1. Guyenet PG. The sympathetic control of blood pressure. Nat Rev Neurosci. 2006; 7:335–346. PMID:
16760914.

2. Pilowsky PM, Goodchild AK. Baroreceptor reflex pathways and neurotransmitters: 10 years on. J Hypertens. 2002; 20:1675–1688. PMID:
12195099.

3. Yates BJ. Vestibular influences on the sympathetic nervous system. Brain Res Brain Res Rev. 1992; 17:51–59. PMID:
1638275.

4. Yates BJ, Miller AD. Properties of sympathetic reflexes elicited by natural vestibular stimulation: implications for cardiovascular control. J Neurophysiol. 1994; 71:2087–2092. PMID:
7931504.

5. Normand H, Etard O, Denise P. Otolithic and tonic neck receptors control of limb blood flow in humans. J Appl Physiol (1985). 1997; 82:1734–1738. PMID:
9173934.
6. Porter JD, Balaban CD. Connections between the vestibular nuclei and brain stem regions that mediate autonomic function in the rat. J Vestib Res. 1997; 7:63–76. PMID:
9057160.

7. Balaban CD, Beryozkin G. Vestibular nucleus projections to nucleus tractus solitarius and the dorsal motor nucleus of the vagus nerve: potential substrates for vestibulo-autonomic interactions. Exp Brain Res. 1994; 98:200–212. PMID:
8050507.

8. Yates BJ, Grélot L, Kerman IA, Balaban CD, Jakus J, Miller AD. Organization of vestibular inputs to nucleus tractus solitarius and adjacent structures in cat brain stem. Am J Physiol. 1994; 267:R974–R983. PMID:
7524372.
9. Holstein GR, Friedrich VL Jr, Kang T, Kukielka E, Martinelli GP. Direct projections from the caudal vestibular nuclei to the ventrolateral medulla in the rat. Neuroscience. 2011; 175:104–117. PMID:
21163335.

10. Kalia M, Mesulam MM. Brain stem projections of sensory and motor components of the vagus complex in the cat: II. Laryngeal, tracheobronchial, pulmonary, cardiac, and gastrointestinal branches. J Comp Neurol. 1980; 193:467–508. PMID:
7440778.

11. Jiang X, Li LW, Lan Y, Yang YZ, Jin GS, Kim MS, Park BR, Jin YZ. Comparative analysis of vestibular receptor and baroreceptor inputs to the nucleus tractus solitarius following acute hypotension in conscious rats. Neurosci Lett. 2014; 563:70–74. PMID:
24486893.

12. Dampney RA. Functional organization of central pathways regulating the cardiovascular system. Physiol Rev. 1994; 74:323–364. PMID:
8171117.

