Abstract
Crohn's disease (CD) is a chronic inflammatory bowel disease with multifactorial causes including environmental and genetic factors. Several studies have demonstrated that the organic cation/carnitine transporter 1 (OCTN1) non-synonymous variant L503F is associated with susceptibility to CD. However, it was reported that L503F is absent in Asian populations. Previously, we identified and functionally characterized genetic variants of the OCTN1 promoter region in Koreans. In that study, four variants demonstrated significant changes in promoter activity. In the present study, we determined whether four functional variants of the OCTN1 promoter play a role in the susceptibility to or clinical course of CD in Koreans. To examine it, the frequencies of the four variants of the OCTN1 promoter were determined by genotyping using DNA samples from 194 patients with CD and 287 healthy controls. Then, associations between genetic variants and the susceptibility to CD or clinical course of CD were evaluated. We found that susceptibility to CD was not associated with OCTN1 functional promoter variants or haplotypes showing altered promoter activities in in vitro assays. However, OCTN1 functional promoter haplotypes showing decreased promoter activities were significantly associated with a penetrating behavior in CD patients (HR=2.428, p=0.009). Our results suggest that the OCTN1 functional promoter haplotypes can influence the CD phenotype, although these might not be associated with susceptibility to this disease.
Organic cation/carnitine transporter (OCTN) of the solute carrier (SLC) 22 family has two isoforms in humans, OCTN1 and OCTN2 [1]. OCTN1, which is encoded by SLC22A4, is expressed in various organs, including the bone marrow, gut, heart, kidney, and lung [1]. OCTN1 transports various endogenous substances or drugs, including ergothioneine, carnitine, tetraethylammonium, and gabapentin, in a sodium- or pH-dependent manner according to the features of the substrates [12345]. Although the physiological role of OCTN1 is not yet well established, previous studies have suggested that this transporter accumulates the anti-oxidant ergothioneine for protecting the body against oxidative stress [15].
Few studies have investigated the role of the genetic variants of OCTN1 in the expression or transport activity of this transporter. Toh et al. [6] identified four single nucleotide polymorphisms (SNPs) of OCTN1 that impair transport activity. In addition, Tahara et al. [7] investigated the functions and effects of SNPs in the proximal promoter region of OCTN1, and determined that all OCTN1 haplotypes identified in their study population showed promoter activity comparable to that of the reference. Previously, we identified and functionally characterized novel OCTN1 promoter variants in Koreans [8]. In that study, we observed that four promoter SNPs resulted in significantly altered promoter activity, compared to the reference. Two of them, g.–1875T>A and g.–1745A>G, demonstrated increased promoter activity, whereas the other two, g.–1145A>G and g.–248C>G, demonstrated decreased promoter activity. Very few studies have investigated the effect of OCTN1 genetic variants on the response or pharmacokinetics of drugs. Urban et al. [2] reported that OCTN1 genetic variants could impact the pharmacokinetics of the anti-epilepsy drug, gabapentin. They found that a non-synonymous variant of OCTN1, L503F demonstrated decreased transport activity for gabapentin, and subjects who were homozygous for this variant demonstrated significantly decreased renal secretion of gabapentin.
Crohn's disease (CD) is a chronic idiopathic inflammatory bowel disease that could involve the whole gastrointestinal tract. Although the pathogenesis of CD remains unclear, it is accepted that CD can be induced by abnormal immune responses against gut flora, in particular, in genetically susceptible individuals [9]. To date, a large number of studies have examined the association between genetic variants and susceptibility to or clinical phenotypes of CD, and many genes, such as NOD2, ATG16L1, IRGM, IBD5, and TNFSF15 were shown to be significantly associated with CD [10111213]. In the case of OCTN, Peltekova et al. [4] reported an association between the TC haplotype of OCTNs consisting of two genetic variants, OCTN1, L503F and OCTN2, g.–207G>C and susceptibility to CD. This finding was validated by several other association studies [141516171819202122]. However, previous studies reported that these two variants are not found in Asian populations [171819]. In particular, to our knowledge, no other study has investigated the association between genetic variants in the OCTN1 promoter as well as susceptibility to CD. Therefore, in the present study, we investigated whether the genetic variants of the OCTN1 promoter that demonstrated altered promoter activity in our previous study could affect the susceptibility to or clinical course of CD in Koreans.
