Abstract
Purpose
To assess the validity of central corneal thickness (CCT) and corrected intraocular pressure (IOP) values obtained by tono-pachymetry in non-surgical and post-photorefractive keratectomy (PRK) eyes.
Methods
For the study, 108 young healthy participants and 108 patients who had PRK were enrolled. Measurements were randomly performed by tono-pachymetry, ultrasonic (US) pachymetry, and Goldmann applanation tonometry (GAT). CCT measurement by tono-pachymetry was compared to that of US pachymetry. The corrected IOP value obtained by tono-pachymetry was compared to that obtained by US pachymetry and GAT. The corrected IOP from US pachymetry and GAT was calculated using the identical compensation formula built into the tono-pachymetry. Bland-Altman plot and paired t-test were conducted to evaluate the between-method agreements.
Results
The mean CCT measurement using tono-pachymetry was significantly greater by 7.3 µm in non-surgical eyes (p < 0.001) and 17.8 µm in post-PRK eyes (p < 0.001) compared with US pachymetry. Differences were significant in both Bland-Altman plotand paired t-test. The mean difference of corrected IOP values obtained by tono-pachymetry and calculated from measurements by US pachymetry and GAT was 0.33 ± 0.87 mmHg in non-surgical eyes and 0.57 ± 1.08 mmHg in post-PRK eyes. The differences in the Bland-Altman plot were not significant.
Conclusions
The CCT measurement determined using tono-pachymetrywas significantly thicker than that of US pachymetry. The difference in CCT was greater in post-PRK eyes than in non-surgical eyes. However, the corrected IOP value obtained by tono-pachymetry showed reasonable agreement with that calculated from US pachymetry and GAT measurements.
Central corneal thickness (CCT) influences tonometry measurements. Accurate determination of intraocular pressure (IOP) requires correction of tonometry readings according to CCT [1234]. The effect of CCT on IOP measurements are such that a 10% difference in CCT could result in a 3.4 mmHg difference in IOP [45]. Corneal refractive surgery has become more popular than in the past due to improvements in visualand safety outcomes. Corneal refractive surgery leads to reduced tonometry readings. The reduction in IOP measurements may delay recognition and treatment of glaucoma in the absence of careful attention to the effect of the reduced CCT on IOP measurements in these patients [6]. Ultrasonic (US) pachymetry has been widely accepted as the gold standard for corneal thickness measurement. US pachymetry is the most commonly used method to measure CCT because of its portability, cost effectiveness, and ease of use [789]. However, US pachymetry has disadvantages, such as the need for topical anesthesia and direct contact with the cornea, with an inherent risk of epithelial erosion, infection transmission, and operator dependence [910].
In recent years, several combination units of non-contact tonometry and pachymetry have been developed. Tono-pachymetry simultaneously measures CCT using the principle of the Scheimpflug camera system and IOP using a conventional non-contact tonometry method. The CCT-corrected IOP is then automatically calculated. Tono-pachymetry is patient-friendly and time-saving, but it has not been well documented whether the corrected IOP values obtained from tono-pachymetry are comparable to those derived from conventional US pachymetry and Goldmann applanation tonometry (GAT) as the gold standard for measuring CCT and IOP [1112].
In this study, we assessed the validity of the corrected IOP value obtained by tono-pachymetry in non-surgical and post-photorefractive keratectomy (PRK) eyes.
This research adhered to the tenets of the Declaration of Helsinki. The institutional review board approved the research, and the patients provided informed consent (IRB-ROK-MND-2014-KMMRP-019). This study was conducted in Aerospace Medical Center, Republic of Korea Air Force.
All patients underwent a complete ophthalmic examination including visual acuity, IOP, refraction, slit lamp biomicroscopy, and fundus examination. In the non-surgical group, 108 young healthy individuals were enrolled. Subjects with non-refractive ocular abnormalities, including ocular or systemic diseases that may affect the cornea, and those with a history of ocular surgery or trauma were excluded.
In the post-PRK group, 108 participants who had undergone advanced surface ablation PRK to correct myopia at least 6 months before enrollment were enrolled. Subjects with any ocular pathology such as keratectasia, cataract, and glaucoma and those with any post-surgical complications were excluded.
