; 284:F1190–F1198. PMID:
12582007.
6. Baum M, Martin MG, Booth IW, Holmberg C, Twombley K, Zhang Q, Gattineni J, Moe O. Nucleotide sequence of the Na
+/H
+ exchanger-8 in patients with congenital sodium diarrhea. J Pediatr Gastroenterol Nutr. 2011; 53:474–477. PMID:
21666503.
7. Xu H, Chen R, Ghishan FK. Subcloning, localization, and expression of the rat intestinal sodium-hydrogen exchanger isoform 8. Am J Physiol Gastrointest Liver Physiol. 2005; 289:G36–G41. PMID:
15731506.

8. Xu H, Li J, Chen R, Zhang B, Wang C, King N, Chen H, Ghishan FK. NHE2X3 DKO mice exhibit gender-specific NHE8 compensation. Am J Physiol Gastrointest Liver Physiol. 2011; 300:G647–G653. PMID:
21252044.

9. Wang A, Li J, Zhao Y, Johansson ME, Xu H, Ghishan FK. Loss of NHE8 expression impairs intestinal mucosal integrity. Am J Physiol Gastrointest Liver Physiol. 2015; 309:G855–G864. PMID:
26505975.

10. Xu H, Li J, Chen H, Wang C, Ghishan FK. NHE8 plays important roles in gastric mucosal protection. Am J Physiol Gastrointest Liver Physiol. 2013; 304:G257–G261. PMID:
23220221.

11. Liu C, Xu H, Zhang B, Johansson ME, Li J, Hansson GC, Ghishan FK. NHE8 plays an important role in mucosal protection via its effect on bacterial adhesion. Am J Physiol Cell Physiol. 2013; 305:C121–C128. PMID:
23657568.

12. Li X, Cai L, Xu H, Geng C, Lu J, Tao L, Sun D, Ghishan FK, Wang C. Somatostatin regulates NHE8 protein expression via the ERK1/2 MAPK pathway in DSS-induced colitis mice. Am J Physiol Gastrointest Liver Physiol. 2016; 311:G954–G963. PMID:
27686614.

13. Payne CM, Fass R, Bernstein H, Giron J, Bernstein C, Dvorak K, Garewal H. Pathogenesis of diarrhea in the adult: diagnostic challenges and life-threatening conditions. Eur J Gastroenterol Hepatol. 2006; 18:1047–1051. PMID:
16957509.

14. Cuevas-Ramos D, Fleseriu M. Somatostatin receptor ligands and resistance to treatment in pituitary adenomas. J Mol Endocrinol. 2014; 52:R223–R240. PMID:
24647046.

15. Pai V, Porter K, Ranalli M. Octreotide acetate is efficacious and safe in children for treating diarrhea due to chemotherapy but not acute graft versus host disease. Pediatr Blood Cancer. 2011; 56:45–49. PMID:
21108438.

16. Szilagyi A, Shrier I. Systematic review: the use of somatostatin or octreotide in refractory diarrhoea. Aliment Pharmacol Ther. 2001; 15:1889–1897. PMID:
11736719.

17. Li X, Wang Q, Xu H, Tao L, Lu J, Cai L, Wang C. Somatostatin regulates tight junction proteins expression in colitis mice. Int J Clin Exp Pathol. 2014; 7:2153–2162. PMID:
24966923.
18. Boshuizen JA, Reimerink JH, Korteland-van Male AM, van Ham VJ, Koopmans MP, Büller HA, Dekker J, Einerhand AW. Changes in small intestinal homeostasis, morphology, and gene expression during rotavirus infection of infant mice. J Virol. 2003; 77:13005–13016. PMID:
14645557.
19. Hainzl E, Stockinger S, Rauch I, Heider S, Berry D, Lassnig C, Schwab C, Rosebrock F, Milinovich G, Schlederer M, Wagner M, Schleper C, Loy A, Urich T, Kenner L, Han X, Decker T, Strobl B, Müller M. Intestinal epithelial cell tyrosine kinase 2 transduces IL-22 signals to protect from acute colitis. J Immunol. 2015; 195:5011–5024. PMID:
26432894.

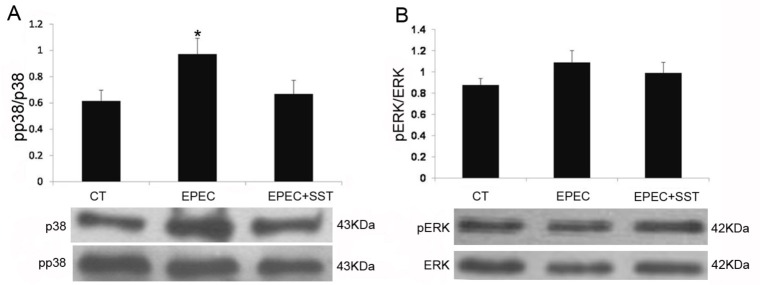
20. Wang C, Xu H, Chen H, Li J, Zhang B, Tang C, Ghishan FK. Somatostatin stimulates intestinal NHE8 expression via p38 MAPK pathway. Am J Physiol Cell Physiol. 2011; 300:C375–C382. PMID:
21106692.