The study protocol was reviewed and approved by the Institutional Review Board of the Ewha Medical Center, Seoul, Korea, and the Institutional Review Board of Severance Hospital at Yonsei University Health System, Seoul, Korea. After receiving written informed consent, DNA samples were obtained from 194 Korean patients with CD. Those diagnosed with CD had at least a 24-month follow-up period with assessment by internal medicine specialists. The CD patients were subgrouped according to age of onset, location, and disease behavior using the Montreal Classification [23]. Among disease behaviors, “penetrating behavior” refers to the presence of intestinal perforation, intraabdominal fistula, or inflammatory mass and/or abscess. For the control group, DNA samples were collected from 287 unrelated healthy Koreans who had no evidence of abnormalities during routine gastrointestinal examinations, showed no gastrointestinal symptoms and took no regular medications at Severance Hospital. Clinical data were obtained by reviewing the medical records.
In the present study, four OCTN1 promoter variants, g.–1875T>A, g.–1745A>G, g.–1145A>g, and g.–248C>G, which showed significant changes in promoter activity in our previous study [8], were genotyped by a SNaPshot assay using an automated DNA analyzer (DNA Link, Inc., Seoul, Korea).
To compare the frequency of OCTN1 genetic variations or haplotypes between patients and control groups, a χ2-test was conducted. Comparisons of the characteristics between patient groups according to OCTN1 functional haplotypes were analyzed using the χ2-test and t-test. The effects of the OCTN1 functional haplotypes on the clinical course (disease behavior, azathioprine or anti-TNF agent use, and surgery) of CD were initially investigated using the Kaplan-Meier estimator and log-rank test to consider time to clinical events. Then, the multivariate Cox proportional hazards regression analysis (for each clinical parameter) was performed with adjustment for sex and age of onset.
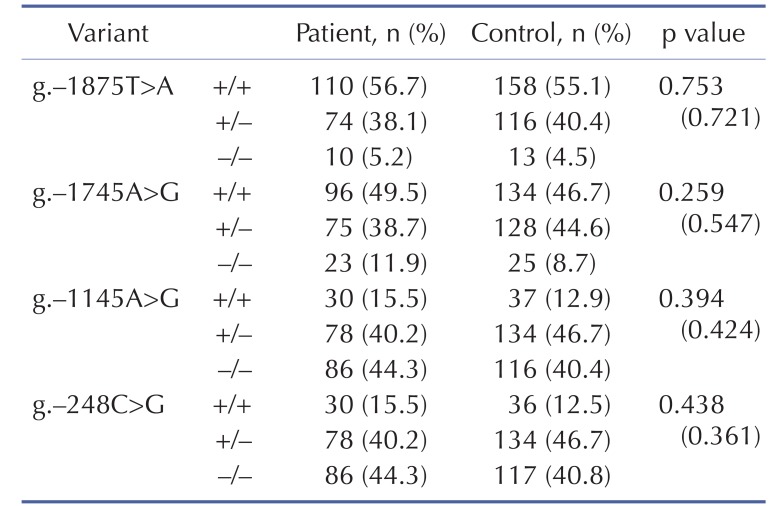
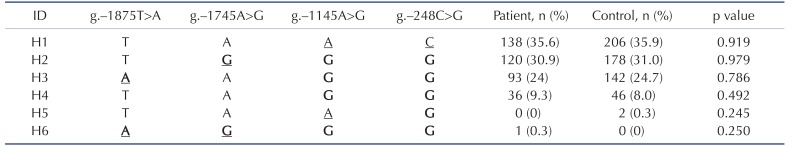
We compared the frequencies of OCTN1 functional variants or haplotypes reported in our previous study [8] between patients with CD and healthy control groups. Table 1 shows the frequency of the four variants between the two groups. We observed that there was no significant difference in the frequency of any of the genetic variants analyzed between the two groups. Using genotype data, haplotypes were assembled using the Haploview program (version 4.3, Broad Institute, Cambridge, MA, USA). There were six promoter haplotypes in our population. The frequency of each haplotype in CD patient and control groups is listed in Table 2. We observed that the frequency of haplotypes in CD patients was comparable with those of the control group. These findings indicate that the susceptibility to CD might not be affected by OCTN1 functional variants or haplotypes in Koreans.
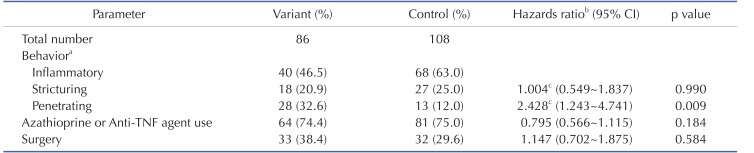
Next, we examined whether the functional promoter haplotypes ofOCTN1 could affect the clinical characteristics of patients with CD, although we found that these haplotypes did not affect susceptibility to CD. Here, we hypothesized that theOCTN1 functional haplotypes that demonstrated decreased promoter activity could be associated with a severe clinical course of CD, as the well-knownOCTN1 variant L503F demonstrated a reduction in transport activity in a previous study [4]. In our population, fiveOCTN1 promoter haplotypes, (H2 to H6) were predicted to have decreased promoter activity according to the results of our previous study [8]. Therefore, we divided the 194 patients into two groups according to the fiveOCTN1 haplotypes: a variant group (n=86) and a control group (n=108). The variant group consisted of subjects having two of five promoter haplotypes, and the control group consisted of subjects who were not members of the variant group. First, we compared the demographic or clinical characteristics of CD patients and observed that the functional haplotypes showing decreasedOCTN1 promoter activity were not associated with sex, age of onset, body mass index, or disease location in Korean patients with CD (Table 3). Then, we examined the association between OCTN1 functional promoter haplotypes and clinical course of CD. We found that OCTN1 haplotypes significantly affected the time to development of a penetrating disease behavior (log-rank p=0.008, Fig. 1), while other clinical events such as usage of azathioprine or anti-TNF agents or surgery were not affected by the haplotypes (data not shown). The risk of a penetrating behavior was significantly higher in patients in the variant group compared to the control group (hazards ratio (HR)=2.428, p=0.009) after adjustment for sex and age of onset in a Cox proportional hazards model (Table 4). The usage of azathioprine or anti-TNF agents and need for surgery were comparable between the two groups.