Measurements were randomly performed by tono-pachymetry (TX-20P; Canon, Tokyo, Japan), US pachymetry (US-4000; Nidek, Gamagori, Japan), or GAT (AT-900; Haag-Streit, Bern, Switzerland). All measurements were made on both eyes of the participants; however, only one eye of each participant was randomly selected for analyses. A block randomization was performed with a block size of 10 participants.
For each individual, all measurements were performed within a 10-minute period by a single experienced examiner. Measurement using tono-pachymetry was conducted with the patient seated using a chin rest and head rest. The patient was instructed to look at a fixation target. Five CCT measurements and three IOP measurements were obtained. The CCT-corrected IOP was calculated automatically using the following compensation formula [13]:
Assessment of CCT using US pachymetry was made after corneal anesthesia with topical application of 0.5% proparacaine with the patient in the sitting position. Five CCT measurements were obtained. Three IOP measurements were performed using the conventional GAT method. Briefly, the cornea was anesthetized with a topical preparation of 0.5% proparacaine, and the tear film was stained with a fluorescein strip. With the cornea and biprism illuminated by a cobalt blue light from the slit lamp, the biprism is brought into gentle contact with the apex of the cornea. The fluorescent semicircles were viewed through the biprism, and the force against the cornea was adjusted until the inner edges overlapped. The IOP was then read directly from a scale on the tonometer housing. Calibration error testing was performed for every 10 consecutive measurements, as recommended by the manufacturer using the standard calibration error check weight bar. The average values of three measurements were used for analyses. The corrected IOP that corresponded to measurements by US pachymetry and GAT was calculated with the aforementioned formula.
Repeatability of CCT measurement with each instrument was established by the intraclass correlation coefficient (ICC) and the coefficient of variation (COV). Differences in CCT, IOP, and corrected IOP measurements between instruments were evaluated by the paired sample t-test. Bland-Altman plot was used to demonstrate the between-method agreement [1415]. Additionally, correlation analysis was conducted between the refractive error and the differences in corrected IOP between the two devices.
All statistical analyses were conducted by the MedCalc software ver. 12.1.4 (Medisoftware, Mariakerke, Belgium). A p-value less than 0.05 was considered statistically significant.
One hundred eight eyes of 108 healthy participants and 108 eyes of 108 post-PRK subjects were evaluated. The mean age was 22.38 ± 3.23 years in non-surgical eyes and 25.12 ± 3.75 years in post-PRK eyes. The sex ratio (male / female) was 2.63 in non-surgical eyes and 1.92 in post-PRK eyes. The average spherical equivalent refractive error was −2.34 ± 2.64 diopter in non-surgical eyes and −0.07 ± 0.36 diopter in post-PRK eyes.
Tono-pachymetry yielded an ICC of 0.984 (95% confidence interval [CI], 0.981–0.987) and a COV of 0.69% in non-surgical eyes; an ICC of 0.981 (95% CI, 0.975–0.987) and a COV of 0.70% in post-PRK eyes. US pachymetry yielded an ICC of 0.976 (95% CI, 0.971–0.981) and a COV of 0.71% in non-surgical eyes; an ICC of 0.967 (95% CI, 0.957–0.977) and a COV of 0.73% in post-PRK eyes. Both devices demonstrated an ICC >0.9, which is sufficient to ensure reasonable validity [16]. Tono-pachymetry yielded slightly higher ICC and lower COV values compared to US pachymetry, which indicated a higher degree of repeatability (Table 1).
Tono-pachymetry yielded an ICC of 0.967 (95% CI, 0.939–0.984) and a COV of 2.84 % in non-surgical eyes; an ICC of 0.972 (95% CI, 0.957–0.987) and a COV of 2.33% in post-PRK eyes. GAT yielded an ICC of 0.943 (95% CI, 0.889–0.973) and a COV of 4.78% in non-surgical eyes; an ICC of 0.949 (95% CI, 0.914–0.974) and a COV of 4.25% in post-PRK eyes. Tono-pachymetry yielded a slightly higher ICC and lower COV values compared to GAT, which indicated a higher degree of repeatability (Table 2).
