Abstract
Purpose
To evaluate the clinical outcomes of cataract surgery using novel diffractive trifocal intraocular lenses (IOLs) in Koreans.
Methods
This was a retrospective, consecutive, interventional study of cataract surgery using POD FineVision IOL implantation. Complete ophthalmologic examinations were performed preoperatively and postoperatively. Defocus curves were assessed over a range of +1.5 to −4.0 diopters in 0.5-diopter steps at one month postoperatively. Uncorrected distant visual acuity, uncorrected intermediate visual acuity, uncorrected near visual acuity, corrected distant visual acuity, distant-corrected intermediate visual acuity, and distant-corrected near visual acuity were assessed one month postoperatively, and manifest refraction was performed during every visit.
Results
The study analyzed 31 eyes in 20 patients. There were statistically significant improvements in uncorrected distance visual acuity, uncorrected intermediate visual acuity, uncorrected near visual acuity, corrected distance visual acuity, distance-corrected intermediate visual acuity, and distance-corrected near visual acuity (p < 0.001). The final postoperative refractive outcomes showed statistically significant myopic shifts compared to the target refraction based on SRK/T, SRK-II, Haigis, and Hoffer Q formulas (p < 0.001).
As a result of improvements in surgical instruments and techniques, the concept of cataract surgery has changed from simple extraction of the cataract to refractive surgery that can provide emmetropia. Recently, the objective of cataract surgery has shifted from simply gaining precise refractive outcomes to also removing the need for corrective lenses. Multifocal intraocular lenses (IOLs) are widely used for this purpose; with the increase in their popularity, various multifocal IOLs are being manufactured by different companies, providing broad options in IOLs [12].
Classic multifocal IOLs are bifocal and thus provide two working distances (distant and near). Many studies have confirmed significant improvements in uncorrected near visual acuity (UNVA) while maintaining acceptable uncorrected distance visual acuity (UDVA) [3]. However, intermediate working distance, which is important for computer work or simple household chores, is not covered by classic bifocal IOLs, making glasses necessary for people who work in these fields [45].
Trifocal IOLs have been recently introduced and provide better visual acuity at intermediate distances without impairing far and near vision compared to bifocal IOLs [67]. Currently, there are several commercially available diffractive trifocal IOLs, including the FineVision Micro F (PhysIOL, Liege, Belgium) and the AT LISA tri 839 MP (Carl Zeiss Meditec, Jena, Germany); many studies have reported satisfactory clinical outcomes with these IOLs [891011121314].
The original FineVision Micro F, the first trifocal IOL to reach the market, was later adapted to create a new double C-loop haptic design to guarantee the IOL's rotational stability. This new IOL model was named the POD FineVision, and it has demonstrated comparable visual outcomes and better rotational stability than the previous iteration [15].
FineVision trifocal IOLs are widely used; there is a large body of literature that covers their clinical outcomes outside Asia. However, they have only recently became available in the Korean market; therefore, there are no clinical reports of the outcomes of FineVision trifocal IOLs in a Korean population. According to the manufacturers, there have been several cases of myopic shift after implantation of POD FineVision IOLs in an Asian population, which we believe merits the study deeper. The main purpose of this investigation was to evaluate the clinical outcomes of POD FineVision IOLs in a Korean population and to compare them with previously reported outcomes in Western studies.
This was a retrospective consecutive interventional case series study performed at two hospitals (Samsung Medical Center and Asan Medical Center) in Seoul, Korea. All patients in the study underwent uneventful phacoemulsification surgery with implantation of the FineVision POD F or FineVision POD FT (PhysIOL). The study was performed in accordance with the principles of the Declaration of Helsinki and was approved by the institutional review board of Samsung Medical Center (2016-05-071-002) and informed consent was waived by the board.
