Abstract
Cancer stem cells (CSCs) are often characterized by the elevated expression of drug-resistance related stem-cell surface markers, such as CD133 and ABCG2. Recently, we reported that CSCs have a high level of expression of the IL-6 receptor (IL-6R). The purpose of this study was to investigate the effect of anticancer drugs on the expression of the drug resistance-related cancer stem cell markers, ABCG2, IL-6R, and CD133 in non-small cell lung cancer (NSCLC) cell lines. A549, H460, and H23 NSCLC cell lines were treated with the anticancer drugs 5-fluorouracil (5-FU; 25 µg/ml) and methotrexate (MTX; 50 µg/ml), and the expression of putative CSC markers was analyzed by fluorescent activated cell sorter (FACS) and the gene expression level of abcg2, il-6r and cd133 by reverse transcriptasepolymerase chain reaction (RT-PCR). We found that the fraction of ABCG2-positive(+) cells was significantly increased by treatment with both 5-FU and MTX in NSCLC cells, and the elevation of abcg2, il-6r and cd133 expressions in response to these drugs was also confirmed using RT-PCR. Also, the number of IL-6R(+) cells was increased by MTX in the 3 cell lines mentioned and increased by 5-FU in the H460 cell line. The number of CD133(+) cells was also significantly increased by both 5-FU and MTX treatment in all of the cell lines tested. These results indicate that 5-FU and MTX considerably enhance the expression of drug-resistance related CSC markers in NSCLC cell lines. Thus, we suggest that antimetabolite cancer drugs, such as 5-FU and MTX, can lead to the propagation of CSCs through altering the expression of CSC markers.
The cancer stem cell (CSC) theory suggests that tumors contain rare subpopulations of undifferentiated cells that possess stem cell properties, such as self-renewal, heterogeneity, and resistance to anticancer drugs [1,2]. CSCs show resistance to chemotherapy because of their low proliferation rate and resistance mechanisms, such as the expression of multidrug transporters of the ATP-binding cassette (ABC) superfamily. The transporter ABCG2 is known to promote resistance to multiple drugs and has been observed in various types of CSCs [3-5]. Due to the drug resistant properties of CSCs, many anticancer drugs show transient effects and often do not improve patient prognosis. Even therapies that cause complete tumor regression may spare CSCs, allowing for regeneration of the tumor. The pentaspan protein, CD133, is a universal marker of organ-specific stem cells and tumor-initiating cells. CD133 was originally identified as a marker for CD34(+) hematopoietic stem and progenitor cells [6] and has been used to identify CSCs in several types of cancer [7-11]. Lung cancer is the leading cause of cancer death in many countries [12]. Poor prognosis of lung cancer patients is due mainly to poor response, early relapse, and metastasis after treatment with chemotherapy and radiotherapy. Several studies have demonstrated that CD133(+) lung cancer cells possess features of stemness and display a higher tumorigenic potential than CD133-negative(-) cells [13-15]. CD133 expression has also been linked to a drug-resistant phenotype in lung cancer patients [16].
In our previous study, lung CSCs, isolated with Hoechst 33342, were found to express significantly higher levels of the IL-6 receptor (IL-6R) and abcg2 [17]. IL-6/IL-6R signaling has been well documented to play a role in the growth and malignancy of cancer. The aberrant production and increased secretion of IL-6 in cancer patients is linked to tumor progression and poor prognosis in many cancer types, including lung cancer [18-20]. IL-6 is also known to promote multi-drug resistance to chemotherapy [21]. Recently, it was reported that the expression of IL-6 and IL-6R in CSCs was much greater than in non-CSCs [11,22]. These findings suggest that IL-6R is a potential CSC marker related to the drug resistance phenotype of some tumors. However, the expression of CSC markers and mechanisms by which CSCs acquire resistance to many anticancer drugs remains unknown. Therefore, we carried out this study to assess the effect of anticancer drugs on the expression of the drug resistance-related cancer stem cell markers, ABCG2, IL-6R, and CD133 in non-small cell lung cancer (NSCLC) cell lines.