The average CCT measurement by tono-pachymetry and US pachymetry was 549.40 ± 31.10 µm and 542.05 ± 35.58 µm in non-surgical eyes, respectively, and 495.73 ± 46.03 µm and 477.96 ± 48.77 µm in post-PRK eyes. Tono-pachymetry yielded CCT measurements that were greater by 7.35 ± 11.37 µm in non-surgical eyes (p < 0.001) (Fig. 1A), and by 17.76 ± 12.09 µm in post-PRK eyes (p < 0.001) (Fig. 1B), compared with US pachymetry. The differences were significant by the paired t-test (Table 3).
The mean IOP measurement by tono-pachymetry and GAT was 17.24 ± 2.89 mmHg and 17.27 ± 2.83 mmHg in non-surgical eyes, respectively, and 15.12 ± 2.77 mmHg and 15.24 ± 2.79 mmHg in post-PRK eyes. The differences were not significant by the paired t-test (Table 3).
In Bland-Altman plot, IOP obtained by tono-pachymetry and US pachymetry showed close agreement, with the mean difference centered around zero, and 95% of the points were accurately located between the predicted 95% limits of agreement in both non-surgical eyes (Fig. 2A) and post-PRK eyes (Fig. 2B). The parameters of slope and intercept of the regression equation in both non-surgical eyes and post-PRK eyes were not significant.
The average corrected IOP value obtained by tono-pachymetry and calculated from measurements by US pachymetry and GAT was 17.26 ± 3.37 mmHg and 17.59 ± 3.43 mmHg in non-surgical eyes and 17.37 ± 3.79 mmHg and 17.93 ± 3.76 mmHg in post-PRK eyes, respectively. The mean difference was 0.33 ± 0.87 mmHg in non-surgical eyes (p < 0.001) and 0.57 ± 1.08 mmHg in post-PRK eyes (p < 0.001). Differences were significant by the paired t-test (Table 3).
In the Bland-Altman plot, corrected IOP obtained by tono-pachymetry and US pachymetry-GAT showed close agreement, with the mean difference centered around zero, and 95% of the points were accurately located between the predicted 95% limits of agreement in both non-surgical eyes (Fig. 3A) and post-PRK eyes (Fig. 3B). The parameters of slope and intercept of the regression equation in both non-surgical eyes and post-PRK eyes were not significant.
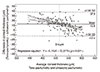
In correlation analyses, there were no significant correlations between spherical equivalent refractive error and differences in corrected IOP between the two devices in either non-surgical eyes (p = 0.983) or post-PRK eyes (p = 0.875) (Fig. 4A and 4B).
Newly introduced instruments should be evaluated for repeatability and should be compared with former instruments to determine the interchangeability of methods before they are widely applied in clinical practice. The combination unit of non-contact tonometry and pachymetry is a recently developed instrument. There are few previous studies that evaluated this device, and the results are inconsistent [1718].
Fujimura et al. [10] demonstrated that tono-pachymetry (NT-530P, Nidek) offered high repeatability and reproducibility in both IOP and CCT measurements. Garcia-Resua et al. [11] showed that uncorrected IOP measurement by tono-pachymetry (NT-530P) did not differ significantly from that obtained by another non-contact tonometer (TX-10, Canon ) and GAT readings. Schiano et al. [17] examined IOP and CCT measurements with tono-pachymetry (NT-530P) and assessed agreement of the device with GAT and US pachymetry in 62 eyes of normal subjects. On average, tono-pachymetry overestimated the IOP by 1.3 mmHg compared with GAT. CCT readings with tono-pachymetry were on average 13 µm thinner than the readings obtained with US pachymetry. Han et al. [18] compared the IOP values measured using tono-pachymetry (NT-530P) and GAT in the same eyes of 26 patients before and after laser-assisted subepithelial keratectomy. CCT was also measured by tono-pachymetry and US pachymetry before and after surgery. Differences in IOP measurement between tono-pachymetry and GAT were not significant in the paired t-test before and after laser-assisted subepithelial keratectomy. Tono-pachymetry overestimated CCT measurements by 3.37 µm before surgery and by 6.27 µm after surgery compared with US pachymetry.
