Abstract
Vasoconstrictive properties of sympathomimetic drugs are the basis of their widespread use as decongestants and possible source of adverse responses. Insufficiently substantiated practice of combining decongestants in some marketed preparations, such are those containing phenylephrine and lerimazoline, may affect the overall contractile activity, and thus their therapeutic utility. This study aimed to examine the interaction between lerimazoline and phenylephrine in isolated rat aortic rings, and also to assess the substrate of the obtained lerimazoline-induced attenuation of phenylephrine contraction. Namely, while lower concentrations of lerimazoline (10−6 M and especially 10−7 M) expectedly tended to potentiate the phenylephrine-induced contractions, lerimazoline in higher concentrations (10−4 M and above) unexpectedly and profoundly depleted the phenylephrine concentration-response curve. Suppression of NO with NO synthase (NOS) inhibitor Nw-nitro-L-arginine methyl ester (L-NAME; 10−4 M) or NO scavanger OHB12 (10−3 M), as well as non-specific inhibition of K+-channels with tetraethylammonium (TEA; 10−3 M), have reversed lerimazoline-induced relaxation of phenylephrine contractions, while cyclooxygenase inhibitor indomethacin (10−5 M) did not affect the interaction between two vasoconstrictors. At the receptor level, non-selective 5-HT receptor antagonist methiothepin reversed the attenuating effect of lerimazoline on phenylephrine contraction when applied at 3×10−7 and 10−6 M, but not at the highest concentration (10−4 M). Neither the 5-HT1D-receptor selective antagonist BRL 15572 (10−6 M) nor 5-HT7 receptor selective antagonist SB 269970 (10−6 M) affected the lerimazoline-induced attenuation of phenylephrine activity. The mechanism of lerimazoline-induced suppression of phenylephrine contractions may involve potentiation of activity of NO and K+-channels and activation of some methiothepin-sensitive receptors, possibly of the 5-HT2B subtype.
Decongestant drugs generally serve as the first-line treatment for nasal congestion and all have α-adrenoceptor agonist, i.e. sympathomimetic activity. They are marketed as topical and oral formulations, aimed to relieve the symptom of nasal congestion, commonly seen in upper respiratory viral infections (common cold), allergic rhinitis, vasomotor rhinitis and chronic sinusitis. Protracted nasal congestion, if untreated, can lead to sequelae such as sinusitis or otitis media. Symptoms of nasal congestion, especially if associated with vasomotor rhinitis and the common cold, can be relieved by the short-term use (usually not longer than 5~7 days) of decongestant nasal drops and sprays. It is emphasized in the literature that their clinical applicability in states that need prolonged administration is limited due to possibility of rebound congestion (rhinitis medicamentosa) on withdrawal [1].
Phenylephrine is an efficacious α1 receptor adrenergic agonist widely used as a nasal decongestant, where its utility has been attributed to α1 adrenergic receptor-mediated vasoconstriction in nasal mucosa. This sympathomimetic agent is a synthetic selective α1-adrenergic agonist with mainly direct rather than indirect effects on adrenergic receptors. It was shown that the α1-adrenoceptor subtype mediating contraction to phenylephrine in rabbit corpus cavernosum has the characteristics of the α1B-adrenoceptor subtype [2]. On the other hand, the results from another study, performed by use of antagonists which in binding studies show selectivity between the cloned α1-adrenoceptor subtypes, suggest that the contraction to phenylephrine of the rat thoracic aorta, mesenteric artery and pulmonary artery are mediated in part via the α1D-subtype of adrenoceptors [3]. Finally, in a similarly designed experiment, it appeared that phenylephrine actions in the model of the rabbit cavernous artery may be antagonized only by an α1A-adrenergic receptor blocker, suggesting that the predominant α1-adrenoceptor subtype involved in vasoconstriction of penile arteries was the α1A-adrenoceptor [4]. From these pieces of evidence it may be concluded that all subtypes of the α1 adrenergic receptor may contribute to vascular effects of phenylephrine.
Lerimazoline is a congener of oxymetazoline and xylometazoline which has been used in combination with phenylephrine in nasal decongestant preparations for half a century [5]. The pharmacological profile of this compound, reported earlier as St-71, trimizoline or trimazoline, is not sufficiently elucidated in the present literature [678]. It has been known for some time that lerimazoline possesses a substantial affinity for 5-HT1D, and much less for 5-HT1B receptors (Ki values 72 vs. 3480 nM) [9]; more recently, it was found that it also demonstrates a high affinity for 5-HT1A receptor (Ki=162.5 nM), while binding affinity estimates (Ki) for α1, 5-HT2A and D2 receptors were 6656, 4202 and 3437.5 nM, respectively [Rizvic et al., manuscript in preparation]. When evaluated for contractile activity in the rings of rabbit saphenous vein pretreated with all, prazosin, idazoxan and indomethacin, in order to exclude possible adrenergic α1, α2 or prostaglandin-mediated effects, respectively, EC50 of lerimazoline (150 nM) was similar to that of the 5-HT1B/D receptor agonist sumatriptan used as the positive control (EC50=220 nM) [9]. As it was shown that the rabbit saphenous vein did not functionally contract to 5-HT1D receptor activation, while the high-affinity 5-HT1B receptor antagonist displayed surmountable antagonism of the contractile effects of sumatriptan [10], it can be indirectly concluded that contractile action of lerimazoline in that blood vessel should arise from activation of 5-HT1B receptors. On the other hand, our recent results suggested that the lerimazoline-induced contractions in rat thoracic aorta, that varied in the range 40~55% of the contractions elicited by 10−4 M phenylephrine, may be mediated mainly through non-α1 adrenergic receptors, possibly of the 5-HT2A subtype [Rizvic et al., manuscript in preparation], making it ‘an atypical decongestant’.