NSCLC cell lines, A549, H460, and H23, were purchased from the Korean Cell Line Bank (KCLB; Seoul, Korea). Cells were grown in RPMI-1640 medium (Gibco, CA, USA), with 10% fetal bovine serum (Gibco, CA, USA) and 1% penicillin/streptomycin (Gibco, CA, USA) in a humidified atmosphere at 37℃ with 5% CO2 as recommended by the KLCB.
The anticancer drugs, 5-FU and MTX, were purchased from Sigma Aldrich Inc. (MO, USA) and dissolved in phosphate buffered saline (pH 7.4). NSCLC cells were seeded in a 6-well cell culture plate (Corning Inc., NY, USA) and incubated overnight in a humidified atmosphere at 37℃ with 5% CO2. Cells were then incubated with 5-FU (25 µg/ml) or MTX (50 µg/ml) in media for 6, 12, and 48 hrs prior to RT-PCR and for 24 hrs prior to FACS analysis.
A549, H460, and H23 NSCLC cells were harvested and suspended at a density of 1×106 cells/ml in FACS buffer containing PBS (pH 7.4) with 2% fetal bovine serum (FBS). The cells were incubated with PE-anti-ABCG2 (Abcam, MA, USA), FITC-anti-IL-6R (Abcam, MA, USA), and PE-anti-CD133 (Miltentyi Biotec, Bergisch Gladbach, Germany) antibodies for 30 min. After washing the cells three times with FACS buffer, the expression of ABCG2, IL-6R, and CD133 were analyzed by fluorescent activated cell sorter (FACScalibur; BD, NJ, USA).
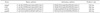
We performed semi-quantitative reverse transcriptasepolymerase chain reaction (RT-PCR) to assess the effect of the anticancer drugs on mRNA expressions of abcg2, il-6r, and cd133. Total RNA of the cells was extracted using Trizol Reagent (Invitrogen, CA, USA) following manufacturer's directions. Briefly, cells were washed with phosphate buffered saline three times and mixed with 1 ml of Trizol reagent. The mixture was extracted with 200 µl of chloroform. After centrifugation at 10,000×g for 30 minutes, the RNA in the aqueous solution was precipitated by adding an equal volume of isopropanol. The precipitated RNA was collected by centrifugation at 10,000×g for 20 minutes, washed by 70% ethanol, dissolved in 20 µl of RNase-free water. The amount of RNA was quantified by its absorption at 260 nm and stored at -80℃ before use. The housekeeping gene, glyceraldehyde-3-phosphate dehydrogenase (gapdh), was used as an internal control, and the mRNA expression of different molecular markers was analyzed by a semiquantitative RT-PCR assay. Briefly, first-strand cDNAs were synthesized from 5 µg of total RNA using superscript III reverse transcriptase (Invitrogen, CA, USA). PCR amplification was performed with specific primer pairs designed from published human gene sequences (Table 1) using a GeneAmp PCR System 9700 (Applied Biosystems, Foster City, CA).
The effect of the anticancer drugs 5-FU and MTX on the expression of CSCs markers was studied in A549, H460, and H23 NSCLC cell lines using FACS analysis. The fractions of ABCG2(+), IL-6R(+), and CD133(+) cells were significantly increased by treatment with 5-FU or MTX in these NSCLC cell lines.
In vehicle-treated A549 cells, approximately 17% of the cells were ABCG2(+). Following 5-FU and MTX treatment, the ABCG2(+) cell-fraction was significantly increased by 2.3- and 4.6-fold, respectively (Fig. 1). H460 cells also showed a 3.5- and 3.9-fold increase in the number of ABCG2(+) cells in response to 5-FU and MTX, respectively. Also, H23 cells displayed a 10~20% increase in the ABCG2(+) fraction by treatment with 5-FU and MTX compared to control treated cells.
