Abstract
Purpose
To evaluate the effects of the surgical assistant's level of resident training on operation time and surgical outcome in the surgical treatment of intermittent exotropia.
Methods
This study included 456 patients with intermittent exotropia who underwent lateral rectus recession and medial rectus resection and were followed up for 24 months after surgery. The patients were divided into two groups according to the surgical assistant's level of resident training: group F (surgery assisted by a first-year resident [n = 198]) and group S (surgery assisted by a second-, third-, or fourth-year resident [n = 258]). The operation time and surgical outcomes (postoperative exodeviation and the number of patients who underwent a second operation) were compared between the two groups.
Results
The average operation times in groups F and S were 36.54 ± 7.4 and 37.34 ± 9.94 minutes, respectively (p = 0.33). Immediate postoperative exodeviation was higher in group F (0.79 ± 3.82 prism diopters) than in group S (0.38 ± 3.75 prism diopters). However, repeated-measures analysis of variance revealed no significant difference in exodeviation between the two groups during the 24-month follow-up period (p = 0.45). A second operation was performed in 29.3% (58 / 198) of the patients in group F, and in 32.2% (83 / 258) of those in group S (p = 0.51).
Conclusions
No significant difference in operation time was observed when we compared the effects of the level of resident training in the surgical treatment of intermittent exotropia. Although the immediate postoperative exodeviation was higher in patients who had undergone surgery assisted by a first-year resident, the surgical outcome during the 24-month follow-up was not significantly different.
The main purpose of strabismus surgery is to align the eyes to their primary position. Previous studies have identified several factors related to surgical outcomes in intermittent exotropia: preoperative angle deviation, near and distance angle deviation difference, and age at surgery [123]. In addition, the main surgeon must perform a safe and exact procedure to ensure good surgical outcomes; the assistant's ability to facilitate the procedure and expose the proper surgical field is also important. Indeed, the assistant's level of training can influence operation times and complication rates in other fields of surgery, such as laparoscopic cholecystectomy or colon surgery [45]. However, there have not been any studies investigating the association between the level of assistant training and surgical outcomes in the surgical treatment of intermittent exotropia. Therefore, the purpose of this study was to investigate the effects of the surgical assistant's level of resident training on operation time and surgical outcomes in the treatment of intermittent exotropia.
This study was approved by the institutional review board of Yeungnam University Hospital (YUH-14-0395-O40). Informed consent was waived by the board. A retrospective medical chart review was performed in patients with intermittent exotropia who had undergone lateral rectus recession and medial rectus resection (R&R) at Yeungnam University Hospital between August 1991 and October 2011 and were followed up for 24 months after surgery. Only patients with the basic type of intermittent exotropia with a distance deviation within 10 prism diopters (PD) of the near deviation were included in this study. Patients with pseudo-divergence excess, as determined using the patch test, were excluded, as were those with constant exotropia, oblique muscle dysfunction, dissociated vertical deviation, an A-V pattern, nystagmus, previous intraocular surgery, any neurological impairments, or severe unilateral amblyopia. Patients missing any regular follow-up over the 24 months after surgery were also excluded. There were three residents in each grade at our clinic. All surgeries were assisted by a randomly participating resident from the first to fourth year. The included patients were divided into two groups according to the level of resident training of the surgical assistant: group F (patients with intermittent exotropia who had undergone surgery assisted by a first-year resident) and group S (patients with intermittent exotropia who had undergone surgery assisted by a second-, third-, or fourth-year resident).
At the initial visit, all patients underwent an examination for ophthalmologic evaluation that included best corrected visual acuity measurement, slit-lamp biomicroscopy, a dilated fundus examination, refractive error measurement, and a stereoacuity test. In cooperative children, the angle of deviation was measured both before and after surgery using the alternate prism cover test at 6 m and 33 cm fixation. Best-corrected visual acuity was measured when possible. If the patients were too young for optotype testing at the initial visit, the visual acuity was evaluated based on the fixation preference. To measure the largest angle of deviation, an additional near measurement was obtained after 1 hour of monocular occlusion of the non-dominant eye. The post-occlusion near measurement was then obtained before binocular fusional ability