Such results were an impetus for assessment of the possible influences of lerimazoline on the contractile activity of phenylephrine, with a remote translational hypothesis that an interaction between these two vasoconstrictor agents, if revealed, may be useful in order to overcome rebound congestion seen on withdrawal of decongestants administered as single agents. We opted to study the putative interaction in the well-validated [11], and in our previous experiments with lerimazoline already used rat aorta preparation, having in mind the recognized variability of agonist-induced actions in different vascular beds of rats, which depend on concentrations tested, type of receptor involved, basal vascular tone, vascular bed analyzed and the presence of possible pathological processes [121314].
Aorta segments were taken from portions of 250~350 g weighing Wistar rats thoracic aorta, obtained from Military farm, Belgrade, Serbia. During treatment, rats were housed in clean transparent plastic cages with free access to tap water and pelleted food and kept in a conventional animal facility at a temperature of 22±1℃, relative humidity of 40~70% and the 12/12 h light/dark period, with lights on from 06:00. The animal study was performed after receiving approval of the Institutional Animal Care and Use Committee (approval No. 323-07-09231/2016-05/4, issued by the Veterinary Administration of the Republic of Serbia).
Methiothepin hydrochloride (non-selective 5-HT antagonist), indomethacin hydrochloride (cyclooxygenase inhibitor), tetraethylammonium (TEA, the nonspecific K+ channel blockers), L-NAME (nonspecific NOS inhibitor Nw-nitro-L-arginine methyl ester) and prazosin hydrochloride (α1 antagonist) were purchased from Sigma Aldrich (St. Louis, MO, USA). SB 269970 (selective 5-HT7 antagonist), BRL 15572 (selective 5-HT1D antagonist) and OHB12 (NO scavenger) were purchased from Tocris (Bristol, UK). Lerimazoline hydrochloride and phenylephrine hydrochloride were kindly donated from Zdravlje Actavis, Leskovac, Serbia.
All drugs, except indomethacin, were prepared as concentrated stocks in distillated water before dilution to the final concentration each day and stored at 4℃ during the experiment. Indomethacin was initially dissolved in 1% DMSO with subsequent dilutions carried out in distillated water. Drug concentrations are described as final molar concentrations in the tissue bath.
Male Wistar rats were euthanized with carbon dioxide and the thoracic aortas were dissected, cleared of connective tissue, and cut into cylindrical segments of approximately 3 mm length while the blood vessels were bathed in Petri dishes containing modified Krebs-bicarbonate solution (KBS) of the following composition: 118.3 mM NaCl, 4.7 mM KCl, 2.5 mM CaCl2, 1.2 mM MgSO4, 25 mM NaHCO3, 1.2 mM KH2PO4, 11 mM glucose. In a number of vessel preparations, the endothelial cell layer was removed by gently rubbing the luminal surface of the ring. Two stainless steel triangles were passed through the lumen of aortic rings, one of which was fixed to the organ bath wall whereas the other one was attached to the MLT0201 force displacement transducer (Panlab, Spain), mounted on a micrometer for manual adjustment of tension. The prepared aortic rings were mounted in a temperature-controlled organ baths (37℃) containing 25 ml Krebs solution which was continuously gassed with 95% O2 and 5% CO2.
The signal was digitalized using the PowerLab/4SP data acquisition system (AD Instruments, Castle Hill, Australia) and changes in isometric tension were recorded with LabChart 6 Pro software (AD Instruments). Four organ baths were run in parallel.
Segments were allowed to equilibrate for 1 h in KBS, during which it was replaced every 10 min to prevent accumulation of metabolic end-products. During further 20 min, each aortic ring was stretched progressively to optimal length of 2 g for maximal isometric contraction and additionally was allowed to equilibrate for 40 min before commencing the experiment. In those protocols involving consecutive obtainment of two or three concentration-response curves, after completion of the previous concentration-response curve, the response was terminated by exchanging the KBS every 10 min for 30 min, thus allowing the aortic rings to return to their baseline tension. Each segment of rat aorta was used only for one experimental protocol.
The first series of experiments were aimed to measure constrictive strength of two agonists, and consisted of two parts performed in separate aorta rings. First, concentration-response curves of phenylephrine were generated by adding it to the organ bath in cumulative concentrations (10−8~10−4 M). Second, concentration-response curves of lerimazoline were constructed by adding it to the organ bath in cumulative concentrations (10−7~3×10−4 M) and after washout, the contraction strength induced by 10−4 M phenylephrine was measured. Cumulative concentration-response curves were generated by increasing the concentration of phenylephrine or lerimazoline in half-log increments, once the constriction to the previous concentration had stabilized [1516].