Inclusion criteria included the presence of a senile cataract with potential visual acuity greater than 20 / 30 based on the potential acuity meter. Exclusion criteria were a history of previous ocular trauma or surgery and other ocular diseases that might interfere with the outcomes of cataract surgery.
The POD FineVision IOL is a single-piece aspheric diffractive trifocal lens composed of 26% hydrophilic acrylic material with blue and ultraviolet blocking properties. The overall diameter is 11.40 mm, with an optic diameter of 6.00 mm. These IOLs are available in powers from +6.0 to +35.0 diopters (D) in 0.5-D increments. The optic is apodized, and additional powers at the IOL plane are +3.50 D for near vision and +1.75 D for intermediate vision. POD FineVision IOLs without a toric component are manufactured under the FineVision POD F name, while toric versions of POD FineVision IOLs are called FineVision POD FT.
Preoperatively, all patients underwent full ophthalmologic examinations, including UDVA, uncorrected intermediate visual acuity (UIVA) at 80 cm, UNVA at 40 cm, corrected distance visual acuity (CDVA), distance-corrected intermediate visual acuity (DCIVA), and distance-corrected near visual acuity (DCNVA) under photopic conditions (85 candelas/m2), as well as slit-lamp microscopy, intraocular pressure, and fundus examinations.
Anterior chamber depth, axial length, and keratometric values were all measured using IOL Master (Carl Zeiss Meditec, Dublin, CA, USA). Because there have been previous cases in which the POD FineVision IOL caused a myopic shift in Asian eyes, the refractive goals were set at hyperopia (approximately 0.0 to +0.3 D). The SRK/T, SRK-II, Haigis, and Hoffer Q formulas were all considered on the basis of individual characteristics of ocular biometry in the selection of IOL power.
All surgeries were carried out by one of the two experienced surgeons who took part in this study (TYC and MJK). Standard sutureless phacoemulsification with a 3.0-mm clear corneal incision was performed under topical anesthesia. IOL design selection and the incision axis were carefully determined based on preoperative corneal astigmatism, which was measured by Scheimpflug topography (Oculus, Wetzlar, Germany). Non-toric versions of POD FineVision IOLs (FineVision POD F) are used in patients with corneal astigmatism less than 1.0 D. For these patients, steep axis corneal incisions were performed in eyes with corneal astigmatism equal to or greater than 0.5 D, and temporal corneal incisions were made in eyes with corneal astigmatism less than 0.5 D. Toric versions of POD FineVision IOLs (FineVision POD FT) are used in patients with corneal astigmatism equal to or greater than 1.0 D. Temporal corneal incisions were made in these patients. IOLs were implanted in the bag with a single-use injector and cartridge (Microset, PhysIOL). Topical gatifloxacin 0.3%, fluorometholone 0.1%, and bromofenac 0.1% were administered postoperatively.
The patients were routinely evaluated one day, one week, one month, and three months postoperatively and also at every subsequent visit. During these routine ophthalmologic examinations, manifested refraction and uncorrected and corrected distance visual acuities were recorded. Participants underwent thorough ophthalmologic examinations at the one-month postoperative visit. Uncorrected and corrected visual acuities for distance, intermediate, and near vision were measured, and the defocus curves were evaluated under photopic conditions using lenses ranging from +2.0 to −4.0 D in 0.5-D steps. The refractive prediction error, which is defined as the difference in diopters between the actual and intended refractive outcome in a particular patient, was assessed in patients with follow-up periods longer than three months. The manifested refraction results of the last visit were used to analyze the refractive predictability.
This study included 31 eyes in 20 patients (9 men [45.0%] and 11 women [55.0%]) with an average age of 60.5 ± 9.6 years (range, 39 to 80 years). The mean implanted IOL power was 19.7 ± 3.5 D (range, 10.0 to 25.0 D). The potential visual acuity as indicated by a potential acuity meter was 0.04 ± 0.06 in the logarithm of the minimum angle of resolution (logMAR) scale (Table 1). All patients had uneventful cataract surgery with a good centration of IOL and no other pupil distortion or iris trauma.
