Abstract
Purpose
We report the detection of peripheral retinal vascular abnormalities in the fellow eye with normal fundus in children with unilateral Coats' disease.
Methods
The clinical records of patients diagnosed with Coats' disease were retrospectively reviewed. We recorded the subjects' characteristics and obtained fundus photography and fluorescein angiography (FA) images. The main outcome measure was peripheral vascular abnormalities in the contralateral eye with normal fundus in children with unilateral Coats' disease, observed with FA.
Results
Out of 47 patients with Coats' disease, two (4.3%) were diagnosed with clinically bilateral Coats' disease. Of the 45 patients with presumed unilateral Coats' disease, four (8.9%) had bilateral abnormal peripheral vasculature in FA. The mean age of these four patients was 6.4 ± 5.4 years (range, 1 to 14 years), and three patients were male (75%). All four had peripheral retinal nonperfusion, and two (50%) received laser photocoagulation due to peripheral leakage with telangiectatic vessels.
Coats' disease is an idiopathic disease characterized by telangiectatic vessels in the retinal temporal periphery with retinal exudation [1]. This disease usually occurs unilaterally in young males, and bilateral cases are rarely reported [1]. Previous studies have reported that 0% to 10% of patients with Coats' disease had bilateral disease [1234567].
However, the diagnosis of unilateral disease is traditionally based predominantly on indirect ophthalmoscopy and fundus photography. A wide-angle angiography system, the RetCam (Clarity Medical Systems, Pleasenton, CA, USA), has become available for examination under anesthesia (EUA). Using this system, peripheral retinal abnormalities in the fellow eye of patients diagnosed with unilateral disease were reported in a few articles [8910].
This suggests that some cases of asymmetric bilateral Coats' disease can remain undetected on fundus examination or photography [1011]. As Coats' disease is mostly progressive during childhood, early detection of abnormal vasculature is important [12]. Here, we report a case series of pediatric patients with unilateral Coats' disease who had these retinal abnormalities and received treatment on the contralateral eye with normal fundus.
A retrospective review of medical records was performed on patients with Coats' disease who underwent EUA at the Seoul National University Children's Hospital between April 2007 and August 2016. The diagnosis of Coats' disease was based on the presence of telangiectatic retinal vessels associated with subretinal exudation. Patients with systemic disorders or history of premature birth (37 weeks or less) were excluded. The institutional review board of Seoul National University Hospital reviewed and approved this study (1712-085-907).
Patients with Coats' disease who had undergone retinal imaging and fluorescein angiography (FA) of both eyes during or before EUA were included. During EUA, FA in conjunction with scleral indentation to image the ora serrata region using the RetCam was performed. The main outcome measure was fluorescein angiographic peripheral vascular abnormalities on the contralateral eye with normal fundus in children with unilateral Coats' disease.
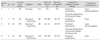
The following preoperative information was collected through a review of medical records from the patients with presumed unilateral Coats' disease: age, sex, laterality of disease, family history, and preoperative ocular abnormalities. Patients with Coats' disease were classified into different stages as described in 2001 by Shields et al. (Table 1) [13]. Fundus photography and FA were reviewed to judge the presence of microaneurysm, telangiectasia, and peripheral retinal nonperfusion in both eyes. Distance from the ora serrata to the vascular termini temporally and nasally was recorded in disc diameter, which is the measurement used in clinical practice and in previous descriptions of the anterior retina [11141516]. If vascular termini were visible but the ora serrata was not, the width of peripheral nonperfusion was measured from the vessel termini to the edge of the image, thus underestimating the actual width [9]. Peripheral nonperfusion was defined as 2 or more disc diameters of nonperfusion [11]. Treatment of retinal abnormalities in both eyes was also assessed.
In total, 47 patients were diagnosed with Coats' disease and had undergone retinal imaging and FA in both eyes. The mean age of the patients was 6.8 ± 4.7 years (range, 1 to 18 years), and 40 patients (85.1%) were male. Six patients (12.8%) had bilateral abnormal vasculature. Of these 47 patients, two (4.3%) were diagnosed with clinically bilateral Coats' disease. Fundoscopic examination showed bilateral foveal exudation with vascular telangiectasia, although retinal detachment presented asymmetrically.
Of the 45 patients with presumed unilateral Coats' disease, four (8.9%) had bilateral peripheral vascular abnormalities in FA. The demographics and clinical characteristics of these four included patients are summarized in Table 2, and they had no family history. The mean age of these patients was 6.4 ± 5.4 years (range, 1 to 14 years), and three patients (75.0%) were male. All four patients showed temporal peripheral retinal nonperfusion and changes in the capillary bed anatomy, such as coarsening or closure of capillaries (Fig. 1A–1D, 2A–2D, 3A–3F). Two (50.0%) of them received laser photocoagulation due to peripheral leakage with telangiectatic vessels (Fig. 1A–1D, 2A–2D). As the other two patients had no leaking microaneurysms, they were managed with observation.