The second series of experiments were aimed at assessing the effect of lerimazoline on contractile response induced by phenylephrine in aorta rings. Twenty min after obtaining the cumulative phenylephrine-induced contraction curve and washing out, lerimazoline was added directly to the organ bath. The effect of lerimazoline (2.1×10−3 M, 10−4, 10−6 or 10−7 M) on the concentration response curves for phenylephrine (10−8 to 10−5 M, with exception for the highest concentration of lerimazoline, where phenylephrine was used in concentration range 10−8 to 10−2 M) was assessed by comparing the contractile response in the absence or presence of lerimazoline.
In the third series of experiments, in order to evaluate the mechanism(s) responsible for lerimazoline-induced attenuation of the contractile response evoked by phenylephrine, each equilibrated rat aorta was first constricted by incremental concentrations of phenylephrine (10−8~10−4 M). The effect of pretreatment with nonspecific NOS inhibitor Nw-nitro-L-arginine methyl ester L-NAME (10−4 M), NO scavanger OHB12 (10−3 M), non-specific K+ channel blocker tetraethylammonium (10−3 M), cyclooxygenase inhibitor indomethacin (10−5 M), nonselective 5-HT antagonist methiothepin (10−4, 10−6 M or 3×10−7 M), selective 5-HT7 antagonist SB 269970 (10−6 M) or selective 5-HT1D antagonist BRL 15572 (10−6 M), on the concentration-response curve for phenylephrine was assessed by measuring the contractile response in the absence and presence of 10−4 M lerimazoline, respectively. The experiments without lerimazoline were performed in those cases where the respective inhibitor/antagonist has previously affected the putative interaction between phenylephrine and lerimazoline.
Throughout the experiment, the constriction strength was expressed as a percentage of the maximum tension induced by the highest concentration of phenylephrine used in the given protocol.
Contractions produced by phenylephrine, lerimazoline or different antagonists/inhibitors on their own were measured as changes in tension from baseline (i.e. the tension immediately before the respective agonist administration) and expressed as a percentage of the phenylephrine maximum (mean±S.E.M). Agonist potency expressed as an EC50 (the molar concentration necessary to produce 50% of the maximum agonist response) and maximum response (Emax) were determined from individual concentration-response curves by non-linear regression analysis.
In experiments with combined administration, EC50 values of phenylephrine obtained in the presence and absence of lerimazoline or the used inhibitor/antagonist were compared by an unpaired t-test. An analysis of variance was used to compare EC50 values and maximum responses obtained with phenylephrine, as well as phenylephrine and lerimazoline in the presence or absence of an inhibitor/antagonist. When the ANOVA indicated that differences existed between groups, Tukey's multiple-comparison test was applied to determine the source of variation [17]. The n values refer to the number of aorta vessels tested. Statistical significance was accepted at p<0.05.
The agonists used in this study exhibited different contractile activity in rat thoracic aortas, irrespective of presence of endothelium. The addition of lerimazoline to the isolated tissues produced virtually no change in isometric tension over the concentration range of 10−7~10−5 M. For higher doses, in the range 10−5~3×10−4 M, lerimazoline produced the maximal response of about 45% of the response induced by 10−4 M phenylephrine, with pEC50=4.20 (Fig. 1). Specifically, phenylephrine started to increase tension from the first concentration of the drug tested (10−8 M), with the pEC50=5.77.
A quantitative comparative study was conducted to examine the effect of lerimazoline on response to phenylephrine. Higher concentrations of lerimazoline (2.1×10−3 M and 10−4 M) highly significantly attenuated maximal response (p<0.001) of phenylephrine concentration-response curve (Emax=100±0.00% and 8.78±2.47%; pEC50 being 5.46±0.31 and 3.06±0.72, p<0.05, for phenylephrine alone and with lerimazoline 2.1×10−3 M, respectively, Fig. 2A; and Emax=100±0.00% and 9.91±4.58%; pEC50 being 5.60±0.17 and 5.23±0.23, p>0.05, for phenylephrine alone and with lerimazoline 10−4 M, respectively, Fig. 2B). However, in tissue precontracted with lerimazoline (10−6 and 10−7 M), phenylephrine produced vasoconstrictor responses which were markedly more prominent then those observed in previous preparations, containing high concentrations of lerimazoline. Indeed, the lower concentrations of lerimazoline (10−6 and 10−7 M) produced a significant potentiation of the phenylephrine-induced contractions (Fig. 2C, D), with fine differences between the effects of two concentrations. While lerimazoline (10−7 M) produced a potentiation of the phenylephrine-induced contractions starting from the lowest concentration of phenylephrine (Emax from 100±0.00% in the absence to 168.10±21.40% in the presence of lerimazoline, Fig. 2D, p<0.01) without significant change in pEC50 (6.11±0.20 control vs 5.92±0.27 in the presence of lerimazoline), a significant increase in maximum response of phenylephrine-evoked vasoconstriction by lerimazoline (10−6 M) occurred only at phenylephrine concentrations of 3×10−6 M and 1×10−5 M (Fig. 2C; p<0.05 at 3×10−6 M and p<0.001 at 1×10−5 M). Moreover, the vasoconstrictive effects of lower concentrations of phenylephrine tended to be counteracted by lerimazoline, a significant decrease being observed at 3×10−7 M of phenylephrine. The Emax value was 100±0.00% in the absence vs 139.99±10.65% in presence of lerimazoline at the concentration of 1×10−6 M, p<0.01, with a significant change in pEC50 (5.60±0.29 control vs 4.62±0.27, p<0.05).