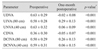
Table 2 shows the preoperative and one-month postoperative visual acuities. The one-month postoperative monocular UDVA, UIVA, UNVA, CDVA, DCIVA, and DCNVA values were −0.02 ± 0.08 (range, −0.17 to 0.10), 0.29 ± 0.13 (range, 0.20 to 0.49), 0.06 ± 0.09 (range, −0.10 to 0.20), −0.05 ± 0.07 (range, −0.18 to 0.00), 0.26 ± 0.13 (range, 0.10 to 0.40), and 0.06 ± 0.15 (range, −0.10 to 0.30) logMAR, respectively. All of the postoperative visual acuities showed statistically significant improvements (Table 2).
Defocus curves illustrate the mean visual acuities and standard deviations for different values of the defocus in the logMAR scale (Fig. 1). Compared to the preoperative defocus curve, the postoperative defocus curve demonstrated general improvement in visual acuities, with a new second peak at a −2.5 D defocus power (equivalent to near viewing at 40 cm). The curve also shows maintenance of visual acuities better than 0.2 logMAR from the defocus power of +1.0 to −3.0 D, indicating that cataract surgeries with FineVision trifocal IOLs provided improvements in near and intermediate vision.
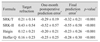
Table 3 displays the refractive results over time. The final postoperative mean monocular refractive correction was 0.09 ± 0.20 D (range, −0.25 to 0.50 D) for the sphere, −0.41 ± 0.27 D (range, 0.00 to −1.00 D) for the cylinder and −0.11 ± 0.22 D (range, −0.50 to 0.25 D) for the spherical equivalent. There were significant reductions in the refractive cylinder (p = 0.002).
Table 4 shows the final postoperative prediction error, which is the difference between the postoperative spherical equivalent measured by manifest refraction and the target refraction of surgery based on SRK/T, SRK-II, Haigis, and Hoffer Q formulas provided by the IOL master. The final postoperative refraction showed a statistically significant myopic shift with all IOL power calculating formulas.
To the best of our knowledge, this is the first study to report clinical outcomes of FineVision trifocal IOL in an Asian population. Compared to previously reported outcomes of FineVision trifocal IOLs, our study showed comparable visual acuities and defocus curves.
The one-month postoperative monocular UDVA, UIVA, UNVA, CDVA, DCIVA, and DCNVA values were −0.02 ± 0.08, 0.29 ± 0.13, 0.06 ± 0.09, −0.05 ± 0.07, 0.26 ± 0.13, and 0.06 ± 0.15, respectively. Sheppard et al. [13] reported two-month postoperative monocular UDVA and CDVA values of 0.19 ± 0.09 and 0.08 ± 0.08, respectively. Alio et al. [8] determined 6-month postoperative monocular UDVA, UIVA, UNVA, CDVA, DCIVA, and DCNVA values of 0.18 ± 0.13, 0.20 ± 0.11, 0.26 ± 0.15, 0.05 ± 0.17, 0.17 ± 0.09, and 0.16 ± 0.13, respectively. The monocular visual outcomes of our study were comparable with the results of previous studies. In an investigation of a Korean population, Kwon et al. [16] reported clinical outcomes of other commercially available trifocal IOLs (AT LISA tri 839 MP) with 6-month postoperative UDVA, UIVA, and UNVA values of 0.00, 0.13, and 0.15 logMAR, respectively. Our visual outcomes were comparable to those of Kwon et al. [16] and slightly better for the UNVA.
Regarding the defocus curve, the optimal visual acuity was obtained at 0.00 D, and there was a second peak at −2.50 D. Previous studies of FineVision trifocal IOLs showed very similar defocus curves, with peaks at 0.00 and −2.50 D and visual acuities greater than 0.2 logMAR from +1.00 to −3.00 D [891314].
In the present study, there were statistically significant myopic results after implantation of the POD FineVision IOL with every formula. In addition, a subgroup analysis of predictive error in both the FineVision POD F group and the FineVision POD FT group showed a similar tendency of myopic shift with statistically significant myopic outcomes in all mentioned formulas. This finding contrasts with previous studies, which reported satisfactory results for postoperative refraction. Poyales et al. [15] identified a high predictability of postoperative refractive outcomes of POD FineVision IOLs with a spherical equivalent of 0.03 ± 0.31 D. The high visual acuity reported in our study likely resulted because the target was set at hyperopia; if the target had been emmetropia, more myopic results would have been attained with fewer uncorrected visual acuities. For this reason, the recent trend in Korea has been to set the refractive target around +0.3 D.