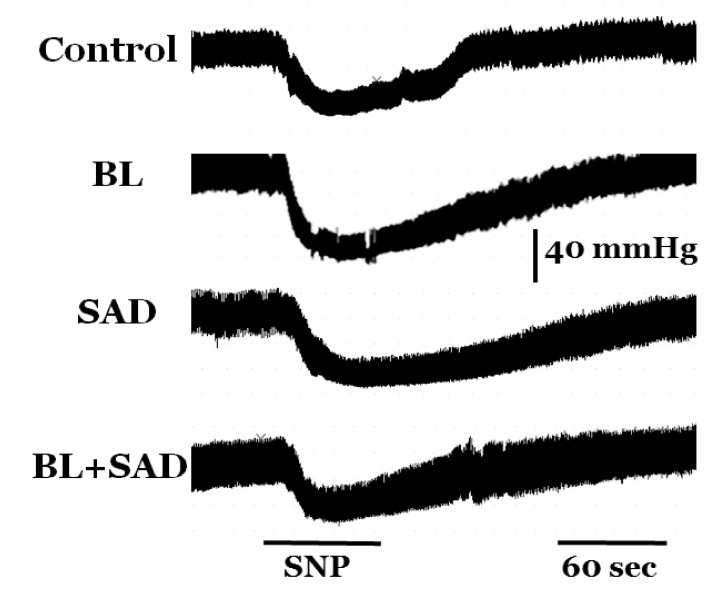
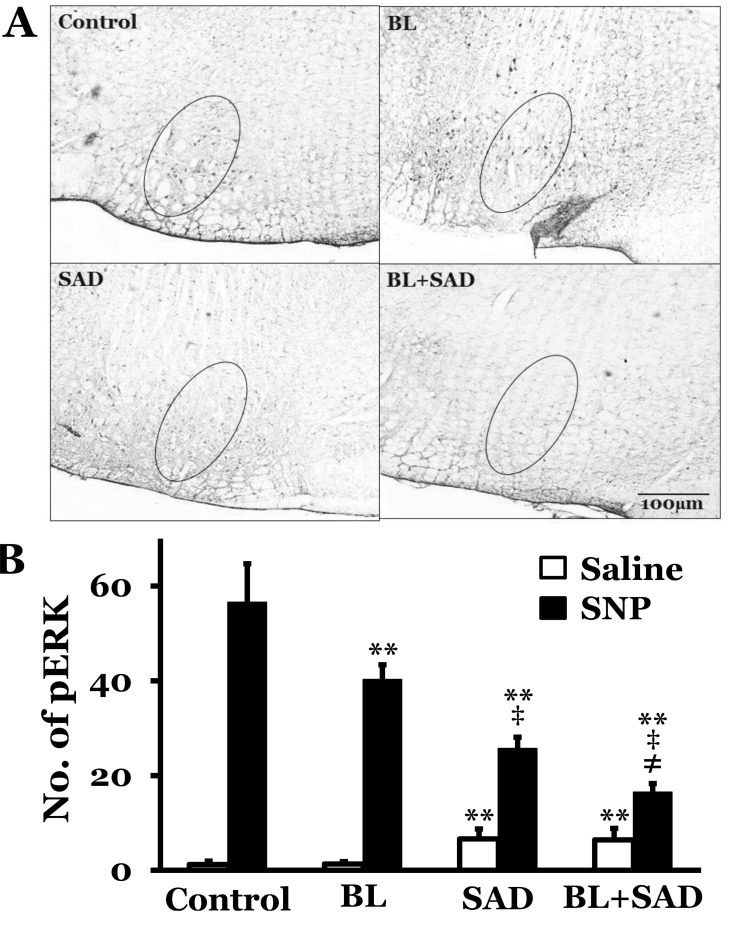
13. Lan Y, Yang YZ, Jiang X, Li LW, Jin GS, Kim MS, Park BR, Jin YZ. Additive role of the vestibular end organ and baroreceptors on the regulation of blood pressure in rats. Korean J Physiol Pharmacol. 2013; 17:367–373. PMID:
23946697.

14. Morrison SF. Glutamate transmission in the rostral ventrolateral medullary sympathetic premotor pathway. Cell Mol Neurobiol. 2003; 23:761–772. PMID:
14514030.
15. Aoki M, Sakaida Y, Tanaka K, Mizuta K, Ito Y. Evidence for vestibular dysfunction in orthostatic hypotension. Exp Brain Res. 2012; 217:251–259. PMID:
22205233.

16. Smit AA, Halliwill JR, Low PA, Wieling W. Pathophysiological basis of orthostatic hypotension in autonomic failure. J Physiol. 1999; 519(Pt 1):1–10. PMID:
10432334.

17. Doba N, Reis DJ. Role of the cerebellum and the vestibular apparatus in regulation of orthostatic reflexes in the cat. Circ Res. 1974; 40:9–18. PMID:
4543723.

18. Mori RL, Cotter LA, Arendt HE, Olsheski CJ, Yates BJ. Effects of bilateral vestibular nucleus lesions on cardiovascular regulation in conscious cats. J Appl Physiol (1985). 2005; 98:526–533. PMID:
15475594.

19. Sgambato V, Pagès C, Rogard M, Besson MJ, Caboche J. Extracellular signal-regulated kinase (ERK) controls immediate early gene induction on corticostriatal stimulation. J Neurosci. 1998; 18:8814–8825. PMID:
9786988.

20. Morgan JI, Curran T. Stimulus-transcription coupling in the nervous system: involvement of the inducible proto-oncogenes fos and jun. Annu Rev Neurosci. 1991; 14:421–451. PMID:
1903243.

21. Koh YH, Ruiz-Canada C, Gorczyca M, Budnik V. The Ras1-mitogen-activated protein kinase signal transduction pathway regulates synaptic plasticity through fasciclin II-mediated cell adhesion. J Neurosci. 2002; 22:2496–2504. PMID:
11923414.

22. Xia Z, Dudek H, Miranti CK, Greenberg ME. Calcium influx via the NMDA receptor induces immediate early gene transcription by a MAP kinase/ERK-dependent mechanism. J Neurosci. 1996; 16:5425–5436. PMID:
8757255.

23. Bobrovskaya L, Odell A, Leal RB, Dunkley PR. Tyrosine hydroxylase phosphorylation in bovine adrenal chromaffin cells: the role of MAPKs after angiotensin II stimulation. J Neurochem. 2001; 78:490–498. PMID:
11483651.