was restored, with an additional +3.00-diopter (D) sphere over each eye. Stereoacuity was confirmed using the Lang 1 test (Lang-Stereotest AG, Küsnacht, Switzerland) and the Stereo Fly Stereotest (Stereo Optical, Chicago, IL, USA) when the patient was able to cooperate and complete the test. All surgeries were performed by a single surgeon (KMM) using a fornix incision with the patient under general anesthesia. The surgical dosage of R&R in our clinic is demonstrated in Table 1. The operation time was defined as the duration from beginning to end of the surgical procedure as assessed by the anesthetic chart. The angle of deviation during the first follow-up visit, which took place within one week of surgery, was defined as the immediate postoperative deviation. The patients were followed up at 1, 3, 6, and 12 months after surgery, and every 6 months thereafter.
Independent t-tests were performed for continuous variables. To compare non-continuous variables, the chi-square method was used. The operation time and surgical outcomes (exodeviation at each follow-up visit for 24 months, and number of patients who underwent a second operation until the last follow-up) were compared between the two groups. To enhance statistical analysis, patients who missed any regular follow-up over the 24 postoperative months were excluded from the study. Repeated measures analysis of variance was performed to compare the postoperative angle of deviation. All data were analyzed using IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA). All p-values <0.05 were considered statistically significant.
A total of 456 patients with intermittent exotropia met the inclusion criteria for this study and were classified into two groups according to the level of assistant training. Of these, 198 patients were included in group F and 258 patients were included in group S. Table 2 shows the demographic and clinical characteristics of the two groups. There were no significant differences in gender distribution, age at surgery, spherical equivalent refractive error, anisometropia, preoperative angle of deviation, laterality of the operated eye, and stereotest results between the two groups.
Group F (36.54 ± 7.49 minutes) had a shorter mean operation time than group S (37.34 ± 9.95 minutes); however, this difference failed to reach statistical significance (p = 0.33). The immediate postoperative angle of deviation was larger in group F (0.79 ± 3.82 PD) than in group S (0.38 ± 3.75 PD) (Table 3); however, repeated-measures analysis of variance revealed that there was no significant difference in exodeviation between the two groups during the 24 months of follow-up (p = 0.45) (Fig. 1). A second operation was performed in 29.3% (58 / 198) of the patients in group F, and in 32.2% (83 / 258) of the patients in group S until the last follow-up. This difference was not significantly different between the two groups (p = 0.51) (Table 3).
Operation time and surgical outcomes are closely related in most fields of surgery. Specifically, longer operation times usually lead to more postoperative complications [67]. Many factors contribute to operation time such as the skill level of the main surgeon, the patient's status at the time of surgery, and the function of the surgical assistant. In other fields of surgery, surgeries assisted by lower level residents are associated with significant increases in surgical times, complications, and costs [4589]. However, there have not been any studies investigating the relationship between the level of training of surgical assistants and outcomes in surgery to correct strabismus.
In the present study, we focused on how the level of training of surgical assistants affected the operation time and outcomes after surgery for intermittent exotropia, the most common type of strabismus among Asian patients. The R&R procedure is one of the most common surgical methods used to correct exotropia. In contrast with other surgical procedures, such as unilateral or bilateral lateral rectus recession, an assistant's skill can affect the surgery and surgical outcomes in the R&R procedure because this technique involves providing a complex surgical field and exposure of the medial rectus muscle [10]. In South Korea, residents usually participate in surgery as surgical assistants. Therefore, in the present study, the level of training of surgical assistants was stratified according to the level of resident training. Winter et al. [11] reported that the operation time in strabismus surgery was longer when lower level residents acted as surgical assistants, and that this increased operation time led to additional surgical costs. They suggested that experience and interest in the surgical procedure affected the operation time. However, although group F had shorter operation times than group S in the current study, the difference was less than a minute. Prior to the study, we speculated that surgery assisted by lower level residents would have a longer operation time; however, our results ran contrary to our speculation, suggesting that the level of training of surgical assistants does not drastically affect the operation time in surgical