In order to elucidate the mechanistic substrate for an unprecedented antagonism of contractile actions of phenylephrine exerted by lerimazoline, we chose to test the increasing concentrations of phenylephrine in presence of various ligands in two protocols: in the absence and presence of 10−4 M lerimazoline. The pEC50 values of combination of phenylephrine and lerimazoline obtained in the absence and presence of the given concentration of ligand, together with the respective number of blood vessel preparations, are given in Table 1.
A quantitative comparative study was performed with the goal to examine the effect of L-NAME (10−4 M) and OHB12 (10−3 M) on responses to phenylephrine in the absence and presence of lerimazoline (10−4 M). Primary, L-NAME potentiated the Emax to phenylephrine in thoracic aorta rings. The maximal contraction pretreated with L-NAME increased from 100% to 163.38±21.06% (Fig. 3A; *p<0.05). Lerimazoline (10−4 M) caused a significant decrease (***p<0.001, Student's unpaired t-test) in the maximum contraction response to phenylephrine from 100% to 55.95±6.47%. The non-selective inhibitor of NO synthesis L-NAME completely reversed the lerimazoline-induced attenuation of the contractile effect of higher doses of phenylephrine. Under these conditions L-NAME increased significantly the maximum contractions of phenylephrine pretreated with lerimazoline (10−4 M) from 55.95±6.47% to 84.59±10.49% (Fig. 3B; #p<0.05,). OHB12 potentiated the Emax to phenylephrine in thoracic aorta rings from 100% to 155.25±11.76% (Fig. 3C; **p<0.01). The maximum response to phenylephrine pretreated with lerimazoline was also significantly increased from 49.18±10.25% to 101.53±12.49% in the presence of OHB12 (Fig. 3D; ##p<0.01).
The interaction between phenylephrine and lerimazoline was examined in the presence of indomethacin or tetraethylammonium (TEA). While the cyclooxygenase inhibitor indomethacin (10−5 M) did not change the basal tone of the vessels pretreated with lerimazoline (Fig. 4A; p>0.05), TEA (10−3 M), a non-specific inhibitor of K+ channels, potentiated the effect of phenylephrine in the thoracic aorta pretreated with lerimazoline. Namely, while TEA did not significantly affect the maximal response to phenylephrine in thoracic aorta rings (Fig. 4B), it increased significantly the maximum contractions of phenylephrine pretreated with lerimazoline (10−4 M), from 59.56±8.53% to 103.32±11.31% (Fig. 4C; ##p<0.01).
The sensitivity of the interaction of phenylephrine and lerimazoline to antagonism by methiothepin was evaluated using three antagonist concentrations (10−4, 10−6 and 3×10−7 M). Methiothepin (10−4 M) caused complete amelioration in tension of phenylephrine induced contraction of rings pretreated with lerimazoline (Emax: 62.49±13.58% in presence of 10−4 M lerimazoline vs 13.94±6.52% in presence of 10−4 M lerimazoline plus 10−4 M methiothepin Fig. 5A, ##p<0.01). The response to phenylephrine in aortic segments untreated with lerimazoline was significantly inhibited by methiothepin at 10−6 M (Fig. 5B, p<0.05), but not at a lower concentration (3×10−7 M) (Fig. 5D). On the contrary, in the presence of lower concentrations of methiothepin (10−6 and 3×10−7 M), concentration response curve to phenylephrine pretreated with lerimazoline was increased at the last three concentrations of phenylephrine concentration response curve (Emax: 59.24±10.42% in presence of 10−4 M lerimazoline vs 87.08±14.83% in presence of 10−4 M lerimazoline plus 10−6 M methiothepin, Fig. 5C; 48.68±3.73% in presence of 10−4 M lerimazoline vs 74.42±11.27% in presence of 10−4 M lerimazoline plus 3×10−7 M methiothepin, Fig. 5E; #p<0.05).
The interaction between phenylephrine and lerimazoline was examined in the presence of higly selective 5-HT7 receptor antagonist SB 269970 (Fig. 6A) and selective 5-HT1D receptor antagonist BRL 15572 (Fig. 6B). Results have shown that neither SB 269970 (10−6 M) nor BRL 15572 (10−6 M) did change the basal tone of the vessels pretreated with lerimazoline (47.89±5.52% in presence of 10−4 M lerimazoline vs 45.24±5.42% in presence of lerimazoline plus 10−6 M SB 269970, p>0.05; 62.08±16.01% in presence of 10−4 M lerimazoline vs 58.76±11.74% in presence of lerimazoline plus 10−6 M BRL 15572, p>0.05).