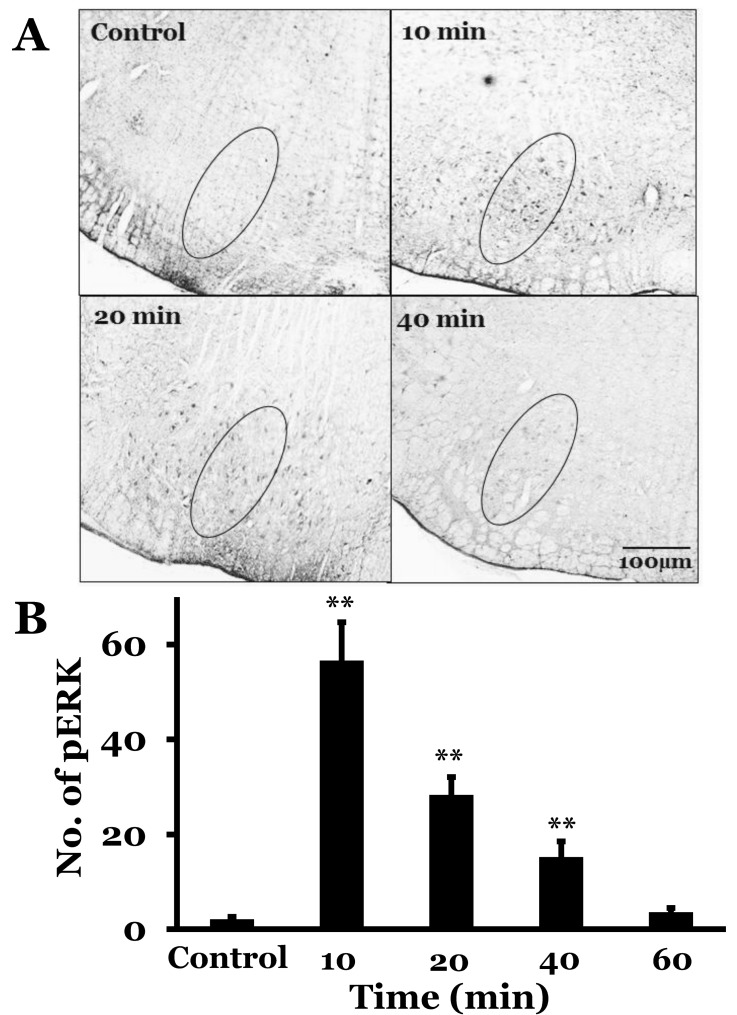
24. Kim MS, Choi DO, Choi MA, Kim JH, Kim KY, Lee MY, Rhee JK, Chun SW, Park BR. Immunohistochemical detection of phosphorylated form of extracellular signal-regulated kinase 1/2 in rat vestibular nuclei following hemorrhagic hypotension. Neurosci Lett. 2004; 360:49–52. PMID:
15082176.

25. Hunt MA, Miller SW, Nielson HC, Horn KM. Intratympanic injection of sodium arsanilate (atoxyl) solution results in postural changes consistent with changes described for labyrinthectomized rats. Behav Neurosci. 1987; 101:427–428. PMID:
3606813.

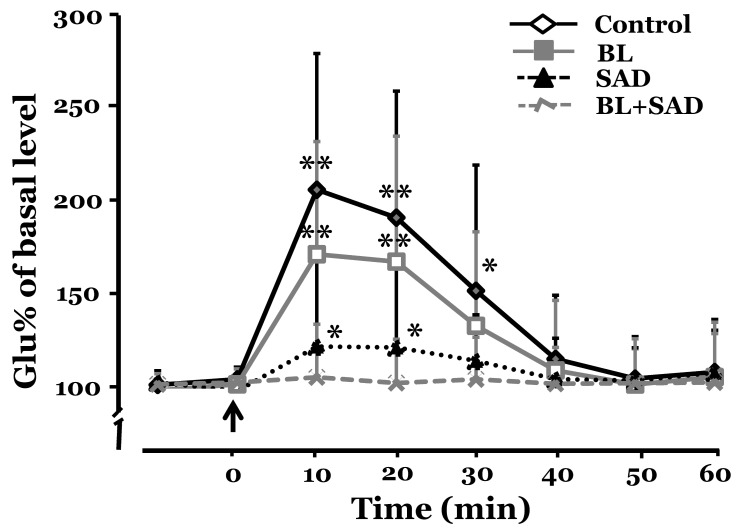
26. Choi MA, Lee JH, Hwang JH, Choi SJ, Kim MS, Park BR. Signaling pathway of glutamate in the vestibular nuclei following acute hypotension in rats. Brain Res. 2008; 1229:111–117. PMID:
18639534.

