Abstract
Purpose
To assess the trends in pars plana vitrectomy surgery rates and factors affecting rate change between 2002 and 2013 in South Korea.
Methods
Data from National Health Insurance Service-National Sample Cohort 2002–2013, which represents 1,025,340 samples with a sampling rate of 2.2% from the total eligible Korean population, was analyzed.
Results
A total of 3,816 vitrectomy procedures were performed (male, 2,010; female, 1,806) from 2002 to 2013. Annual rates of vitrectomy increased from 15.1 (in 2002) to 49.4 (in 2013) per 100,000 individuals, and this trend was prominent in those aged 60 years or older. As for the anesthetic method, vitrectomy under local anesthesia increased more prominently than vitrectomy under general anesthesia. The most common diagnoses associated with vitrectomy were diabetic retinopathy, retinal detachment, epiretinal membrane, and macular hole.
The surgical methods and equipment for vitrectomy surgery have been significantly improved since its introduction by Machemer et al. [1]. In its early days, vitrectomy was selectively performed in cases of retinal detachment with large retinal tear or proliferative vitreoretinopathy. However, with the introduction of the sutureless vitrectomy system and wide-field retinal imaging technology, its incidence has increased, and indication of the surgery has widened [23]. Recently, the clinical efficacy and safety were reported for the 27-gauge vitrectomy system, as well as 23- and 25-gauge vitrectomy. Moreover, postoperative complication and patient discomfort have decreased, while the incidence of vitrectomy has increased [45]. Previous studies reported trends in vitreo-retinal surgery in England from 1968 to 2004 [6], and rates of vitrectomy among enrollees in a managed care network from 2001 to 2012 [7]. However, vitrectomy rate and trends in South Korean patients have not been previously reported. Thus, in this study, we evaluated the vitrectomy rate and its changes in the South Korean population.
This study adhered to the tenets of the Declaration of Helsinki and was waived for the requirement of written informed consent. The design of this study was approved by the institutional review board of the National Health Insurance Service Ilsan Hospital, Goyang, Korea.
The Korean National Health Insurance Service (KNHIS) enrolls more than 97% of the entire Korean population. We used the data of National Health Insurance Service-National Sample Cohort (NHIS-NSC) 2002–2013, which is provided by KNHIS [8]. A representative 1,025,340 samples were randomly selected using 1,476 strata, comprising 2.2% of the total eligible Korean population in 2002. During the follow-up period, in order to make the sample size similar across the years and to compensate for the annual decrease of cohort size due to eligibility disqualifications from KNHIS (death, immigration, etc.), the dynamic cohort was refreshed annually by adding newborns, who were sampled using the 2.2% sampling rate [8]. This database provides detailed information from 2002 to 2013 on procedures and prescription drugs, as well as diagnostic codes and personal information.
In KNHIS, all types of medical information are exchanged via Korean electronic data interchange (KEDI) code between all medical facilities including government, any medical providers, and public health centers. We defined pars plana vitrectomy (PPV) based on the KEDI code of S5121. Age groups were divided by 10-year intervals, and participant residence was divided into 16 Si or Do areas. We identified the major disease code (Korean Classification of Diseases [KCD], Hxx.xx) for PPV based on the same claim. Until KCD version 5 (~2010), the disease code included one decimal place (i.e., Hxx.x), and it was impossible to identify an exact cause of PPV. From KCD version 6 (2011~), the KCD code provided more detailed disease code, including two decimal places (i.e., Hxx.xx); therefore, we estimated major disease cause for PPV from 2011. We also identified the use of general anesthesia for PPVbased claims on the same day, which is associated with general anesthesia including endotracheal procedures.
Annual participants were defined as all participants with NHIS qualification on January 1 of each year. The incidence of PPV was calculated using the total number of PPV and annual participants and was calculated with 95% confidence interval based on a Poisson distribution. The overall incidence density was also calculated. We provided the number of PPV patients by subgroup of gender, year, age group, residence area, and medical provider location. Major causative diseases for PPV were inferred from 2011 using KCD version 6, which offers a more detailed code for retinal disease than the previous version of KCD. The Stata/MP, ver. 14.0 (StataCorp., College Station, TX, USA) was used.