Crohn's disease (CD) is a chronic relapsing inflammatory disease and its incidence and prevalence are increasing with time [24]. Although the etiopathogenesis of CD is unclear, it is well accepted that this disease could be caused by dysregulated immune responses in genetically susceptible subjects [9]. Previous genome-wide or genotype-phenotype association studies have reported a significant association between genetic variants and susceptibility to or clinical phenotypes of CD [10111213]. In particular, it was shown that several genetic variants of IL12B, TNFSF15, IL23R, and ATG16L2 were associated with susceptibility to or phenotypes of CD in Koreans [252627]. The TC haplotype consisting of OCTN1, L503F and OCTN2, g.–207G>C was shown to be a predictor of CD development [4]. Several studies have found that L503F and –207G>C are ethnic-specific variants. For example, it has been reported that the frequencies of L503F and –207G>C were 0.412 and 0.500, respectively, in Europeans [728]. In those studies, the frequencies of these variants were also high in Mexicans: the frequencies of L503F and –207G>C were 0.230 and 0.679, respectively. However, interestingly, both are absent in Asian populations [171819]. Recently, we reported that the functional haplotype of the OCTN2 promoter was associated with the clinical course in Korean CD patients [29]. In that study, compared to the controls, we observed much higher frequencies of a penetrating behavior and need for surgery in patients with the OCTN2 haplotype showing decreased promoter activity.
In the present study, we evaluated the clinical usefulness of OCTN1 functional haplotypes identified in our previous study [8]. First, we investigated the association between genetic variants of the OCTN1 promoter and CD. The four variants showing significant changes in promoter activity in our previous study were not associated with susceptibility to CD in Koreans. In addition, the frequencies of all variants or haplotypes were comparable between patients and healthy controls. Vermeire et al. [30] previously reported that OCTN1, L503F was not associated with susceptibility to inflammatory bowel diseases, including CD, but was associated with the clinical phenotypes of the disease, particularly perianal or penetrating complications in the population that was studied. Therefore, we next examined whether OCTN1 functional promoter haplotypes could affect CD phenotypes. Previous studies reported that OCTN1 is expressed in the intestinal epithelium and plays a protective role against oxidative stress by transporting the anti-oxidant, ergothioneine [3132]. Another study reported that the expression of OCTN2 was increased in inflamed areas in order to compensate for cellular damage [33]. Therefore, we hypothesized that patients with decreased OCTN1 activity by genetic variants would be susceptible to intestinal inflammation, and would demonstrate more severe CD phenotypes than patients with normal OCTN1 activity. In our previous study, we determined that the OCTN1 haplotypes that contain two variants, g.–1145A>G and g.–248C>G, showed reduced promoter activity [8]. Among the six OCTN1 promoter haplotypes in the present study, five haplotypes (H2 to H6) contained these variants. Therefore, we compared the characteristics or clinical course of patients according to these five haplotypes. We found that the frequency of a penetrating behavior was much higher in patients in the variant group.
There are several limitations in the present study. First, the sample number of our study population was relatively small. In this study, we could not find any significant effect of OCTN1 genotypes or haplotypes on susceptibility to CD. Validation with a larger number of patients of various ethnic groups is necessary to confirm these negative associations. Second, because the analysis of the genotype-phenotype of CD was performed retrospectively in the present study, we could not consider environmental factors in our analysis. However, we compared smoking history in some patients according to the OCTN1 functional haplotypes; there was no significant difference in the number of smokers (30.9% of 62 patients in the variant group vs. 39.4% of 71 patients in the control groups, p=0.290).
In conclusion, we found that OCTN1 functional promoter haplotypes could affect the clinical phenotype of CD in Koreans, although the susceptibility to CD was unrelated to OCTN1 genotypes or haplotypes. To our knowledge, this is the first study to examine the association between CD and genetic variants of the OCTN1 promoter. The presence of these haplotypes may be an important predisposing factor for developing a penetrating behavior in CD.
ACKNOWLEDGEMENTS
This work was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning [2010-0027945 and 2013R1A2A2A01067123], and grants from the National Project for Personalized Genomic Medicine [A111218-PG03] and the Korean Health Technology R&D Project [A120176], Ministry for Health & Welfare, Korea.
Notes
References
1. Tamai I. Pharmacological and pathophysiological roles of carnitine/organic cation transporters (OCTNs: SLC22A4, SLC22A5 and Slc22a21). Biopharm Drug Dispos. 2013; 34:29–44. PMID: 22952014.