As shown in Fig. 2, the population of IL-6R(+) cells in A549, H460, and H23 were 1.4, 0.04, and 0.74%, respectively. IL-6R(+) fractions were significantly increased by MTX treatment in all 3 cell lines. Alternatively, the IL-6R (+) fraction was not increased by 5-FU in A549 and H23 cells, but H460 cells displayed a large increase in the IL-6R (+) cell population. In the 3 NSCLC cell lines tested, the CD133(+) population varied from 0.17% to 0.82% (Fig. 3). Specifically, in A549 cells, the CD133(+) fraction was slightly increased by 5-FU or MTX treatment, while the CD133(+) fractions were markedly increased by 2- to 7-fold by 5-FU or MTX treatment in H460 and H23.
The expression of ABCG2, IL-6R, and CD133 was confirmed at the mRNA level in the A549, H460, and H23 NSCLC cell lines using semi-quantitative RT-PCR (Figs. 4~6). The expression levels of abcg2 and il-6r were increased in the 3 cell lines following treatment with 5-FU or MTX. As shown in Fig. 6, the expression level of cd133 was increased in A549 cell line following treatment with 5-FU or MTX.
Various studies have revealed that CSCs develop resistance to anticancer drugs [3,11,23], but the mechanisms responsible for this trait have not been well established. In our study, 5-FU and MTX treatment increased ABCG2(+) cell populations to a similar extent in 3 NSCLC cell lines. Gene expression of abcg2 was also increased by 5-FU and MTX treatment. 5-FU has been used to select quiescent or slow-dividing stem/progenitor cells based on the fact that only rapidly dividing cells are sensitive to 5-FU [24-26]. There is growing evidence that CSCs are more resistant to 5-FU than non-CSCs [27,28]. This explains why 5-FU treatment can spare CSCs, while inducing cell death in cancer cells. MTX is a typical substrate of the membranous efflux transporter, ABCG2. Therefore, overexpression of ABCG2 in cancer cells results in an extensive reduction in the amount of MTX absorption, leading to drug resistance [29]. Previously, we have shown that lung CSCs have higher expression of ABCG2 and display greater resistance to MTX than non-CSCs [17,30]. This indicates that treating cancer cells with MTX can allow for CSC survival. Although we have no direct evidence for the increase of ABCG2(+) cell populations due to 5-FU and MTX, it is speculated that these anticancer drugs can induce the expression of the ABCG2 transporter, thus sparing drug-resistant CSCs.
Our results indicate that MTX increased the population of IL-6R(+) cells in A549, H460, and H23 cells, while 5-FU increased the IL-6R(+) population in only H460 cells. Although the responses of IL-6R expression to 5-FU treatment were not the same among the 3 NSCLC cell lines tested, the up-regulation of IL-6R(+) cells by MTX was similar in the 3 NSCLC cell lines. Conze et al. demonstrated that IL-6 release could promote resistance to chemotherapy [21] through the induction of multi-drug resistance 1 (MDR1) gene expression [21]. Also, Levina et al. reported that drug resistant-CSCs, isolated from H460 NSCLC cell line, have significantly elevated levels of IL-6 compared to non-CSCs. These reports indicate that IL-6/IL-6R signaling and drug resistance are closely related in both cancer cells and cancer stem cells. Our results demonstrate that the anticancer drugs 5-FU and MTX markedly increased the CD133(+) cell population in 3 NSCLC cell lines. Consistent with our results, Sozzi et al. demonstrated that CD133(+) cells display stem cell-like features and are resistant to anticancer drugs [3]. In addition, Herr et al. showed that CD133(+) cells had a resistance phenotype in lung cancer patients [16]. Therefore, these findings suggest that the elevation of CSC marker-positive cells by 5-FU or MTX treatment results in CSC resistance in NSCLC cell lines.
In conclusion, 5-FU and MTX considerably alter the expression of drug-resistance related CSC populations in the NSCLC cell lines A549, H460, and H23. Thus, we suggest that antimetabolite cancer drugs, such as 5-FU and MTX, can lead to propagation of CSCs by enhancing the expression of several CSC markers. These findings provide a novel mechanism for the highly drug resistant phenotype of lung CSCs and their ability to survive chemotherapy.