The SRK-II formula demonstrated the largest myopic shift of all formulas considered in the selection of IOL power, with a prediction error of −0.55 ± 0.58 D. Surgeons should be deliberate when choosing the power of POD FineVision IOLs in Korean eyes, especially when using the SRK-II formula.
The authors have no experience with these types of constant and repeated myopic shifts with other commercially available IOLs. Although the number of eyes included in the study was small, the keratometric value, anterior chamber depth, and axial length were mostly within the normal range without any outliers. Although surgeries were carried out at two centers by two different surgeons, the refractive outcomes of FineVision trifocal IOLs from the two centers showed similar tendencies of myopic shift. Therefore, we concluded that the results were unlikely to be driven by a biased distribution of enrolled eyes or the particular surgeon.
The constants used for IOL power calculations are dependent on multiple factors, including the type and material of the IOL, the individual surgeon, the incisional technique, and the patient population [17]. Based on prior observations, the consistent and repeated myopic results for POD FineVision IOLs might be driven by the use of IOL constants of the lens power calculating formulas mainly established in a Western population. In previous reports, some commercially available IOLs have required different IOL constants for an Asian population. Inspection of the ULIB (User Group for Laser Interference Biometry) data revealed differences in IOL constants for the same IOL model between Japanese and non-Japanese eyes, Chinese and non-Chinese eyes, and Indian and non-Indian eyes [19]. This result could be due to differences in ocular biometry between Caucasian and Asian eyes, which are already established in the literature. In previous reports, the anterior segments of Asian eyes are reported to be smaller compared to those of Caucasian eyes [20]. This difference might have led to anteriorization of effective lens position and produced a myopic shift in the present study. Accordingly, caution should be exercised when using IOL constants optimized for other patient populations [22]; for an accurate and precise prediction of refraction, POD FineVision IOLs seem to require new IOL constants in a Korean population.
The limitations of this study include its short follow-up period. However, since there was a significant myopic shift in all mentioned formulas with a p-value <0.001, the authors strongly believe that POD FineVision IOL produces myopic results. In addition, since POD FineVision IOLs were introduced relatively recently in Asia, the tendency of significant myopic shift in a Korean population has significant clinical implications. Deteriorated uncorrected distant visual acuity caused by residual postoperative myopia can greatly decrease patient satisfaction. Because of the severity of the issue at hand, it is necessary for the results to be established, despite a limited follow-up period. Further investigations with larger sample sizes and a longer follow-up period will be necessary to establish new IOL constants.
In summary, POD FineVision IOLs provide excellent distance, intermediate, and near visual outcomes among patients undergoing cataract surgery in a Korean population. However, in terms of refractive predictability, POD FineVision IOLs produce myopic outcomes in a Korean population when IOL power is calculated using IOL constants established in Western countries. Therefore, surgeons who are planning to use POD FineVision IOLs in a Korean population should consider targeting slight hyperopia.
Figures and Tables
 | Fig. 1Preoperative and one-month postoperative monocular defocus curves of the FineVision trifocal intraocular lens. logMAR = logarithm of the minimum angle of resolution. |
Table 1
Demographics and biometry in patients who received a FineVision trifocal intraocular lens implant
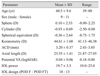
Table 2
Preoperative and one-month postoperative monocular visual acuities in patients implanted with a FineVision trifocal intraocular lens
References
1. Agresta B, Knorz MC, Kohnen T, et al. Distance and near visual acuity improvement after implantation of multifocal intraocular lenses in cataract patients with presbyopia: a systematic review. J Refract Surg. 2012; 28:426–435.