2. Urban TJ, Brown C, Castro RA, Shah N, Mercer R, Huang Y, Brett CM, Burchard EG, Giacomini KM. Effects of genetic variation in the novel organic cation transporter, OCTN1, on the renal clearance of gabapentin. Clin Pharmacol Ther. 2008; 83:416–421. PMID: 17609685.

3. Yabuuchi H, Tamai I, Nezu J, Sakamoto K, Oku A, Shimane M, Sai Y, Tsuji A. Novel membrane transporter OCTN1 mediates multispecific, bidirectional, and pH-dependent transport of organic cations. J Pharmacol Exp Ther. 1999; 289:768–773. PMID: 10215651.
4. Peltekova VD, Wintle RF, Rubin LA, Amos CI, Huang Q, Gu X, Newman B, Van Oene M, Cescon D, Greenberg G, Griffiths AM, St George-Hyslop PH, Siminovitch KA. Functional variants of OCTN cation transporter genes are associated with Crohn disease. Nat Genet. 2004; 36:471–475. PMID: 15107849.

5. Gründemann D, Harlfinger S, Golz S, Geerts A, Lazar A, Berkels R, Jung N, Rubbert A, Schömig E. Discovery of the ergothioneine transporter. Proc Natl Acad Sci U S A. 2005; 102:5256–5261. PMID: 15795384.
6. Toh DS, Murray M, Pern Tan K, Mulay V, Grewal T, Lee EJ, Zhou F. Functional analysis of pharmacogenetic variants of human organic cation/carnitine transporter 2 (hOCTN2) identified in Singaporean populations. Biochem Pharmacol. 2011; 82:1692–1699. PMID: 21864509.