Figures and Tables
 | Fig. 1Analysis of ABCG2 expression after 5-FU or MTX treatment. A549, H460, and H23 non-small cell lung cancer cell lines were treated with 5-FU (25 µg/ml) or MTX (50 µg/ml) for 24 hours and incubated with a PE-anti-ABCG2 antibody. The number of fluorescent-conjugated cells in 104 cells was analyzed by fluorescence activated cell sorter (FACS). |
 | Fig. 2Analysis of IL-6R expression after 5-FU or MTX treatment. A549, H460, and H23 non-small cell lung cancer cell lines were treated by 5-FU (25 µg/ml) or MTX (50 µg/ml) for 24 hours and incubated with a FITC-anti-IL-6R antibody. The number of fluorescent-conjugated cells in 104 cells was analyzed by fluorescence activating cell sorter (FACS). |
 | Fig. 3Analysis of CD133 expression after 5-FU or MTX treatment. A549, H460, and H23 non-small cell lung cancer cell lines were treated with 5-FU (25 µg/ml) or MTX (50 µg/ml) for 24 hours and incubated with a PE-anti-CD133 antibody. The number of fluorescent-conjugated cells in 104 cells was analyzed by fluorescence activating cell sorter (FACS). |
 | Fig. 4Gene expression of abcg2 after 5-FU or MTX treatment. (A) A549, H460, and H23 non-small cell lung cancer cell lines were treated with 5-FU (25 µg/ml) or MTX (50 µg/ml) for 6, 12, and 48 hr. After the incubation period, total RNA was extracted, and mRNA levels were analyzed by RT-PCR. PCR amplification was performed using specific primer pairs designed from published human gene sequences. A housekeeping gene, glyceraldehyde-3-phosphate dehydrogenase (gapdh), was selected as an internal control. (B) The densities of the DNA bands of abcg2 were analyzed by Image J Software (NIH, http://rsb.info.nih.gov/nih_image/index.html). |
 | Fig. 5Gene expression of IL-6R after 5-FU or MTX treatment. (A) A549, H460, and H23 non-small cell lung cancer cell lines were treated with 5-FU (25 µg/ml) or MTX (50 µg/ml) for 6, 12, and 48 hr. After the incubation period, total RNA was extracted, and mRNA levels were analyzed by RT-PCR. PCR amplification was performed using specific primer pairs designed from published human gene sequences. A housekeeping gene, glyceraldehyde-3-phosphate dehydrogenase (gapdh), was selected as an internal control. (B) The densities of the DNA bands of il-6r were analyzed by the Image J Software. |
 | Fig. 6Gene expression of CD133 after 5-FU or MTX treatment. (A) A549, H460, and H23 non-small cell lung cancer cell lines were treated with 5-FU (25 µg/ml) or MTX (50 µg/ml) for 12 hr. After the incubation period, total RNA was extracted, and mRNA levels were analyzed by RT-PCR. PCR amplification was performed using specific primer pairs designed from published human gene sequences. A housekeeping gene, glyceraldehyde-3-phosphate dehydrogenase (gapdh), was selected as an internal control. (B) The densities of the DNA bands of cd133 were analyzed by the Image J Software. |
References
1. Ponti D, Costa A, Zaffaroni N, Pratesi G, Petrangolini G, Coradini D, Pilotti S, Pierotti MA, Daidone MG. Isolation and in vitro propagation of tumorigenic breast cancer cells with stem/progenitor cell properties. Cancer Res. 2005. 65:5506–5511.
2. Pardal R, Clarke MF, Morrison SJ. Applying the principles of stem-cell biology to cancer. Nat Rev Cancer. 2003. 3:895–902.
3. Bertolini G, Roz L, Perego P, Tortoreto M, Fontanella E, Gatti L, Pratesi G, Fabbri A, Andriani F, Tinelli S, Roz E, Caserini R, Lo Vullo S, Camerini T, Mariani L, Delia D, Calabrò E, Pastorino U, Sozzi G. Highly tumorigenic lung cancer CD133(+) cells display stem-like features and are spared by cisplatin treatment. Proc Natl Acad Sci USA. 2009. 106:16281–16286.