2. Mesci C, Erbil H, Ozdoker L, et al. Visual acuity and contrast sensitivity function after accommodative and multifocal intraocular lens implantation. Eur J Ophthalmol. 2010; 20:90–100.

3. Calladine D, Evans JR, Shah S, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2012; (9):CD003169.

4. Cochener B, Lafuma A, Khoshnood B, et al. Comparison of outcomes with multifocal intraocular lenses: a meta-analysis. Clin Ophthalmol. 2011; 5:45–56.
5. Hutz WW, Eckhardt HB, Rohrig B, Grolmus R. Intermediate vision and reading speed with array, Tecnis, and ReSTOR intraocular lenses. J Refract Surg. 2008; 24:251–256.

6. Jonker SM, Bauer NJ, Makhotkina NY, et al. Comparison of a trifocal intraocular lens with a ‡3.0 D bifocal IOL: results of a prospective randomized clinical trial. J Cataract Refract Surg. 2015; 41:1631–1640.

7. Cochener B. Prospective clinical comparison of patient outcomes following implantation of trifocal or bifocal intraocular lenses. J Refract Surg. 2016; 32:146–151.

8. Alio JL, Montalban R, Pena-Garcia P, et al. Visual outcomes of a trifocal aspheric diffractive intraocular lens with microincision cataract surgery. J Refract Surg. 2013; 29:756–761.

9. Cochener B, Vryghem J, Rozot P, et al. Clinical outcomes with a trifocal intraocular lens: a multicenter study. J Refract Surg. 2014; 30:762–768.

10. Marques EF, Ferreira TB. Comparison of visual outcomes of 2 diffractive trifocal intraocular lenses. J Cataract Refract Surg. 2015; 41:354–363.

11. Mendicute J, Kapp A, Levy P, et al. Evaluation of visual outcomes and patient satisfaction after implantation of a diffractive trifocal intraocular lens. J Cataract Refract Surg. 2016; 42:203–210.

12. Mojzis P, Pena-Garcia P, Liehneova I, et al. Outcomes of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2014; 40:60–69.

13. Sheppard AL, Shah S, Bhatt U, et al. Visual outcomes and subjective experience after bilateral implantation of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2013; 39:343–349.

14. Vryghem JC, Heireman S. Visual performance after the implantation of a new trifocal intraocular lens. Clin Ophthalmol. 2013; 7:1957–1965.

15. Poyales F, Garzon N, Rozema JJ, et al. Stability of a novel intraocular lens design: comparison of two trifocal lenses. J Refract Surg. 2016; 32:394–402.

16. Kwon YK, Kim HK, Lee JH. Clinical outcomes of diffractive trifocal intraocular lens in both eyes: a 6-month follow-up. J Korean Ophthalmol Soc. 2015; 56:1331–1337.

17. Aristodemou P, Knox Cartwright NE, et al. Intraocular lens formula constant optimization and partial coherence interferometry biometry: refractive outcomes in 8108 eyes after cataract surgery. J Cataract Refract Surg. 2011; 37:50–62.

18. Olsen T. Improved accuracy of intraocular lens power calculation with the Zeiss IOLMaster. Acta Ophthalmol Scand. 2007; 85:84–87.

19. User Group for Laser Interference Biometry. Zeiss IOL-Master [Internet]. [place unknown]: User Group for Laser Interference Biometry;2016. cited 2016 Apr 24. Available from: http://ocusoft.de/ulib/c1.htm.
20. Qin B, Tang M, Li Y, et al. Anterior segment dimensions in Asian and Caucasian eyes measured by optical coherence tomography. Ophthalmic Surg Lasers Imaging. 2012; 43:135–142.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download