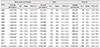
Table 1 shows the number of participants, number of performed PPV procedures, and annual rate of PPV per 100,000 individuals in both male and female, male, and female groups from 2002 to 2013. The sample size remained approximately 100,000 (998,527 in 2009–1,025,340 in 2002), and a total of 3,816 cases of vitrectomy were performed between 2002 and 2013. There was a steady increase in vitrectomy cadence from 2002 to 2013 (115 cases in 2002 and 501 cases in 2013). The rate of vitrectomy per 100,000 individuals was 31.5 cases during the decade, and there was a more than three-fold increase in the overall vitrectomy rate from 2002 (15.1 vitrectomies per 100,000 people) to 2013 (49.4 vitrectomies per 100,000 people). Fig. 1 clearly shows the increase in annual vitrectomy rate. When stratified according to sex, a total of 2,010 vitrectomies in males and 1,806 vitrectomies in females were performed during 12 years, and the vitrectomy rate was slightly higher in males (33.1 per 100,000 individuals) than in females (28.4 per 100,000 individuals).
Table 2 shows the annual incidence of vitrectomy according to age. A total of eight vitrectomies were performed in the group aged 9 years or less. The incidence seems to increase with older age. Over the 12-year period, a total of 1,165 cases of vitrectomy were performed in individuals in their 60s, represent the highest frequency among the age groups, and the incidence was lower (815) in those aged 70 years or older. However, individuals aged 70 years or older showed the greatest increase in vitrectomy incidence over the 12-year period (from 16 cases in 2002 to 142 cases in 2013).
Table 3 shows the presumed diagnostic causes for vitrectomy, based on the principal diagnosis registered at the time of vitrectomy. The diagnosis was provided with a four-digit number from 2011, and there were a total of 1,388 cases until 2013. However, in approximately one-third of the vitrectomy cases (385), the exact diagnostic cause was unclear, because the registered diagnosis was not clearly stated, including “unspecified” or “other”. The most common diagnosis was diabetic retinopathy (441 cases). The other diagnoses were retinal detachment, epiretinal membrane, macular hole, and lens (intraocular or crystalline) in descending order of frequency.
Fig. 2 shows the annual incidence of vitrectomy by anesthetic method. There was a noticeable increase in local vitrectomy versus vitrectomy performed under general anesthesia.
This analysis of data from the NHIS-NSC shows a more than three-fold steady increase in vitrectomies over the 12 years, from 15.1 (2002) to 31.5 (2013) episodes per 100,000 people. An average of 31.5 cases were performed annually during the same period.
No previous research about a similar topic has been performed in South Korea, and there were only two studies abroad. According to the study that was performed in England from 1968 to 2004, which analyzed the trends in vitreo-retinal surgery including scleral buckling vitrectomy, the annual rate of vitrectomy was fewer than one episode per 100,000 individuals in 1968 [6]. The operation rates persisted at this level for 20 years until 1987, and then rose sharply to approximately 26 (Hospital Episode Statistics) or 27 (Oxford Record Linkage Study) by 2004. In our study, the operation rate in 2004 was 22.8 per 100,000 people, showing similar results and its trend of rising incidence. The rate of vitrectomy also increased in the United States [7]. Analysis of the patients with codes for any eye-related diagnosis or procedural code for any eye-related visits among the enrollees of Managed Care Network between 2001 and 2012 showed an overall 31% increase in vitrectomy rate from 2001 to 2012 (from 1.47 to 1.92 per 1,000 individuals). Over the 12-year period, patients aged 65 years or older had the greatest overall rate of vitrectomy (3.81 to 4.52 per 1,000 patients), while those 40 to 64 years of age had the greatest increase in vitrectomy rate (81%). However, since this study evaluated claims from only one particular large managed care network and those with codes for ophthalmologic diagnosis or procedure, cautious interpretation is mandatory when applying these results, such as vitrectomy rate, to the total population.
The vitrectomy rates are increasing in England, United States, and South Korea, and the possible explanations for this trend are as follows. After introduction of small-gauge vitrectomy, such as the 25-gauge system in 2002 and the 23-gauge system in 2005, in the early period, there were disadvantages and surgical complications associated with these smaller gauge systems, such as postoperative hypotony or endophthalmitis [4]. However, with the modification of surgical technique and increased surgeon experience with the new equipment, smaller-gauge vitrectomy has been recognized as safe and offers shorter operative time in spite of the early concerns. Moreover, a wide-angle viewing system such as binocular indirect ophthalmomicroscope (BIOM) facilitates all vitreoretinal surgical procedures. Incidence of vitrectomy performed under local anesthesia increased more significantly than that performed under general anesthesia (Fig. 2). It seems that local anesthesia is increasingly preferred because the operation time is short, and greater patient convenience can be achieved [9]. These factors may have contributed to the increased vitrectomy rates.
Our results showed a higher incidence of vitrectomy in older age groups, and those in their 60s had the highest rate of vitrectomy (Table 2). The group with the greatest increase in vitrectomy rate was the patients aged 70 years or older, increasing from 16 cases in 2002 to 142 cases in 2013. Given this active surgical treatment in the elderly, when we consider the longer life expectancy, as well as the rapid rate of population aging in South Korea and its entrance into a super-aged society by 2026, the rate of vitrectomy is expected to continually rise.