4. Yang JP, Liu Y, Zhong W, Yu D, Wen LJ, Jin CS. Chemoresistance of CD133+ cancer stem cells in laryngeal carcinoma. Chin Med J (Engl). 2011. 124:1055–1060.
5. Yanamoto S, Kawasaki G, Yamada S, Yoshitomi I, Kawano T, Yonezawa H, Rokutanda S, Naruse T, Umeda M. Isolation and characterization of cancer stem-like side population cells in human oral cancer cells. Oral Oncol. 2011. 47:855–860.
6. Miraglia S, Godfrey W, Yin AH, Atkins K, Warnke R, Holden JT, Bray RA, Waller EK, Buck DW. A novel five-transmembrane hematopoietic stem cell antigen: isolation, characterization, and molecular cloning. Blood. 1997. 90:5013–5021.
7. Singh SK, Hawkins C, Clarke ID, Squire JA, Bayani J, Hide T, Henkelman RM, Cusimano MD, Dirks PB. Identification of human brain tumour initiating cells. Nature. 2004. 432:396–401.
8. Vander Griend DJ, Karthaus WL, Dalrymple S, Meeker A, DeMarzo AM, Isaacs JT. The role of CD133 in normal human prostate stem cells and malignant cancer-initiating cells. Cancer Res. 2008. 68:9703–9711.
9. Hermann PC, Huber SL, Herrler T, Aicher A, Ellwart JW, Guba M, Bruns CJ, Heeschen C. Distinct populations of cancer stem cells determine tumor growth and metastatic activity in human pancreatic cancer. Cell Stem Cell. 2007. 1:313–323.
10. Eramo A, Lotti F, Sette G, Pilozzi E, Biffoni M, Di Virgilio A, Conticello C, Ruco L, Peschle C, De Maria R. Identification and expansion of the tumorigenic lung cancer stem cell population. Cell Death Differ. 2008. 15:504–514.
11. Levina V, Marrangoni AM, DeMarco R, Gorelik E, Lokshin AE. Drug-selected human lung cancer stem cells: cytokine network, tumorigenic and metastatic properties. PLoS One. 2008. 3:e3077.
12. Stanley K, Stjernswärd J. Lung cancer--a worldwide health problem. Chest. 1989. 96:1 Suppl. 1S–5S.
13. Jiang T, Collins BJ, Jin N, Watkins DN, Brock MV, Matsui W, Nelkin BD, Ball DW. Achaete-scute complex homologue 1 regulates tumor-initiating capacity in human small cell lung cancer. Cancer Res. 2009. 69:845–854.
14. Chen YC, Hsu HS, Chen YW, Tsai TH, How CK, Wang CY, Hung SC, Chang YL, Tsai ML, Lee YY, Ku HH, Chiou SH. Oct-4 expression maintained cancer stem-like properties in lung cancer-derived CD133-positive cells. PLoS One. 2008. 3:e2637.
15. Bertolini G, Roz L, Perego P, Tortoreto M, Fontanella E, Gatti L, Pratesi G, Fabbri A, Andriani F, Tinelli S, Roz E, Caserini R, Lo Vullo S, Camerini T, Mariani L, Delia D, Calabrò E, Pastorino U, Sozzi G. Highly tumorigenic lung cancer CD133+ cells display stem-like features and are spared by cisplatin treatment. Proc Natl Acad Sci USA. 2009. 106:16281–16286.
16. Salnikov AV, Gladkich J, Moldenhauer G, Volm M, Mattern J, Herr I. CD133 is indicative for a resistance phenotype but does not represent a prognostic marker for survival of non-small cell lung cancer patients. Int J Cancer. 2010. 126:950–958.