treatment of intermittent exotropia. Moreover, surgical outcomes did not show a significant difference between the two groups. In other fields of surgery, previous studies have reported that an assistant's level of training affects both the surgery and surgical outcomes [4512], although some studies have claimed that this relationship is minimal [1314]. It may be that this association is due to the learning curve for surgical procedures and the use of surgical instruments. For example, in laparoscopic surgery, even the main surgeon has a steep learning curve and must become accustomed to laparoscopic instruments and the view of internal organs through these instruments. In the same way, assistants need time to become familiar with anatomy as viewed through the laparoscope, and to become comfortable with the use of laparoscopic surgical instruments. In particular, Hwang et al. [15] reported that novice assistants must take part in at least 38 laparoscopic operations before they can function adequately. For strabismus surgery, the exact number of cases needed for assistants to become accustomed to the procedure has not been determined. However, differences in the time taken for an assistant to become comfortable with the operation or use of instruments may affect operation times and outcomes. In the present study, the immediate postoperative angle of deviation was larger in group F (0.79 ± 3.82 PD) than in group S (0.38 ± 3.75 PD). This difference in the immediate postoperative deviation between the two groups may be due to the amount of medial R&R as affected by the training level of the assistant. During the medial R&R procedure, the assistant exposes the medial rectus and surgical field using two muscle hooks. A study by Jeon et al. [10] showed that the amount of medial R&R can be changed with the muscle hooks, so there may be differences in the ocular muscle resection with different assistants during the same surgical procedure with the same surgeon. However, in their follow-up study, the same investigators concluded that these errors were not likely to influence surgical outcomes [16]. Our study agrees with the results above, although the immediate postoperative angle of deviation was larger in patients who had undergone surgery assisted by a f irst-year resident (group F). Throughout the 24-month follow-up period, there was no significant difference in the angle of deviation between the two groups, suggesting that the surgical outcome is not affected by the level of assistant training in the surgical treatment of intermittent exotropia.
This study had some limitations. First, we were not able to analyze interpersonal differences in the level of surgical assistants among residents because of the retrospective nature of the study. Since there were only three residents in each grade, interpersonal differences could have influenced the surgical outcome. To clarify the effect of this factor, a prospective study stratified by each individual resident may be considered in the future. Second, this study only included patients with intermittent exotropia who had undergone the R&R procedure. Therefore, the results do not reflect the association between surgical outcomes and level of assistant training in other surgical procedures such as unilateral or bilateral rectus recession. The influence of assistant training level in surgeries for other types of strabismus including the restrictive type and re-operation is also questionable. Third, differences in assistant skill by monthly period and their effect on surgical outcome were not analyzed. There may be differences in assistant skill between the early and late learning phase of first year residents. However, we were unable to analyze the association between the monthly learning effect and surgical outcome in group F because of the small size of the monthly group. These questions will be further examined in a future study.
In conclusion, the level of resident training of assistants did not affect operation time in the surgical treatment of intermittent exotropia. Although the immediate postoperative exodeviation was higher in patients who had undergone surgery assisted by a first-year resident, the surgical outcome throughout the 24-month postoperative follow-up was not significantly different from outcomes in patients who had undergone surgery assisted by a second-, third-, or fourth-year resident.
Figures and Tables
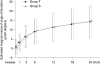 | Fig. 1The postoperative angle of deviation over the 24-month follow-up for groups F and S. Group F: patients with intermittent exotropia who underwent surgery assisted by a first-year resident. Group S: patients with intermittent exotropia who underwent surgery assisted by a second-, third- or fourth-year resident. Repeated measures analysis of variance revealed no significant difference in exodeviation over 24 months postoperatively between the two groups (p = 0.45). The plus numbers of prism diopters represent exodeviation and the minus numbers of prism diopters represent esodeviation. |
Table 1
Surgical dosage of LR recession and MR resection for patients with intermittent exotropia at Yeungnam University Hospital