27. Wei S, Lei M, Tong M, Ding J, Han Q, Xiao M. Acute baroreceptor unloading evokes Fos expression in anesthetized rat brain. Brain Res Bull. 2008; 76:63–69. PMID:
18395612.

28. Paxinos G, Watson C. The rat brain in stereotaxic coordinates. Orlando, FL, USA: Academic Press;2007.
29. Yu HL, An Y, Jiang HY, Jin QH, Jin YZ. Changes of amino acid concentrations in the rat medial vestibular nucleus following unilateral labyrinthectomy. Sheng Li Xue Bao. 2007; 59:71–78. PMID:
17294045.
30. Jin QH, Ueda Y, Ishizuka Y, Kunitake T, Kannan H. Cardiovascular changes induced by central hypertonic saline are accompanied by glutamate release in awake rats. Am J Physiol Regul Integr Comp Physiol. 2001; 281:R1224–R1231. PMID:
11557631.

31. Pirodda A, Brandolini C, Carlo Modugno G. Hypotension associated with autonomic dysfunction: a possible cause of vertigo? Med Hypotheses. 2004; 63:1086. PMID:
15504583.

32. Freeman R. Clinical practice. Neurogenic orthostatic hypotension. N Engl J Med. 2008; 358:615–624. PMID:
18256396.
33. Cornish KG, Gilmore JP. Sino-aortic denervation in the monkey. J Physiol. 1985; 360:423–432. PMID:
3989722.

34. Murad F. Cyclic guanosine monophosphate as a mediator of vasodilation. J Clin Invest. 1986; 78:1–5. PMID:
2873150.

35. Takamura H, Ichisaka S, Watanabe K, Toigawa M, Hata Y. Effects of anesthesia on immunohistochemical detection of phosphorylated extracellular signal-regulated kinase in cerebral cortex. J Neurosci Methods. 2008; 170:300–304. PMID:
18294698.

36. Guo ZL, Lai HC, Longhurst JC. Medullary pathways involved in cardiac sympathoexcitatory reflexes in the cat. Brain Res. 2002; 925:55–66. PMID:
11755900.

37. Park BR, Kim MS, Kim JH, Jin YZ. Effects of acute hypotension on neuronal activity in the medial vestibular nuclei of rats. Neuroreport. 2001; 12:3821–3824. PMID:
11726802.

38. Kim MS, Kim JH, Kry D, Choi MA, Choi DO, Cho BG, Jin YZ, Lee SH, Park BR. Effects of acute hypotension on expression of cFos-like protein in the vestibular nuclei of rats. Brain Res. 2003; 962:111–121. PMID:
12543461.

39. Singewald N, Zhou GY, Chen F, Philippu A. Corticotropinreleasing factor modulates basal and stress-induced excitatory amino acid release in the locus coeruleus of conscious rats. Neurosci Lett. 1996; 204:45–48. PMID:
8929974.

40. Zhou W, Fu LW, Guo ZL, Longhurst JC. Role of glutamate in the rostral ventrolateral medulla in acupuncture-related modulation of visceral reflex sympathoexcitation. Am J Physiol Heart Circ Physiol. 2007; 292:H1868–H1875. PMID:
17158649.

41. Len WB, Chan JY. Glutamatergic projection to RVLM mediates suppression of reflex bradycardia by parabrachial nucleus. Am J Physiol. 1999; 276:H1482–H1492. PMID:
10330230.
42. Krassioukov AV, Weaver LC. Connections between the pontine reticular formation and rostral ventrolateral medulla. Am J Physiol. 1993; 265:H1386–H1392. PMID:
8238426.

43. Barman SM, Gebber GL, Orer HS. Medullary lateral tegmental field: an important source of basal sympathetic nerve discharge in the cat. Am J Physiol Regul Integr Comp Physiol. 2000; 278:R995–R1004. PMID:
10749789.
44. Dampney RA, Horiuchi J, Tagawa T, Fontes MA, Potts PD, Polson JW. Medullary and supramedullary mechanisms regulating sympathetic vasomotor tone. Acta Physiol Scand. 2003; 177:209–218. PMID:
12608991.

45. Holstein GR, Friedrich VL Jr, Martinelli GP. Projection neurons of the vestibulo-sympathetic reflex pathway. J Comp Neurol. 2014; 522:2053–2074. PMID:
24323841.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download