7. Tahara H, Yee SW, Urban TJ, Hesselson S, Castro RA, Kawamoto M, Stryke D, Johns SJ, Ferrin TE, Kwok PY, Giacomini KM. Functional genetic variation in the basal promoter of the organic cation/carnitine transporters OCTN1 (SLC22A4) and OCTN2 (SLC22A5). J Pharmacol Exp Ther. 2009; 329:262–271. PMID: 19141711.

8. Park HJ, Choi JH. Identification and functional characterization of novel genetic variations in the OCTN1 promoter. Korean J Physiol Pharmacol. 2014; 18:169–175. PMID: 24757380.
9. Khor B, Gardet A, Xavier RJ. Genetics and pathogenesis of inflammatory bowel disease. Nature. 2011; 474:307–317. PMID: 21677747.

10. Van Limbergen J, Wilson DC, Satsangi J. The genetics of Crohn's disease. Annu Rev Genomics Hum Genet. 2009; 10:89–116. PMID: 19453248.

11. Economou M, Trikalinos TA, Loizou KT, Tsianos EV, Ioannidis JP. Differential effects of NOD2 variants on Crohn's disease risk and phenotype in diverse populations: a metaanalysis. Am J Gastroenterol. 2004; 99:2393–2404. PMID: 15571588.

12. Palomino-Morales RJ, Oliver J, Gómez-García M, López-Nevot MA, Rodrigo L, Nieto A, Alizadeh BZ, Martín J. Association of ATG16L1 and IRGM genes polymorphisms with inflammatory bowel disease: a meta-analysis approach. Genes Immun. 2009; 10:356–364. PMID: 19491842.

13. Parkes M, Barrett JC, Prescott NJ, Tremelling M, Anderson CA, Fisher SA, Roberts RG, Nimmo ER, Cummings FR, Soars D, Drummond H, Lees CW, Khawaja SA, Bagnall R, Burke DA, Todhunter CE, Ahmad T, Onnie CM, McArdle W, Strachan D, Bethel G, Bryan C, Lewis CM, Deloukas P, Forbes A, Sanderson J, Jewell DP, Satsangi J, Mansfield JC, Cardon L, Mathew CG. Wellcome Trust Case Control Consortium. Sequence variants in the autophagy gene IRGM and multiple other replicating loci contribute to Crohn's disease susceptibility. Nat Genet. 2007; 39:830–832. PMID: 17554261.

14. Martinez A, Martin MC, Mendoza JL, Taxonera C, Diaz-Rubio M, de la Concha EG, Urcelay E. Association of the organic cation transporter OCTN genes with Crohn's disease in the Spanish population. Eur J Hum Genet. 2006; 14:222–226. PMID: 16333318.

15. Tomer G, Wetzler G, Keddache M, Denson LA. Polymorphisms in the IBD5 locus are associated with Crohn disease in pediatric Ashkenazi Jewish patients. J Pediatr Gastroenterol Nutr. 2009; 48:531–537. PMID: 19412005.

16. Leung E, Hong J, Fraser AG, Merriman TR, Vishnu P, Krissansen GW. Polymorphisms in the organic cation transporter genes SLC22A4 and SLC22A5 and Crohn's disease in a New Zealand Caucasian cohort. Immunol Cell Biol. 2006; 84:233–236. PMID: 16519742.
17. Li M, Gao X, Guo CC, Wu KC, Zhang X, Hu PJ. OCTN and CARD15 gene polymorphism in Chinese patients with inflammatory bowel disease. World J Gastroenterol. 2008; 14:4923–4927. PMID: 18756601.