Our study revealed that there is an intricate interaction between phenylephrine, a strong vasoconstrictor selective for α1 adrenergic receptors, and lerimazoline, an imidazoline ligand whose moderate vasoconstrictor actions have been related more to activation of 5-HT1B [9] or 5-HT2A [Rizvic et al., manuscript in preparation], than α1 adrenergic receptors. While lower concentrations of lerimazoline (10−6 or 10−7 M) tended to potentiate the vasoconstrictor activity of phenylephrine, lerimazoline in higher concentrations (10−4 M and above) unveiled the potential to profoundly suppress the phenylephrine-induced vasoconstriction. The latter action was totally unexpected and asked for further elucidation.
Potentiation of phenylephrine-induced contractions by low lerimazoline concentrations could be explained as follows: phenylephrine activated its α1 receptors on vascular smooth muscle cells and exhibited potent vasoconstrictor effects, while lerimazoline may potentiated that action by eliciting additional contractile effects related to activation of 5-HT1B [9] and/or 5-HT2A receptors. On the other hand, it is not possible to propose a parsimonious explanation for the antagonistic action of higher concentrations of lerimazoline on contraction of rat aorta produced by phenylephrine. It has been noticed that cumulative addition of 10−4 M lerimazoline (a concentration that significantly attenuated phenylephrine concentration-response curve), induced contraction of rat aorta of about 20% of the response induced by 10−4 M phenylephrine ([5]; the present results), while a one-time addition of the same lerimazoline concentration did not induce any change in the tone of the same vessel (the present results). However, in the latter, but not the former case, lerimazoline was added into organ bath after obtaining the cumulative phenylephrine-induced contraction curve and washing out, and in such settings a kind of homologous (related to α1 adrenergic receptors) or, more probably, heterologous (related to distinct subtypes of 5-HT receptors) desensitization, demonstrated and described in detail in rabbit aorta exposed to norepinephrine and angiotensin II [18], could have taken its place.
Two main questions to be addressed are related to molecular messengers and receptor substrates of the observed attenuation of phenylephrine-induced rat aorta contraction achieved by lerimazoline, as a vasoconstrictive, rather than vasodilatory, agent on its own. Endothelium plays an important role in the regulation of vasoconstriction and vasodilation response elicited by different agonists. It releases vasodilatator factors, i.e. NO, EDHF and prostacyclin, as well as vasoconstrictor factors, i.e. endothelin 1, COX-derived vasoconstrictor products and superoxide anion [1920]. While NO inhibits the contractile response to many vasoconstrictors [2122], EDHF causes endothelium-dependent hyperpolarization and relaxation in the rat aorta by opening K+ channels, which cannot be overcome by the full blockade of NOS and cyclooxigenase [21]. As we used both, endothelium intact and denuded rings and the vascular activity of phenylephrine and lerimazoline, on their own and in combination, was unaffected by presence or absence of endothelium, it could be supposed that modulation of endothelial-derived vasoactive factors would not dominantly change the blood vessel reactivity to them. Nevertheless, the possibility of involvement of endogenously produced NO or prostaglandins in the mediation of phenylephrine – lerimazoline interaction was studied in the presence of the NO inhibitors L-NAME and OHB12 or cyclooxygenase inhibitor indomethacin, respectively. In addition, we investigated the influence of non-selective K+ inhibitor tetraethylammonium on attenuation of phenylephrine-induced contraction induced by lerimazoline. Lastly, the place of the 5-HT receptor pathway in the observed interaction was assessed using the highly selective 5-HT1D receptor antagonist BRL 15572, 5-HT7 receptor antagonist SB 269970 and non-selective 5-HT receptor antagonist methiothepin.
Pretreatment with L-NAME or OHB12 reduced the lerimazoline-induced attenuation of the maximal contractile response to phenylephrine. This effect may be at least partially correlated via the NO-mediated modulation by lerimazoline of the phenylephrine contraction. However, assessment of relative contribution of this mechanism to the overall action of lerimazoline is hampered by the fact that both, L-NAME and OHB12 significantly potentiated the phenylephrine contraction on its own. On the other hand, the opening of K+ channels in vascular smooth muscle cells triggers membrane potential hyperpolarization and thus provides an important mechanism to prevent blood vessel contraction, the activities of certain K+-channels are inhibited by the non-selective blocker TEA. The opening of K+ channels is probably activated by lerimazoline irrespective of phenylephrine, since there was no significant potentiation in the phenylephrine concentration-response curve pretreated with TEA. The described pattern of possible signaling mechanisms is not unique; as an example, a similar pattern was reported for amfepramone (diethylpropion), an appetite-suppressant drug with incompletely elucidated receptor/channel binding profile, but with a substantial difference that amfepramone on its own tended to relax rather than contract rat aortic rings [23].