We report a series of four patients initially diagnosed with unilateral Coats' disease who later showed bilateral abnormal retinal vasculature on FA. Shields et al. [1] have reported that 5% of patients with Coats' disease had bilateral disease, and most reported cases of bilateral Coats' disease represent other conditions and do not meet the criteria for diagnosis. They also reported that bilateral Coats' disease showed asymmetry of severity. In our study, two (4.3%) out of a total of 47 patients had clinically bilateral Coats' disease, and both patients showed asymmetric staging. This result is comparable to other reports of well-documented Coats' disease [1345].
As FA has become available during EUA, subtle peripheral retinal abnormalities have been detected in the fellow eyes of patients with unilateral Coats' disease [910]. Our study also demonstrated that four (8.9%) of 45 patients with normal fundus in children with unilateral Coats' disease had bilateral abnormal vascular peripheral vasculature in FA. This supports the idea that there may be bilateral abnormalities of Coats' disease that are undetected by traditional methods, and it may more often be a bilateral disease with asymmetry [910]. Blair et al. [9] reported that 15 of 24 patients (62.5 %) had peripheral nonperfusion in contralateral eyes in presumed unilateral Coats' disease, and their mean age was 6.5 ± 4.2 years (range, 1 to 14 years). Suzani and Moore [8] reported that only one (4%) of 25 patients had minor areas of nonperfusion in the contralateral eye in patients with early (stage 2) unilateral Coats' disease. These variable proportions may be due to the quality of the angiograms or different stages of the affected eye [8]. In our study, imaging of the contralateral eye was not routinely performed at an early phase of the angiogram, and patients showed different stages (stage 2a to 3b) in the affected eyes. Although the effects of race on the predilection for and clinical differences in Coats' disease are not yet known, there may be variability due to race. Coats' disease in Asian patients has been reported in a few articles [11217].
These subtle bilateral findings in presumed unilateral cases support an underlying genetic cause. Furthermore, familial exudative vitreoretinopathy and Coats' disease share similar fundus features, including peripheral avascularization of the retina and retinal exudation [1011]. Arguments that familial exudative vitreoretinopathy and Coats' disease exist on a continuous spectrum of retinal vascular disorders have been supported by their phenotypic similarity [91018].
Our study is limited by its retrospective design, small sample size, and suboptimal quality of angiogram. However, to the best of our knowledge, this is the first report to treat peripheral retinal abnormalities on contralateral eyes with normal fundus in children with unilateral Coats' disease. As Coats' disease is mainly a progressive condition, early detection of vascular abnormalities is important to preserve visual acuity [12]. In stage 1 disease, there is a high probability that the eye can be salvaged, the visual prognosis is favorable, and the disease can be managed by either periodic observation or laser photocoagulation [1213]. We applied laser treatment around the telangiectatic vessels to cauterize the retinal vasculature in two patients through early detection by FA. Two patients who received treatment in fellow eyes showed no progression during a follow-up period of 6 months.
In conclusion, patients with Coats' disease should undergo careful examination of the fellow eye with FA in order to detect vascular abnormalities that might not be visible clinically. As Coats' disease is a progressive ocular condition, early detection of vascular abnormalities and proper treatment are necessary.
Figures and Tables
Fig. 1
Color fundus photography and fluorescein angiography were performed using the RetCam during an examination under anesthesia (patient 1). Fundus photography showing (A) no definite abnormal vasculature in the right eye and (B) widespread yellowish exudates with partial cystic change and vascular telangiectasia in the left eye. (C) Fluorescein angiogram (1:58) demonstrating a peripheral avascular retina bordered posteriorly by leaking telangiectasias in the right eye. (D) Laser photocoagulation was applied to the peripheral avascular retina in the right eye.
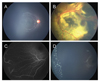
Fig. 2
Color fundus photography and fluorescein angiography of patient 3. Fundus photography showing (A) yellowish exudates with vascular telangiectasia in the right eye and (B) no definite abnormal vasculature in the left eye. (C) Fluorescein angiogram (1:07) demonstrating peripheral avascular retina, shunt vessels, and leaking telangiectasias in the left eye. (D) Laser photocoagulation with a large spot diode laser was applied around the leaking telangiectasias in the left eye.