We attempted to define the common causes of vitrectomy; however, there was significant limitation because certain diagnoses could be identified only after the sixth revision of KCD in 2012 (Table 3). Supposedly, common diagnoses were complications of diabetic retinopathy, retinal detachment, epiretinal membrane, macular hole, and dislocation of intraocular lens. From 2011 to 2013, the numbers of annual cases were similar; however, macular puckering cases showed an increasing trend (22 cases in 2011, 42 cases in 2012, and 62 cases in 2013). Current International Statistical Classification of Disease and Related Health Problems and KCD are based on anatomical classification, making it slightly inappropriate for ophthalmic disease. To improve accuracy and applicability of health insurance claim data, refinements to the diagnostic system, especially those with large economic burden, must be performed.
When analyzed by age group, in the age group of 70 years and older, there were six cases of local vitrectomy in 2002, 12 cases of local vitrectomy in 2003, and the incidence gradually increased to 101 cases of local vitrectomy in 2013, representing more than a 10-fold increase over the 12-year period. There was a three- to four-fold increase of vitrectomy incidence in the 50s age group and about a four-fold increase in the 60s age group between 2002 and 2013, confirming increased local vitrectomy rates in the aged population.
Our study has inevitable limitations as an analysis tool using health insurance claim data [10]. First, the cohort consisted of 2.2% of the eligible Korean population in 2002 by stratified random sampling; therefore, it had high representativeness in 2002. However, when adding newborns to the cohort starting in 2003, income was not included in its stratification; hence, the representativeness might have decreased over subsequent years [8]. Second, because of its separation from medical health insurance claim data, our study lacks information on the exact preoperative diagnosis for the surgery or the severity of the diagnosis. However, despite these limitations, this study has value as a baseline for analyzing and predicting the future trends of vitrectomy in Korea.
In conclusion, we analyzed data from a sample cohort of approximately one million people and assessed the rate of vitrectomy performed in South Korea. From 2002 to 2013, the average annual incidence was 31.5 per 100,000 people. The increasing rate of the vitrectomy has been steady, especially in the elderly; when considering the population trends with a foreseen entrance into a super-aged society, vitrectomy is expected to increase in the future in South Korea.
Figures and Tables
Acknowledgements
This work was supported by a National Health Insurance Service Ilsan Hospital Grant (NHIMC 2016-46). This study used the NHIS-NSC 2002-2013 (NHIS-2016-2-089), which was released by the KNHIS. The authors alone are responsible for the content and writing of the paper.
References
1. Machemer R, Buettner H, Norton EW, Parel JM. Vitrectomy: a pars plana approach. Trans Am Acad Ophthalmol Otolaryngol. 1971; 75:813–820.
2. Cho YJ, Lee JM, Kim SS. Vitreoretinal surgery using transconjunctival sutureless vitrectomy. Yonsei Med J. 2004; 45:615–620.
3. Jin SY, Choi MJ, Kim CG, Kim JW. A combination of 23-gauge and 20-gauge transconjunctival sutureless vitrectomy. J Korean Ophthalmol Soc. 2008; 49:65–70.
4. Kim MJ, Park KH, Hwang JM, et al. The safety and efficacy of transconjunctival sutureless 23-gauge vitrectomy. Korean J Ophthalmol. 2007; 21:201–207.
5. Park JH, Kim MH, Sagong M, Chang WH. Silicone oil with short-term prone position in macular hole retinal detachment surgery in high myopia. J Korean Ophthalmol Soc. 2015; 56:1566–1571.
6. El-Amir AN, Keenan TD, Abu-Bakra M, et al. Trends in rates of retinal surgery in England from 1968 to 2004: studies of hospital statistics. Br J Ophthalmol. 2009; 93:1585–1590.
7. Wubben TJ, Talwar N, Blachley TS, et al. Rates of vitrectomy among enrollees in a United States Managed Care Network, 2001-2012. Ophthalmology. 2016; 123:590–598.
8. Lee J, Lee JS, Park SH, et al. Cohort profile: The National Health Insurance Service-National Sample Cohort (NHISNSC), South Korea. Int J Epidemiol. 2017; 46:e15.
9. Li CL, Liu DT, Chan WM, Lam DS. Local anesthesia for vitrectomy. Ophthalmology. 2006; 113:1887–1888.
10. Rim TH, Oh J, Lee CS, et al. Evaluation of the association between retinal vein occlusion and the risk of atrial fibrillation development: a 12-year, retrospective nationwide cohort study. Sci Rep. 2016; 6:34708.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download