INTRODUCTION
METHODS
Reagents and antibodies
Cell culture
Establishment of cisplatin-resistant variant cells
RT-PCR
Western blot analysis
Clonogenic assay
Cell viability assay
ELISA
Statistical analysis
RESULTS
Long-term cisplatin exposure results in acquisition of resistance in human lung cancer cells
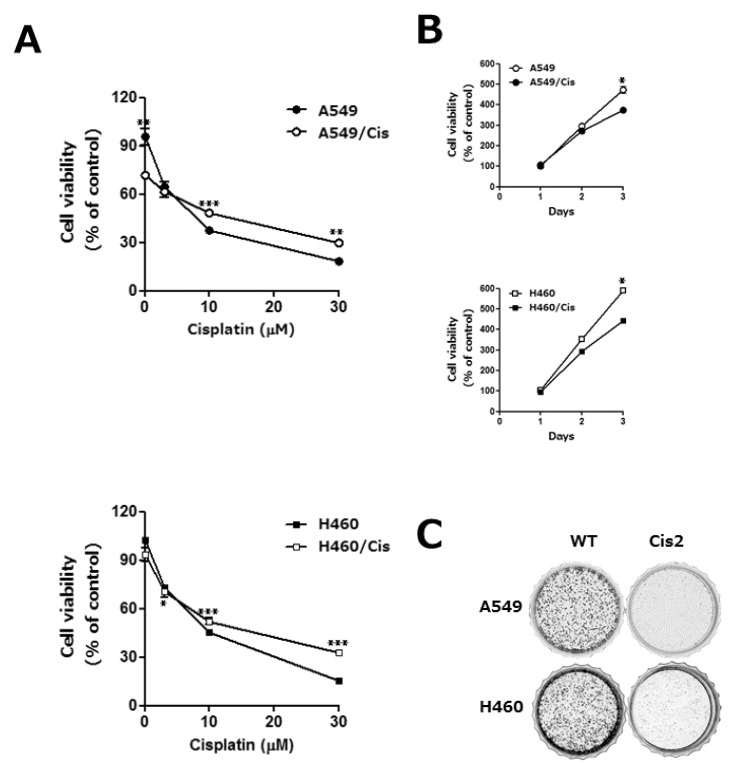 | Fig. 1The acquisition of cisplatin resistance results in the reduction of proliferative capability in human lung cancer cells. A549 and H460 cells were exposed to increasing concentrations of cisplatin in a stepwise manner, which resulted in the development of their variants with cisplatin resistant, A549/Cis and H460/Cis, respectively. (A) Both parental, A549 and H460, and each of chemoresistant variants, A549/Cis and H460/Cis, were treated with the indicated concentrations of cisplatin for 24 h. Cell viability was measured by CCK-8 assay. Each error bar represents mean±SD of at least three independent experiments. The asterisks indicate the significant difference compared to the control value (*p<0.05 H460 vs H460/Cis at 3 µM cisplatin, **p<0.01 A549 vs A549/Cis at 0, 30 µM cisplatin, ***p<0.001 A549 vs A549/Cis at 10 µM cisplatin and H460 vs H460/Cis at 10, 30 µM cisplatin). (B) Cells (1×103 cells/well) were seeded onto 96-well plates and allowed to grow for 72 h. The proliferation rate was determined by CCK-8 assay. Data are expressed as mean±SD from three independent experiments. Data are expressed as mean±SD of three independent experiments. The asterisks indicate the significant difference compared to the control