17. Seo DC, Sung JM, Cho HJ, Yi H, Seo KH, Choi IS, Kim DK, Kim JS, El-Aty AM A, Shin HC. Gene expression profiling of cancer stem cell in human lung adenocarcinoma A549 cells. Mol Cancer. 2007. 6:75.
18. Hodge DR, Hurt EM, Farrar WL. The role of IL-6 and STAT3 in inflammation and cancer. Eur J Cancer. 2005. 41:2502–2512.
19. Tchirkov A, Khalil T, Chautard E, Mokhtari K, Véronèse L, Irthum B, Vago P, Kémény JL, Verrelle P. Interleukin-6 gene amplification and shortened survival in glioblastoma patients. Br J Cancer. 2007. 96:474–476.
20. Gao SP, Mark KG, Leslie K, Pao W, Motoi N, Gerald WL, Travis WD, Bornmann W, Veach D, Clarkson B, Bromberg JF. Mutations in the EGFR kinase domain mediate STAT3 activation via IL-6 production in human lung adenocarcinomas. J Clin Invest. 2007. 117:3846–3856.
21. Conze D, Weiss L, Regen PS, Bhushan A, Weaver D, Johnson P, Rincón M. Autocrine production of interleukin 6 causes multidrug resistance in breast cancer cells. Cancer Res. 2001. 61:8851–8858.
22. Wang H, Lathia JD, Wu Q, Wang J, Li Z, Heddleston JM, Eyler CE, Elderbroom J, Gallagher J, Schuschu J, MacSwords J, Cao Y, McLendon RE, Wang XF, Hjelmeland AB, Rich JN. Targeting interleukin 6 signaling suppresses glioma stem cell survival and tumor growth. Stem Cells. 2009. 27:2393–2404.
23. Liu T, Xu F, Du X, Lai D, Liu T, Zhao Y, Huang Q, Jiang L, Huang W, Cheng W, Liu Z. Establishment and characterization of multi-drug resistant, prostate carcinoma-initiating stem-like cells from human prostate cancer cell lines 22RV1. Mol Cell Biochem. 2010. 340:265–273.
24. Campard D, Vasse M, Rose-John S, Poyer F, Lamacz M, Vannier JP. Multilevel regulation of IL-6R by IL-6-sIL-6R fusion protein according to the primitiveness of peripheral blood-derived CD133+ cells. Stem Cells. 2006. 24:1302–1314.
25. Rice A, Barbot C, Lacombe F, Dubosc-Marchenay N, Marit G, Hau F, Boiron JM, Reiffers J. 5-fluorouracil permits access to a primitive subpopulation of peripheral blood stem cells. Stem Cells. 1993. 11:326–335.
26. Bertolini F, Battaglia M, Soligo D, Corsini C, Curioni C, Lazzari L, Pedrazzoli P, Thalmeier K. "Stem cell candidates" purified by liquid culture in the presence of Steel factor, IL-3, and 5FU are strictly stroma-dependent and have myeloid, lymphoid, and megakaryocytic potential. Exp Hematol. 1997. 25:350–356.
27. Todaro M, Perez Alea M, Scopelliti A, Medema JP, Stassi G. IL-4-mediated drug resistance in colon cancer stem cells. Cell Cycle. 2008. 7:309–313.
28. Takaishi S, Okumura T, Tu S, Wang SS, Shibata W, Vigneshwaran R, Gordon SA, Shimada Y, Wang TC. Identification of gastric cancer stem cells using the cell surface marker CD44. Stem Cells. 2009. 27:1006–1020.
29. Volk EL, Farley KM, Wu Y, Li F, Robey RW, Schneider E. Overexpression of wild-type breast cancer resistance protein mediates methotrexate resistance. Cancer Res. 2002. 62:5035–5040.
30. Sung JM, Cho HJ, Yi H, Lee CH, Kim HS, Kim DK, Abd El-Aty AM, Kim JS, Landowski CP, Hediger MA, Shin HC. Characterization of a stem cell population in lung cancer A549 cells. Biochem Biophys Res Commun. 2008. 371:163–167.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download