In the present study, the mean CCT measurement using tono-pachymetry was significantly thicker than that obtained using US pachymetry, by 7.35 ± 11.37 µm in non-surgical eyes and 17.76 ± 12.09 µm in post-PRK eyes. The extent of overestimation of CCT was greater in post-PRK eyes than innon-surgical eyes. The probe-corneal contact with US pachymetry may be responsible for these results. Probe-corneal contact can yield thinner CCT readings as a result of tissue indentation [12] and displacement of the tear film [19]. This effect can be greater in athinner cornea, including post-PRK eyes. In the Bland-Altman plot, CCT measurement by tono-pachymetry and US pachymetry showed close agreement with the clinically acceptable range of limits of agreement. However, regression equations of the Bland-Altman plot were significant in both non-control eyes and post-PRK eyes. When Bland-Altman plots of non-surgical eyes and post-PRK eyes were merged, the average difference in CCT measurement between tono-pachymetry and US pachymetry was 12.8 µm (Fig. 5). Additionally, the regression analysis showed that tono-pachymetry tended to underestimate CCT for thicknesses greater than 514 µm and tended to overestimate CCT for thicknesses less than 514 µm when compared to the US pachymetry measurement. The exact reason for this result is unclear; however, methodological properties inherent to the device may have partly contributed to this tendency.
The IOP measurement by tono-pachymetry showed a reasonable agreement with that obtained by GAT in both non-surgical eyes and post-PRK eyes. The difference of IOP value between tono-pachymetry and GAT was not significant in paired t-test. The Bland-Altman plot demonstrated a very close agreement between the IOP measurement by tono-pachymetry and US pachymetry. The mean difference in IOP measurement was 0.0 mmHg in non-surgical eyes and 0.2 mmHg in post-PRK eyes.
The corrected IOP value obtained by tono-pachymetry showed a reasonable agreement with that calculated from US pachymetry and GAT measurements. The difference in corrected IOP value between tono-pachymetry and US pachymetry and GAT was significant by the paired t-test. However, the mean discrepancy was 0.33 mmHg in non-surgical eyes and 0.57 mmHg in post-PRK eyes, which is too small to produce any clinical effect. The Bland-Altman plot demonstrated very close agreement between the corrected IOP obtained by tono-pachymetry and US pachymetry.
There were some limitations in this study. The GAT examiner was not masked to the IOP readings using tono-pachymetry, eyes with high or low IOP were not included, and only very young subjects were included.
In conclusion, the CCT and IOP measurements by tono-pachymetry had a high level of repeatability. CCT measurement obtained using tono-pachymetry was significantly thicker than that obtained using US pachymetry, and the difference in CCT was greater in post-PRK eyes than non-surgical eyes. The corrected IOP value obtained by tono-pachymetry showed reasonable agreement with that calculated from US pachymetry and GAT measurements.
Figures and Tables
 | Fig. 1Bland-Altman plots of central corneal thickness in non-surgical eyes (A) and post-photorefractive keratectomy eyes (B). SD = standard deviation. |
 | Fig. 2Bland-Altman plots of intraocular pressure in non-surgical eyes (A) and post-photorefractive keratectomy eyes (B). SD = standard deviation. |
 | Fig. 3Bland-Altman plots of corrected intraocular pressure in non-surgical eyes (A) and post-photorefractive keratectomy eyes (B). SD = standard deviation. |
 | Fig. 4Scatter diagram and regression line of correlation analyses between refractive error and the differences in corrected intraocular pressure between the two devices in non-surgical eyes (A) and post-photorefractive keratectomy eyes (B). D = diopter. |
 | Fig. 5Merged Bland-Altman plot and regression equation of central corneal thickness of non-surgical eyes and post-photorefractive keratectomy eyes. SD = standard deviation. |
Acknowledgements
This work was supported by the Korean Military Medical Research Project funded by the ROK Ministry of National Defense (ROK-MND-2014-KMMRP-019).