In regard to the receptor pathways involved in the lerimazoline functional antagonism of the phenylephrine-induced rat aorta contraction, we concentrated on the 5-HT7 receptor. Namely, it is well documented that 5-HT exerts a major part of its vasodilatory potential by activation of 5-HT7 receptors, which can be prevented by use of the selective antagonist SB 269970. As an example, it is shown that 5-HT directly relaxes the rat superior mesenteric veins primarily through activation of the 5-HT7 receptor [24]. Moreover, 5-HT was able to exert direct relaxant responses in canine basilar and middle cerebral arteries via the same, 5-HT7 receptors [25]. On the other hand, BRL 15572, as the selective antagonist at the 5-HT1D receptor, was used as a kind of negative control, having in mind that the canine external carotid vasodilator responses remained unaffected in presence of this ligand [26]. However, it appeared that not only the 5-HT1D, but also the 5-HT7 receptor was not involved in relaxant influences of lerimazoline. Nevertheless, the experiment with methiothepin gave a hint about the receptor substrate of the relaxant potential of lerimazoline. Namely, while methiothepin at 10−4 M did not affect the action of lerimazoline, methiothepin at 10−6 and 3×10−7 M significantly reversed the lerimazoline-induced attenuation of the phenylephrine concentration-response curve, the lower concentration of methiothepin being devoid of the potential to interact with phenyleprine. If we assume that methiothepin in low concentrations did bind only to those receptors for which possesses the highest affinity, we can postulate that the 5-HT2B subtype, to which methiothepin has Ki in the range 8.7~9.2 (IUPHAR database), was the first receptor blocked with methiothepin, significantly increasing in turn the contractile action of the blood vessel exposed to phenylephrine and lerimazoline in combination. This is in accordance with findings that 5-HT2B receptors are located on the endothelial cell and, when activated, stimulate NO release [27]. Moreover, it was demonstrated that treatment with 5-HT2B receptor antagonist abolishes a bypass-induced fall in blood pressure in Wistar rat in vivo [28]. It is worth to note that the second in a row binding site for methiothepin is the 5-HT7 receptor (with Ki value in the range 8.4~9.4) (IUPHAR database), which suggests once more that the 5-HT2B receptor is the probable receptor substrate of the relaxant actions of lerimazoline; however, further work is necessary before definite assignments can be made.
Finally, it shall be commented that the seemingly paradoxical pattern of actions of lerimazoline, with its moderate contractile activity, but also a capability to suppress the contraction induced by another, more effective contractile agent, should not be regarded as totally unprecedented. As an important example, Lamarre et al. [29] have reported that cocaine can exhibit both vasoconstricting and vasorelaxant effects. In fact, at a concentration devoid of effects on its own, cocaine potentiated the vasoconstriction produced by norepinephrine, as well the α1-selective agonists phenylephrine and methoxamine. On the other hand, higher concentrations of cocaine in combination with adrenergic agonists exerted a concentration-related relaxation, i.e. gave an inverted-U shaped (hormetic) dose–effect curve. The authors postulated that the relaxing component of the effect was due to activation of myosin light chain phosphatase by cocaine, shown by Li et al. [30].
In conclusion, the present results indicate that the presence of lerimazoline, at a concentration close to and above that of phenylephrine, may result in the level of vasoconstriction less pronounced than that obtained with either of agents alone. In can be hypothesized that the interaction of lerimazoline with phenylephrine as one of standard decongestants, effected through receptor and signaling mechanisms probably involving the substrates other than the α1 adrenergic receptor, may suppress or slow down the development of the rebound congestion, which needs further research and assessment in clinical settings.
Figures and Tables
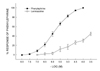 | Fig. 1Comparison of the contractile effect of phenylephrine (n=12) and lerimazoline (n=12) on rat thoracic aorta.Data are shown as mean±S.E.M, expressed for phenylephrine as the percentage of maximum contraction induced by maximum dose of phenylephrine, and for lerimazoline as the percentage of maximum contraction induced by 10−4 M phenylephrine.
|
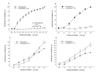 | Fig. 2Vascular responses to phenylephrine in blood vessels exposed to different concentrations of lerimazoline.(A) Concentration-response curves for phenylephrine in the absence (•, n=7) and in the presence of lerimazoline 2.1×10−3 M (∘, n=7). (B) Concentration–response curves for phenylephrine in the absence (•, n=10) and in the presence of lerimazoline 10−4 M (∘, n=10). (C) Concentration–response curves for phenylephrine in the absence (•, n=10) and in the presence of lerimazoline 10−6 M (∘, n=10). (D) Concentration–response curves for phenylephrine in the absence (•, n=9) and in the presence of lerimazoline 10−7 M (∘, n=9). Results (means±S.E.M) were expressed as percentages of the response to the 10−4 M phenylephrine. *p<0.05, **p<0.01 vs. the effect of the respective concentration of phenylephrine.
|
 | Fig. 3Effects of L-NAME and OHB12 on the vasoconstrictor responses induced by phenylephrine and lerimazoline.(A) Effect of 10−4 M L-NAME on the phenylephrine concentration response curve in rings without 10−4 M lerimazoline. (B) Effect of 10−4 M L-NAME on the phenylephrine concentration response curve in rings pretreated with 10−4 M lerimazoline. (C) Effect of 10−3 M OHB12 on the phenylephrine concentration response curve in rings without 10−4 M lerimazoline. (D) Effect of 10−3 M OHB12 on the phenylephrine concentration response curve in rings pretreated with 10−4 M lerimazoline.Results (means±S.E.M) were expressed as percentages of the response to the 10−4 M phenylephrine. *p<0.05, **p<0.01, ***p<0.001 vs. phenylephrine; #p<0.05, ##p<0.01, ###p<0.001 vs. phenylephrine plus lerimazoline.