value (*p<0.001 A549 vs A549/Cis and H460 vs H460/Cis at day 3) (C) Cells (2×103 cells/dish) were seeded onto 35 mm dishes and allowed to grow for 7 to 10 days until to form colonies. The colonies were visualized by crystal violet staining. The data shown is representative of at least three independent experiments. |
Acquisition of cisplatin resistance gives rise to the reduction of proliferative capability
EGCG inhibits proliferation of both parental and cisplatin resistant cells
 | Fig. 2EGCG inhibits proliferation of both parental and cisplatin resistant lung cancer cells. (A) Cells (3×103 cells/dish) were seeded onto 100 mm dishes, grown overnight and treated with 80 µM EGCG for 24 h. After treatment, cells were harvested, stained with tryphan blue, and the number of viable cells was counted. Data are represented as mean±SD of at least three independent experiments. The asterisks indicate the significant difference compared to the control value (*p<0.005 A549 vs A549/Cis and **p<0.0001 H460 vs H460/Cis at 80 µM EGCG). (B) Cells (2×103 cells/dish) were seeded onto 35 mm dishes and allowed to grow in the absence or presence of 80 µM EGCG for 7 to 10 days. The colonies were visualized by crystal violet staining. The data shown is representative of at least three independent experiments. |
IL-6/STAT 3 axis is not associated with the anti-proliferative effect of EGCG