21. Li X, Cai L, Xu H, Geng C, Lu J, Tao L, Sun D, Ghishan FK, Wang C. Somatostatin regulates NHE8 protein expression via the ERK1/2 MAPK pathway in DSS-induced colitis mice. Am J Physiol Gastrointest Liver Physiol. 2016; 311:G954–G963. PMID:
27686614.

22. Sandle GI. Infective and inflammatory diarrhoea: mechanisms and opportunities for novel therapies. Curr Opin Pharmacol. 2011; 11:634–639. PMID:
21983454.

23. Hecht G, Hodges K, Gill RK, Kear F, Tyagi S, Malakooti J, Ramaswamy K, Dudeja PK. Differential regulation of Na
+/H
+ exchange isoform activities by enteropathogenic E. coli in human intestinal epithelial cells. Am J Physiol Gastrointest Liver Physiol. 2004; 287:G370–G378. PMID:
15075254.
24. Collins JW, Keeney KM, Crepin VF, Rathinam VA, Fitzgerald KA, Finlay BB, Frankel G. Citrobacter rodentium: infection, inflammation and the microbiota. Nat Rev Microbiol. 2014; 12:612–623. PMID:
25088150.

25. O'Hara JR, Skinn AC, MacNaughton WK, Sherman PM, Sharkey KA. Consequences of Citrobacter rodentium infection on enteroendocrine cells and the enteric nervous system in the mouse colon. Cell Microbiol. 2006; 8:646–660. PMID:
16548890.
26. Eliakim R, Karmeli F, Okon E, Rachmilewitz D. Octreotide effectively decreases mucosal damage in experimental colitis. Gut. 1993; 34:264–269. PMID:
8381760.

27. van Bergeijk JD, Wilson JH. Somatostatin in inflammatory bowel disease. Mediators Inflamm. 1997; 6:303–309. PMID:
18472863.

28. McKeen ES, Feniuk W, Humphrey PP. Somatostatin receptors mediating inhibition of basal and stimulated electrogenic ion transport in rat isolated distal colonic mucosa. Naunyn Schmiedebergs Arch Pharmacol. 1995; 352:402–411. PMID:
8532068.

29. Warhurst G, Barbezat GO, Higgs NB, Reyl-Desmars F, Lewin MJ, Coy DH, Ross I, Grigor MR. Expression of somatostatin receptor genes and their role in inhibiting Cl-secretion in HT-29cl.19A colonocytes. Am J Physiol. 1995; 269:G729–G736. PMID:
7491965.
30. Ayiomamitis GD, Notas G, Zaravinos A, Drygiannakis I, Georgiadou M, Sfakianaki O, Mastrodimou N, Thermos K, Kouroumalis E. Effects of octreotide and insulin on colon cancer cellular proliferation and correlation with hTERT activity. Oncoscience. 2014; 1:457–467. PMID:
25594044.

31. Saksena S, Theegala S, Bansal N, Gill RK, Tyagi S, Alrefai WA, Ramaswamy K, Dudeja PK. Mechanisms underlying modulation of monocarboxylate transporter 1 (MCT1) by somatostatin in human intestinal epithelial cells. Am J Physiol Gastrointest Liver Physiol. 2009; 297:G878–G885. PMID:
20501436.

32. Hope N, Butt G, Ross I, Warhurst G, Arn M, Grigor M, Lubcke R, Barbezat GO. Somatostatin enhances cAMP-dependent shortcircuit current in human colon via somatostatin receptor subtype-2. Dig Dis Sci. 2001; 46:2499–2503. PMID:
11713960.
33. Warhurst G, Higgs NB, Fakhoury H, Warhurst AC, Garde J, Coy DH. Somatostatin receptor subtype 2 mediates somatostatin inhibition of ion secretion in rat distal colon. Gastroenterology. 1996; 111:325–333. PMID:
8690197.

34. O'Neill LA. Targeting signal transduction as a strategy to treat inflammatory diseases. Nat Rev Drug Discov. 2006; 5:549–563. PMID:
16773072.
35. Chang JP, Habibi HR, Yu Y, Moussavi M, Grey CL, Pemberton JG. Calcium and other signalling pathways in neuroendocrine regulation of somatotroph functions. Cell Calcium. 2012; 51:240–252. PMID:
22137240.

36. Ben-Shlomo A, Pichurin O, Barshop NJ, Wawrowsky KA, Taylor J, Culler MD, Chesnokova V, Liu NA, Melmed S. Selective regulation of somatostatin receptor subtype signaling: evidence for constitutive receptor activation. Mol Endocrinol. 2007; 21:2565–2578. PMID:
17609435.

37. Czerucka D, Dahan S, Mograbi B, Rossi B, Rampal P. Implication of mitogen-activated protein kinases in T84 cell responses to enteropathogenic Escherichia coli infection. Infect Immun. 2001; 69:1298–1305. PMID:
11179291.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download