18. Yamazaki K, Takazoe M, Tanaka T, Ichimori T, Saito S, Iida A, Onouchi Y, Hata A, Nakamura Y. Association analysis of SLC22A4, SLC22A5 and DLG5 in Japanese patients with Crohn disease. J Hum Genet. 2004; 49:664–668. PMID: 15503241.

19. Tosa M, Negoro K, Kinouchi Y, Abe H, Nomura E, Takagi S, Aihara H, Oomori S, Sugimura M, Takahashi K, Hiwatashi N, Takahashi S, Shimosegawa T. Lack of association between IBD5 and Crohn's disease in Japanese patients demonstrates population-specific differences in inflammatory bowel disease. Scand J Gastroenterol. 2006; 41:48–53. PMID: 16373276.
20. Barrett JC, Hansoul S, Nicolae DL, Cho JH, Duerr RH, Rioux JD, Brant SR, Silverberg MS, Taylor KD, Barmada MM, Bitton A, Dassopoulos T, Datta LW, Green T, Griffiths AM, Kistner EO, Murtha MT, Regueiro MD, Rotter JI, Schumm LP, Steinhart AH, Targan SR, Xavier RJ, Libioulle C, Sandor C, Lathrop M, Belaiche J, Dewit O, Gut I, Heath S, Laukens D, Mni M, Rutgeerts P, Van Gossum A, Zelenika D, Franchimont D, Hugot JP, de Vos M, Vermeire S, Louis E, Cardon LR, Anderson CA, Drummond H, Nimmo E, Ahmad T, Prescott NJ, Onnie CM, Fisher SA, Marchini J, Ghori J, Bumpstead S, Gwilliam R, Tremelling M, Deloukas P, Mansfield J, Jewell D, Satsangi J, Mathew CG, Parkes M, Georges M, Daly MJ. NIDDK IBD Genetics Consortium. Belgian-French IBD Consortium. Wellcome Trust Case Control Consortium. Genome-wide association defines more than 30 distinct susceptibility loci for Crohn's disease. Nat Genet. 2008; 40:955–962. PMID: 18587394.

21. Franke A, McGovern DP, Barrett JC, Wang K, Radford-Smith GL, Ahmad T, Lees CW, Balschun T, Lee J, Roberts R, Anderson CA, Bis JC, Bumpstead S, Ellinghaus D, Festen EM, Georges M, Green T, Haritunians T, Jostins L, Latiano A, Mathew CG, Montgomery GW, Prescott NJ, Raychaudhuri S, Rotter JI, Schumm P, Sharma Y, Simms LA, Taylor KD, Whiteman D, Wijmenga C, Baldassano RN, Barclay M, Bayless TM, Brand S, Buning C, Cohen A, Colombel JF, Cottone M, Stronati L, Denson T, De Vos M, D'Inca R, Dubinsky M, Edwards C, Florin T, Franchimont D, Gearry R, Glas J, Van Gossum A, Guthery SL, Halfvarson J, Verspaget HW, Hugot JP, Karban A, Laukens D, Lawrance I, Lemann M, Levine A, Libioulle C, Louis E, Mowat C, Newman W, Panes J, Phillips A, Proctor DD, Regueiro M, Russell R, Rutgeerts P, Sanderson J, Sans M, Seibold F, Steinhart AH, Stokkers PC, Torkvist L, Kullak-Ublick G, Wilson D, Walters T, Targan SR, Brant SR, Rioux JD, D'Amato M, Weersma RK, Kugathasan S, Griffiths AM, Mansfield JC, Vermeire S, Duerr RH, Silverberg MS, Satsangi J, Schreiber S, Cho JH, Annese V, Hakonarson H, Daly MJ, Parkes M. Genome-wide meta-analysis increases to 71 the number of confirmed Crohn's disease susceptibility loci. Nat Genet. 2010; 42:1118–1125. PMID: 21102463.