Table 2
Demographics and clinical characteristics of patients in groups F and S

Group F: patients with intermittent exotropia who underwent surgery assisted by a first-year resident. Group S: patients with intermittent exotropia who underwent surgery assisted by a second-, third- or fourth-year resident.
SE = spherical equivalent; D = diopter; PD = prism diopter.
*Chi-square test; †Independent samples t-test.
Notes
References
1. Gezer A, Sezen F, Nasri N, Gozum N. Factors influencing the outcome of strabismus surgery in patients with exotropia. J AAPOS. 2004; 8:56–60.

2. Lim SH, Hwang BS, Kim MM. Prognostic factors for recurrence after bilateral rectus recession procedure in patients with intermittent exotropia. Eye (Lond). 2012; 26:846–852.

3. Wright KW, Strube YN, editors. Pediatric ophthalmology and strabismus. 3rd ed. New York: Oxford University Press;2012. p. 306–316.
4. Kim YW, Min BS, Kim NK, et al. The impact of incorporating of a novice assistant into a laparoscopic team on operative outcomes in laparoscopic sigmoidectomy: a prospective study. Surg Laparosc Endosc Percutan Tech. 2010; 20:36–41.

5. Scheer A, Martel G, Moloo H, et al. Laparoscopic colon surgery: does operative time matter? Dis Colon Rectum. 2009; 52:1746–1752.

6. Ando M, Takahashi Y, Kikuchi T. Short operation time: an important element to reduce operative invasiveness in pediatric cardiac surgery. Ann Thorac Surg. 2005; 80:631–635.

7. Mannen K, Tsunada S, Hara M, et al. Risk factors for complications of endoscopic submucosal dissection in gastric tumors: analysis of 478 lesions. J Gastroenterol. 2010; 45:30–36.

8. Hosler MR, Scott IU, Kunselman AR, et al. Impact of resident participation in cataract surgery on operative time and cost. Ophthalmology. 2012; 119:95–98.

9. Pollei TR, Barrs DM, Hinni ML, et al. Operative time and cost of resident surgical experience: effect of instituting an otolaryngology residency program. Otolaryngol Head Neck Surg. 2013; 148:912–918.

10. Jeon GS, Choi MY, Choi DG. The change of rectus muscle length caused by traction with muscle hooks in strabismus surgery: the f irst report. J Korean Ophthalmol Soc. 2010; 51:401–405.
11. Winter TW, Olson RJ, Larson SA, et al. Resident and fellow participation in strabismus surgery: effect of level of training and number of assistants on operative time and cost. Ophthalmology. 2014; 121:797–801.
12. Hsu GP, Morton JM, Jin L, et al. Laparoscopic Roux-en-Y gastric bypass: differences in outcome between attendings and assistants of different training backgrounds. Obes Surg. 2005; 15:1104–1110.

13. Bakaeen FG, Dhaliwal AS, Chu D, et al. Does the level of experience of residents affect outcomes of coronary artery bypass surgery? Ann Thorac Surg. 2009; 87:1127–1133.

14. Goodwin AT, Birdi I, Ramesh TP, et al. Effect of surgical training on outcome and hospital costs in coronary surgery. Heart. 2001; 85:454–457.

15. Hwang MR, Seo GJ, Yoo SB, et al. Learning curve of assistants in laparoscopic colorectal surgery: overcoming mirror imaging. Surg Endosc. 2010; 24:2575–2580.

16. Jeon GS, Kim DW, Choi MY, Choi DG. The change of rectus muscle length caused by traction with muscle hooks in strabismus surgery: the second report. J Korean Ophthalmol Soc. 2012; 53:674–680.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download