|
 | Fig. 4Effects of indomethacin and TEA on the vasoconstrictor responses induced by phenylephrine and lerimazoline.(A) Effect of 10−5 M indomethacin on the phenylephrine concentration response curve in rings pretreated with 10−4 M lerimazoline. (B) Effect of 10−3 M TEA on the phenylephrine concentration response curve in rings without 10−4 M lerimazoline. (C) Effect of 10−3 M TEA on the phenylephrine concentration response curve in rings pretreated with 10−4 M lerimazoline. Results (means±S.E.M) were expressed as percentages of the response to the 10−5 M phenylephrine. *p<0.05, **p<0.01, ***p<0.001 vs. phenylephrine; #p<0.05, ##p<0.01 vs. phenylephrine plus lerimazoline.
|
 | Fig. 5Effects of methiothepin on the vasoconstrictor responses induced by phenylephrine and lerimazoline.(A) Effect of 10−4 M methiothepin on the phenylephrine concentration response curve in rings pretreated with 10−4 M lerimazoline. (B) Effect of 10−6 M methiothepin on the phenylephrine concentration response curve in rings without 10−4 M lerimazoline. (C) Effect of 10−6 M methiothepin on the phenylephrine concentration response curve in rings pretreated with 10−4 M lerimazoline. (D) Effect of 3×10−7 M methiothepin on the phenylephrine concentration response curve in rings without 10−4 M lerimazoline. (E) Effect of 3×10−7 M methiothepin on the phenylephrine concentration response curve in rings pretreated with 10−4 M lerimazoline. Results (means±S.E.M.) were expressed as percentages of the response to 10−4 M phenylephrine. *p<0.05, **p<0.01, ***p<0.001 vs. phenylephrine; #p<0.05, ##p<0.01 vs. phenylephrine plus lerimazoline.
|
 | Fig. 6Effects of SB 269970 and BRL 15572 on the vasoconstrictor responses induced by phenyephrine and lerimazoline.(A) Effect of 10−6 M SB 269970 on the phenylephrine concentration response curve in rings pretreated with 10−4 M lerimazoline. (B) Effect of 10−6 M BRL 15572 on the phenylephrine concentration response curve in rings pretreated with 10−4 M lerimazoline. Results (means±S.E.M) were expressed as percentages of the response to 10−4 M phenylephrine. *p<0.05, **p<0.01, ***p<0.001 vs. phenylephrine; #p<0.05, ##p<0.01 vs. phenylephrine plus lerimazoline.
|
ACKNOWLEDGEMENTS
This work was supported in part by the Ministry of Education, Science and Technological Development, R. Serbia – Grant No. 175076 (MMS). We acknowledge the contribution to discussion made by Ms. Aleksandra Vidojević and technical assistance of Ms. Milica Gajić.
Notes
References
1. Corey JP, Houser SM, Ng BA. Nasal congestion: a review of its etiology, evaluation, and treatment. Ear Nose Throat J. 2000; 79:690–698.
2. Furukawa K, Chess-Williams R, Uchiyama T. Alpha 1B-adrenoceptor subtype mediating the phenylephrine-induced contractile response in rabbit corpus cavernosum penis. Jpn J Pharmacol. 1996; 71:325–331.
3. Hussain MB, Marshall I. Characterization of alpha1-adrenoceptor subtypes mediating contractions to phenylephrine in rat thoracic aorta, mesenteric artery and pulmonary artery. Br J Pharmacol. 1997; 122:849–858.
4. Morton JS, Daly CJ, Jackson VM, McGrath JC. Alpha(1A)-adrenoceptors mediate contractions to phenylephrine in rabbit penile arteries. Br J Pharmacol. 2007; 150:112–120.
5. Brayfield A, Martindale W. Martindale: the complete drug reference. 38th ed. London: Pharmaceutical Press;2014.
6. Boudier HS, de Boer J, Smeets G, Lien EJ, van Rossum J. Structure activity relationships for central and peripheral alpha adrenergic activities of imidazoline derivatives. Life Sci. 1975; 17:377–385.
7. Malta E, Ong JS, Raper C, Tawa PE, Vaughan GN. Structure-activity relationships of clonidine- and tolazoline-like compounds at histamine and alpha-adrenoceptor sites. Br J Pharmacol. 1980; 69:679–688.
8. Nathanson JA. Phenyliminoimidazolidines. Characterization of a class of potent agonists of octopamine-sensitive adenylate cyclase and their use in understanding the pharmacology of octopamine receptors. Mol Pharmacol. 1985; 28:254–268.
9. Law H, Dukat M, Teitler M, Lee DK, Mazzocco L, Kamboj R, Rampersad V, Prisinzano T, Glennon RA. Benzylimidazolines as h5-HT1B/1D serotonin receptor ligands: a structure-affinity investigation. J Med Chem. 1998; 41:2243–2251.