22. Jostins L, Ripke S, Weersma RK, Duerr RH, McGovern DP, Hui KY, Lee JC, Schumm LP, Sharma Y, Anderson CA, Essers J, Mitrovic M, Ning K, Cleynen I, Theatre E, Spain SL, Raychaudhuri S, Goyette P, Wei Z, Abraham C, Achkar JP, Ahmad T, Amininejad L, Ananthakrishnan AN, Andersen V, Andrews JM, Baidoo L, Balschun T, Bampton PA, Bitton A, Boucher G, Brand S, Buning C, Cohain A, Cichon S, D'Amato M, De Jong D, Devaney KL, Dubinsky M, Edwards C, Ellinghaus D, Ferguson LR, Franchimont D, Fransen K, Gearry R, Georges M, Gieger C, Glas J, Haritunians T, Hart A, Hawkey C, Hedl M, Hu X, Karlsen TH, Kupcinskas L, Kugathasan S, Latiano A, Laukens D, Lawrance IC, Lees CW, Louis E, Mahy G, Mansfield J, Morgan AR, Mowat C, Newman W, Palmieri O, Ponsioen CY, Potocnik U, Prescott NJ, Regueiro M, Rotter JI, Russell RK, Sanderson JD, Sans M, Satsangi J, Schreiber S, Simms LA, Sventoraityte J, Targan SR, Taylor KD, Tremelling M, Verspaget HW, De Vos M, Wijmenga C, Wilson DC, Winkelmann J, Xavier RJ, Zeissig S, Zhang B, Zhang CK, Zhao H, Silverberg MS, Annese V, Hakonarson H, Brant SR, Radford-Smith G, Mathew CG, Rioux JD, Schadt EE, Daly MJ, Franke A, Parkes M, Vermeire S, Barrett JC, Cho JH. International IBD Genetics Consortium (IIBDGC). Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature. 2012; 491:119–124. PMID: 23128233.

23. Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006; 55:749–753. PMID: 16698746.

24. Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, Benchimol EI, Panaccione R, Ghosh S, Barkema HW, Kaplan GG. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012; 142:46–54.e42. quiz e30. PMID: 22001864.

25. Moon CM, Shin DJ, Son NH, Shin ES, Hong SP, Kim TI, Kim WH, Cheon JH. Genetic variants in the IL12B gene are associated with inflammatory bowel diseases in the Korean population. J Gastroenterol Hepatol. 2013; 28:1588–1594. PMID: 23573954.
26. Yang SK, Hong M, Zhao W, Jung Y, Baek J, Tayebi N, Kim KM, Ye BD, Kim KJ, Park SH, Lee I, Lee EJ, Kim WH, Cheon JH, Kim YH, Jang BI, Kim HS, Choi JH, Koo JS, Lee JH, Jung SA, Lee YJ, Jang JY, Shin HD, Kang D, Youn HS, Liu J, Song K. Genome-wide association study of Crohn's disease in Koreans revealed three new susceptibility loci and common attributes of genetic susceptibility across ethnic populations. Gut. 2014; 63:80–87. PMID: 23850713.

27. Yang DH, Yang SK, Song K, Hong M, Park SH, Lee HS, Kim JB, Lee HJ, Park SK, Jung KW, Kim KJ, Ye BD, Byeon JS, Myung SJ, Kim JH, Shin US, Yu CS, Lee I. TNFSF15 is an independent predictor for the development of Crohn's disease-related complications in Koreans. J Crohns Colitis. 2014; 8:1315–1326. PMID: 24835165.

28. Urban TJ, Yang C, Lagpacan LL, Brown C, Castro RA, Taylor TR, Huang CC, Stryke D, Johns SJ, Kawamoto M, Carlson EJ, Ferrin TE, Burchard EG, Giacomini KM. Functional effects of protein sequence polymorphisms in the organic cation/ergothioneine transporter OCTN1 (SLC22A4). Pharmacogenet Genomics. 2007; 17:773–782. PMID: 17700366.

29. Park HJ, Jung ES, Kong KA, Park EM, Cheon JH, Choi JH. Identification of OCTN2 variants and their association with phenotypes of Crohn's disease in a Korean population. Sci Rep. 2016; 6:22887. PMID: 26965072.