References
1. Ehlers N, Bramsen T, Sperling S. Applanation tonometry and central corneal thickness. Acta Ophthalmol (Copenh). 1975; 53:34–43.
2. Whitacre MM, Stein RA, Hassanein K. The effect of corneal thickness on applanation tonometry. Am J Ophthalmol. 1993; 115:592–596.
3. Stodtmeister R. Applanation tonometry and correction according to corneal thickness. Acta Ophthalmol Scand. 1998; 76:319–324.
4. Doughty MJ, Zaman ML. Human corneal thickness and its impact on intraocular pressure measures: a review and meta-analysis approach. Surv Ophthalmol. 2000; 44:367–408.
5. Bron AM, Creuzot-Garcher C, Goudeau-Boutillon S, d'Athis P. Falsely elevated intraocular pressure due to increased central corneal thickness. Graefes Arch Clin Exp Ophthalmol. 1999; 237:220–224.
6. Mardelli PG, Piebenga LW, Whitacre MM, Siegmund KD. The effect of excimer laser photorefractive keratectomy on intraocular pressure measurements using the Goldmann applanation tonometer. Ophthalmology. 1997; 104:945–948.
7. Gonzalez-Meijome JM, Cervino A, Yebra-Pimentel E, Parafita MA. Central and peripheral corneal thickness measurement with Orbscan II and topographical ultrasound pachymetry. J Cataract Refract Surg. 2003; 29:125–132.
8. Williams R, Fink BA, King-Smith PE, Mitchell GL. Central corneal thickness measurements: using an ultrasonic instrument and 4 optical instruments. Cornea. 2011; 30:1238–1243.
9. Sedaghat MR, Daneshvar R, Kargozar A, et al. Comparison of central corneal thickness measurement using ultrasonic pachymetry, rotating Scheimpflug camera, and scanning-slit topography. Am J Ophthalmol. 2010; 150:780–789.
10. Fujimura F, Kamiya K, Fujiwara K, et al. Repeatability and reproducibility of measurements using a NT-530P noncontact tono/pachymeter and correlation of central corneal thickness with intraocular pressure. Biomed Res Int. 2013; 2013:370592.
11. Garcia-Resua C, Pena-Verdeal H, Minones M, et al. Reliability of the non-contact tono-pachymeter Tonopachy NT-530P in healthy eyes. Clin Exp Optom. 2013; 96:286–294.
12. Barkana Y, Gerber Y, Elbaz U, et al. Central corneal thickness measurement with the Pentacam Scheimpflug system, optical low-coherence reflectometry pachymeter, and ultrasound pachymetry. J Cataract Refract Surg. 2005; 31:1729–1735.
13. Kohlhaas M, Boehm AG, Spoerl E, et al. Effect of central corneal thickness, corneal curvature, and axial length on applanation tonometry. Arch Ophthalmol. 2006; 124:471–476.
14. Bland JM, Altman DG. Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet. 1995; 346:1085–1087.
15. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986; 1:307–310.
16. Portney LG, Watkins MP, editors. Foundations of clinical research: applications to practice. Upper Saddle River: Pearson/Prentice Hall;2009. p. 588–597.
17. Schiano Lomoriello D, Lombardo M, Tranchina L, et al. Repeatability of intra-ocular pressure and central corneal thickness measurements provided by a non-contact method of tonometry and pachymetry. Graefes Arch Clin Exp Ophthalmol. 2011; 249:429–434.
18. Han KE, Kim H, Kim NR, et al. Comparison of intraocular pressures after myopic laser-assisted subepithelial keratectomy: tonometry-pachymetry, Goldmann applanation tonometry, dynamic contour tonometry, and noncontact tonometry. J Cataract Refract Surg. 2013; 39:888–897.
19. Amano S, Honda N, Amano Y, et al. Comparison of central corneal thickness measurements by rotating Scheimpflug camera, ultrasonic pachymetry, and scanning-slit corneal topography. Ophthalmology. 2006; 113:937–941.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download