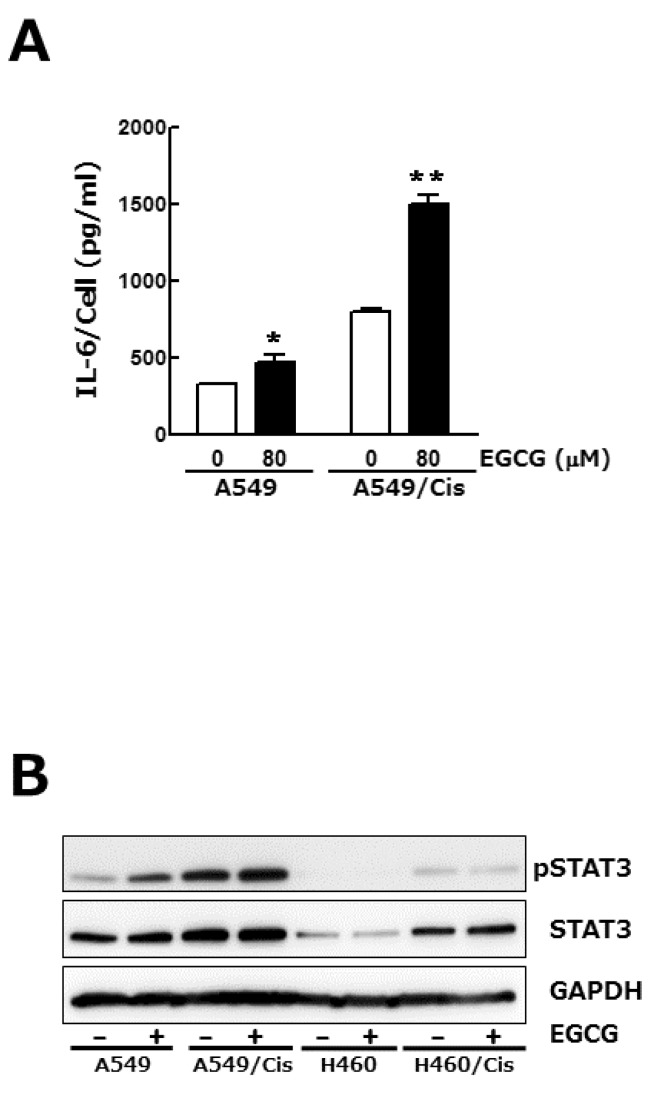 | Fig. 3IL-6/STAT 3 axis is not associated with the anti-proliferative effect of EGCG. Cells (3×103 cells/dish) were seeded onto 100 mm dishes, grown overnight and treated with 80 µM EGCG for 24 h. (A) Conditioned media were harvested and used for IL-6 ELISA. To assess its production per cell, the total amount of IL-6 was normalized by the number of viable cells. Results are from three independent experiments. Data are expressed as the mean±SD of triplicate samples conducted in three independent experiments. The asterisks indicate the significant difference compared to the control value (*p<0.05 A549 vs A549/EGCG and **p<0.001 A549/Cis vs A549/Cis/EGCG). (B) In parallel, Western blot analysis was conducted to determine the phosphorylation status of STAT3. The level of total STAT3, an internal control, and of GAPDH, a loading control, was also detected. The data shown is representative of three independent experiments. |
EGCG inhibits the expression of Axl and Tyro 3 receptor tyrosine kinases
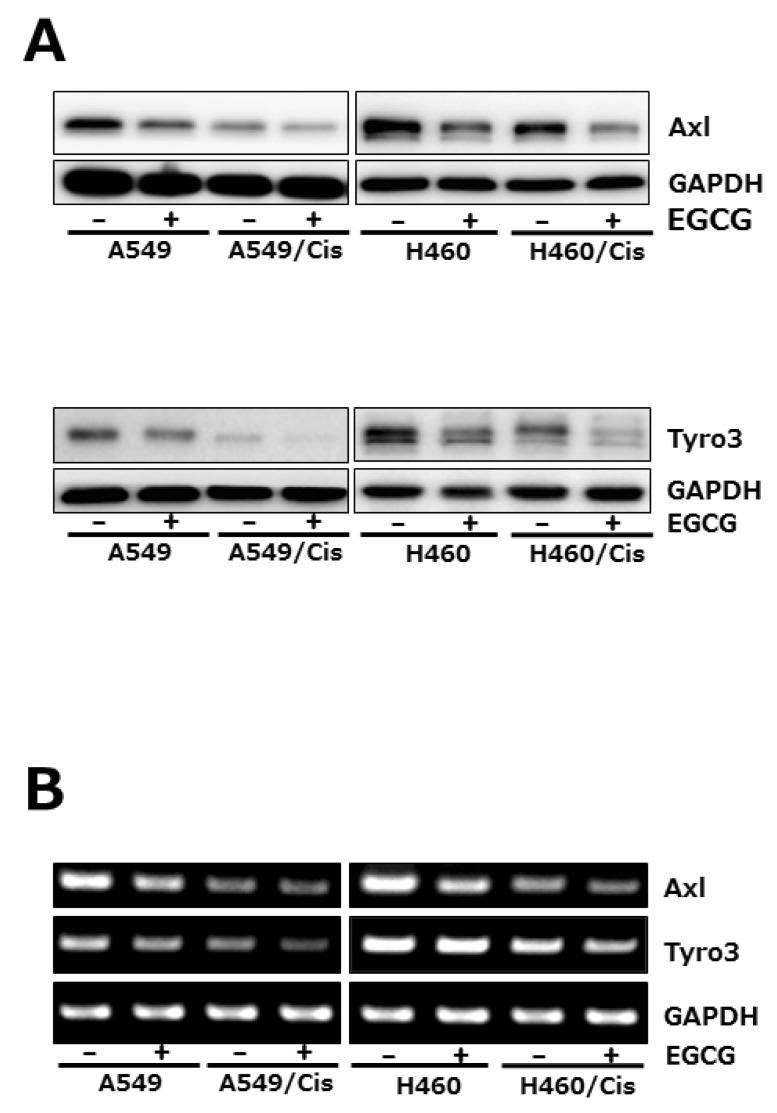 | Fig. 4EGCG suppresses the expression of Axl and Tyro 3 RTKs. Cells (3×103 cells/dish) were seeded onto 100 mm dishes, grown overnight and treated with 80 µM EGCG for 24 h. (A) The protein level of Axl and Tyro 3 was assessed by Western blot analysis to determine the effect of EGCG on their expression. GAPDH was used as a loading control. Results are from three independent experiments. (B) For RT-PCR, total RNAs from those cells were isolated and used for analysis of Axl and Tyro 3 mRNA expression. The level of Axl and Tyro 3 mRNA was normalized to that of GAPDH. The data shown is representative of three independent experiments. |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download