10. Bhattacharya A, Schenck KW, Xu YC, Nisenbaum L, Galbreath E, Cohen ML. 5-Hydroxytryptamine1B receptor-mediated contraction of rabbit saphenous vein and basilar artery: role of vascular endothelium. J Pharmacol Exp Ther. 2004; 309:825–832.
11. Rameshrad M, Babaei H, Azarmi Y, Fouladia DF. Rat aorta as a pharmacological tool for in vitro and in vivo studies. Life Sci. 2016; 145:190–204.
12. Morán A, Ortiz de Urbina AV, Martín ML, García M, Rodriguez-Barbero A, Dorado F, San Román L. Characterization of contractile 5-hydroxytryptamine receptor subtypes in the in situ autoperfused kidney in the anaesthetized rat. Eur J Pharmacol. 2008; 592:133–137.
13. Fernández MM, Morán A, Martín ML, San Román L. Mesenteric vasoconstrictor response to 5-hydroxytryptamine in the in situ blood autoperfused rat mesentery: involvement of 5-HT(2B) and/or 5-HT(2C) receptor activation. Eur J Pharmacol. 2000; 401:221–227.
14. Calama E, Fernández MM, Morán A, Martín ML, San Román L. Vasodilator and vasoconstrictor responses induced by 5-hydroxytryptamine in the in situ blood autoperfused hindquarters of the anaesthetized rat. Naunyn Schmiedebergs Arch Pharmacol. 2002; 366:110–116.
15. Flavahan NA, McGrath JC. Are human vascular alpha-adrenoceptors atypical? J Cardiovasc Pharmacol. 1984; 6:208–210.
16. Chotani MA, Flavahan S, Mitra S, Daunt D, Flavahan NA. Silent alpha(2C)-adrenergic receptors enable cold-induced vasoconstriction in cutaneous arteries. Am J Physiol Heart Circ Physiol. 2000; 278:H1075–H1083.
17. Wallenstein S, Zucker CL, Fleiss JL. Some statistical methods useful in circulation research. Circ Res. 1980; 47:1–9.
18. Jerez S, Peral de, Coviello A. Cross talk between angiotensin II and alpha 1 adrenergic receptors in rabbit aorta: role of endothelium. J Cardiovasc Pharmacol. 2004; 43:402–409.
19. Lüscher TF. 1993 Mack Forster Award Lecture. Review. The endothelium as a target and mediator of cardiovascular disease. Eur J Clin Invest. 1993; 23:670–685.
20. Marín J, Rodríguez-Martínez MA. Role of vascular nitric oxide in physiological and pathological conditions. Pharmacol Ther. 1997; 75:111–134.
21. Hatake K, Wakabayashi I, Hishida S. Endothelium-dependent relaxation resistant to NG-nitro-L-arginine in rat aorta. Eur J Pharmacol. 1995; 274:25–32.
22. Stallone JN. Role of endothelium in sexual dimorphism in vasopressin-induced contraction of rat aorta. Am J Physiol. 1993; 265:H2073–H2080.
23. López-Canales JS, Lozano-Cuenca J, Muãoz-Islas E, Aguilar-Carrasco JC, López-Canales OA, López-Mayorga RM, Castillo-Henkel EF, Valencia-Hernández I, Castillo-Henkel C. Mechanisms involved in the vasorelaxant effects produced by the acute application of amfepramone in vitro to rat aortic rings. Braz J Med Biol Res. 2015; 48:537–544.
24. Watts SW, Darios ES, Seitz BM, Thompson JM. 5-HT is a potent relaxant in rat superior mesenteric veins. Pharmacol Res Perspect. 2015; 3:e00103.
25. Terrón JA, Falcón-Neri A. Pharmacological evidence for the 5-HT7 receptor mediating smooth muscle relaxation in canine cerebral arteries. Br J Pharmacol. 1999; 127:609–616.
26. Muñoz-Islas E, Lozano-Cuenca J, González-Hernández A, Ramírez-Rosas MB, Sánchez-López A, Centurión D, Maassenvandenbrink A, Villalón CM. Spinal sumatriptan inhibits capsaicin-induced canine external carotid vasodilatation via 5-HT1B rather than 5-HT1D receptors. Eur J Pharmacol. 2009; 615:133–138.
27. Ishida T, Kawashima S, Hirata K, Yokoyama M. Nitric oxide is produced via 5-HT1B and 5-HT2B receptor activation in human coronary artery endothelial cells. Kobe J Med Sci. 1998; 44:51–63.
28. Borgdorff P, Fekkes D, Tangelder GJ. Hypotension caused by extracorporeal circulation: serotonin from pump-activated platelets triggers nitric oxide release. Circulation. 2002; 106:2588–2593.
29. Lamarre NS, Raffa RB, Tallarida RJ. Cocaine synergism with α agonists in rat aorta: computational analysis reveals an action beyond reuptake inhibition. Drug Alcohol Depend. 2013; 129:226–231.
30. Li W, Su J, Sehgal S, Altura BT, Altura BM. Cocaine-induced relaxation of isolated rat aortic rings and mechanisms of action: possible relation to cocaine-induced aortic dissection and hypotension. Eur J Pharmacol. 2004; 496:151–158.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download