30. Vermeire S, Pierik M, Hlavaty T, Claessens G, van Schuerbeeck N, Joossens S, Ferrante M, Henckaerts L, Bueno de Mesquita M, Vlietinck R, Rutgeerts P. Association of organic cation transporter risk haplotype with perianal penetrating Crohn's disease but not with susceptibility to IBD. Gastroenterology. 2005; 129:1845–1853. PMID: 16344053.

31. Kato Y, Kubo Y, Iwata D, Kato S, Sudo T, Sugiura T, Kagaya T, Wakayama T, Hirayama A, Sugimoto M, Sugihara K, Kaneko S, Soga T, Asano M, Tomita M, Matsui T, Wada M, Tsuji A. Gene knockout and metabolome analysis of carnitine/organic cation transporter OCTN1. Pharm Res. 2010; 27:832–840. PMID: 20224991.

32. Sakrak O, Kerem M, Bedirli A, Pasaoglu H, Akyurek N, Ofluoglu E, Gültekin FA. Ergothioneine modulates proinflammatory cytokines and heat shock protein 70 in mesenteric ischemia and reperfusion injury. J Surg Res. 2008; 144:36–42. PMID: 17603080.

33. Fujiya M, Musch MW, Nakagawa Y, Hu S, Alverdy J, Kohgo Y, Schneewind O, Jabri B, Chang EB. The Bacillus subtilis quorum-sensing molecule CSF contributes to intestinal homeostasis via OCTN2, a host cell membrane transporter. Cell Host Microbe. 2007; 1:299–308. PMID: 18005709.

Fig. 1
Kaplan-Meier curve for developing a penetrating disease behavior in Korean CD patients during follow-up.
The log-rank test was performed between the OCTN1 variant (solid line) and control (dashed line) groups (p=0.008).
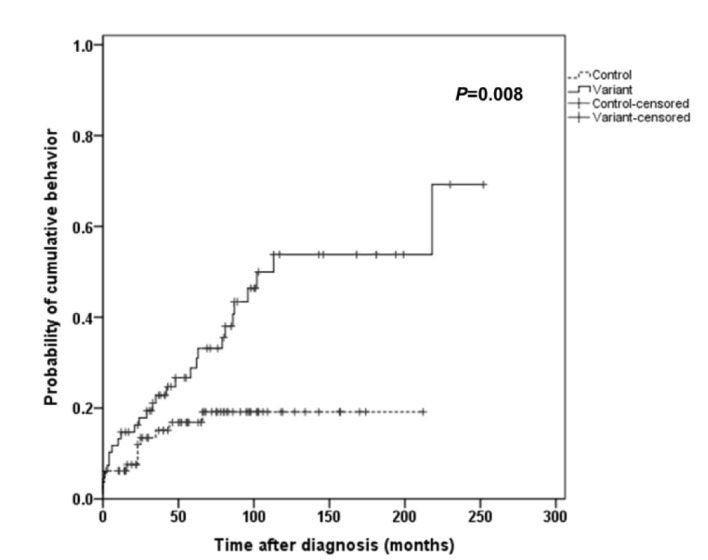
Table 3
Demographic and clinical characteristics of patients according to OCTN1 haplotypes
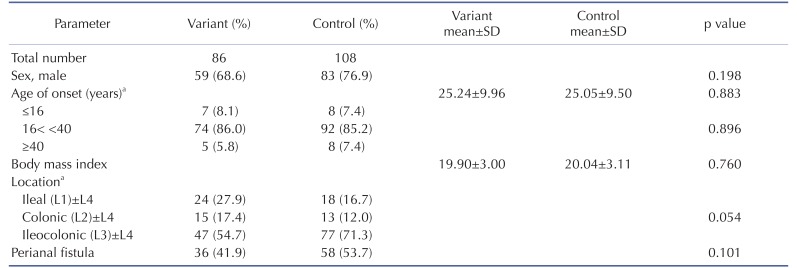
aAccording to the Montreal Classification [23].
L4 indicates upper gastrointestinal involvement.
SD, standard deviation.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download