Fig. 3
Color fundus photography and fluorescein angiography of patients 2 (A–C) and 4 (D–F). (A,D) Fundus photography showing no definite abnormal vasculature in the contralateral eye of either patient. Early phase fluorescein angiogram of patients 2 (B, 1:19) and 4 (E, 0:52), demonstrating peripheral nonperfusion, capillary bed closure, and shunt formation (arrow). However, no leakage was confirmed in either patient. (C,F) Fundus photography showing yellowish exudates and vascular telangiectasia in the affected eyes of both patients. (C) Laser photocoagulation was applied in the left eye in patient 2.

References
1. Shields JA, Shields CL, Honavar SG, Demirci H. Clinical variations and complications of Coats disease in 150 cases: the 2000 Sanford Gifford Memorial Lecture. Am J Ophthalmol. 2001; 131:561–571.

2. Woods AC, Duke JR. Coats's disease. I. Review of the literature, diagnostic criteria, clinical findings, and plasma lipid studies. Br J Ophthalmol. 1963; 47:385–412.

4. Spitznas M, Joussen F, Wessing A, Meyer-Schwickerath G. Coat's disease: an epidemiologic and fluorescein angiographic study. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1975; 195:241–250.
5. Tarkkanen A, Laatikainen L. Coat's disease: clinical, angiographic, histopathological findings and clinical management. Br J Ophthalmol. 1983; 67:766–776.

6. Shienbaum G, Tasman WS. Coats disease: a lifetime disease. Retina. 2006; 26:422–424.
7. Rishi P, Rishi E, Uparkar M, et al. Coats' disease: an Indian perspective. Indian J Ophthalmol. 2010; 58:119–124.

8. Suzani M, Moore AT. Intraoperative fluorescein angiography-guided treatment in children with early Coats' disease. Ophthalmology. 2015; 122:1195–1202.

9. Blair MP, Ulrich JN, Elizabeth Hartnett M, Shapiro MJ. Peripheral retinal nonperfusion in fellow eyes in coats disease. Retina. 2013; 33:1694–1699.

10. Shane TS, Berrocal AM, Hess DJ. Bilateral fluorescein angiographic findings in unilateral Coats' disease. Ophthalmic Surg Lasers Imaging. 2011; 42:e15–e17.

11. Blair MP, Shapiro MJ, Hartnett ME. Fluorescein angiography to estimate normal peripheral retinal nonperfusion in children. J AAPOS. 2012; 16:234–237.

12. Ghorbanian S, Jaulim A, Chatziralli IP. Diagnosis and treatment of coats' disease: a review of the literature. Ophthalmologica. 2012; 227:175–182.

13. Shields JA, Shields CL, Honavar SG, et al. Classification and management of Coats disease: the 2000 Proctor Lecture. Am J Ophthalmol. 2001; 131:572–583.

14. Rutnin U, Schepens CL. Fundus appearance in normal eyes. II. The standard peripheral fundus and developmental variations. Am J Ophthalmol. 1967; 64:840–852.
15. Rutnin U, Schepens CL. Fundus appearance in normal eyes. IV. Retinal breaks and other findings. Am J Ophthalmol. 1967; 64:1063–1078.
16. Rutnin U, Schepens CL. Fundus appearance in normal eyes. 3. Peripheral degenerations. Am J Ophthalmol. 1967; 64:1040–1062.
17. Lai CH, Kuo HK, Wu PC, et al. Manifestation of Coats' disease by age in Taiwan. Clin Exp Ophthalmol. 2007; 35:361–365.

18. Sims KB. NDP-related retinopathies. In : Pagon RA, Adam MP, Ardinger HH, editors. GeneReviews(R). Seattle: University of Washington;2014.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download