Abstract
Purpose
The aim of this study was to investigate the incidence and associated clinical factors of delayed absorption of subretinal fluid (SRF) after surgery for rhegmatogenous retinal detachment.
Methods
This study involved 36 eyes of 36 consecutive patients who underwent successful surgery for rhegmatogenous retinal detachment. A complete ophthalmologic evaluation, including clinical fundus examination, optical coherence tomography, and indocyanine green angiography, was conducted before and after surgery. Delayed absorption was defined as the presence of residual concave SRF or an SRF bleb at 6 months after surgery. Clinical factors and choroidal features on indocyanine green angiography were compared according to the presence and absence of delayed absorption.
Results
Eighteen of 36 eyes (50%) showed delayed absorption. Macular involvement and worse preoperative visual acuity were significantly related to the presence of delayed absorption (p = 0.001 and p = 0.034, respectively). On indocyanine green angiography, preoperative choroidal vascular hyperpermeability was noted in 70% of eyes with delayed absorption and in 14% of eyes without it (p = 0.010).
Conclusions
Delayed absorption of SRF after retinal reattachment surgery was not rare, with a 50% of incidence in this study. Macula-off status was significantly related to the incidence of delayed SRF absorption, and choroidal features such as choroidal vascular hyperpermeability might be responsible in part, possibly through the resultant exudative property of choroid.
Persistent subretinal fluid (SRF) may exist after surgery for rhegmatogenous retinal detachment (RRD), even when the retina appears fully attached on ophthalmoscopic examination. Machemer [1] first reported on persistent SRF with owl monkeys in 1983. The introduction of optical coherence tomography (OCT), a useful, noninvasive diagnostic method to detect SRF that cannot be appreciated on clinical examination, made possible the observation of persistent fluid after RRD surgery in multiple studies [2345678]. The incidence of SRF varies from 25% to 70% at 4 to 6 weeks postoperation. Delayed absorption at up to 6 months postoperation has been reported to a lesser degree, and there have been only a few reports with such a long-term follow-up.
Accumulation of SRF can also develop in the form of a SRF bleb around the posterior pole after scleral buckling for RRD [9]. In the study, choroidal vascular congestion and choroidal vascular hyperpermeability (CVH) were identified on indocyanine green angiography (ICGA). The choroidal layer is thought to play a significant role in physiologic retinal attachment. Considering the importance of choriocapillary ischemia and retinal pigment epithelial dysfunction in serous or exudative retinal detachments, there is a possibility that choroidal characteristics influence the absorption of SRF.
The purpose of this study was to investigate the incidence and associated factors of delayed absorption of SRF after surgery for RRD, including choroidal features on ICGA.
We conducted a study of 36 eyes from 36 consecutive patients who underwent a scleral buckling procedure and/or vitrectomy for primary RRD at Samsung Medical Center from January 2011 to September 2014. This study was approved by the institutional review board (No. 2012-01-017), and the work was carried out in accordance with the Declaration of Helsinki. Patients who consented to participate in this study were enrolled. Before the surgery, all patients provided informed consent for participation in this study. Informed consent regarding ICGA was also received from patients who agreed to the study.
This study included only the eyes with successful retinal reattachment after the initial operation. All patients were evaluated at 1 week, 1 month, 3 months, and 6 months after surgery. Exclusion criteria included reoperation from primary failure or redetachment, long-standing RRD with duration of more than 3 months, proliferative vitreoretinopathy grade C or more, diabetic retinopathy, short follow-up period of less than 6 months, history of previous vitreoretinal surgery, and pre-existence of macular pathology, intraocular inflammation, or advanced glaucoma. Patients who followed up for more than 6 months after the surgery were enrolled. In cases with complete absorption of SRF, follow-up visit was not required. In cases with delayed absorption, follow-up visits were arranged to evaluate the changes in SRF until complete absorption. Assuming that SRF was caused by CVH, photodynamic therapy was performed in patients with residual shallow SRF.
Surgical treatments for RRD were conducted by one retinal surgeon (SWK). Patients underwent elective surgery for RRD rather than emergency surgery. The duration between initial diagnosis of RRD and surgery ranged from 1 to 4 days. Patients with failed reattachment after first surgery received a second surgery. The selection of reattachment surgery for this study was determined by the surgeon based on each patient's condition. Generally, scleral buckling was performed for the following conditions: presence of retinal break located near the vitreous base or inferior retina, retinal dialysis, and retinal detachment associated with atopy. Vitrectomy was performed for the following conditions: presence of a large retinal break (more than 3 clock hour), a retinal break located near the posterior retina, or if more than 3 point buckle were needed. For those who received segmental scleral buckling, application of cryotherapy to retinal breaks was done before a radially- or circumferentially-oriented scleral explant was positioned to seal the break. The explant was a silicone sponge with a width of 5.0 mm (506 type; MIRA Inc., Waltham, MA, USA). Generally, external SRF drainage was not performed. In cases with severe bullous detachment, drainage was performed so that a retinal break could be placed in juxtaposition to the buckle. Before suture of the conjunctiva, the scleral explant and scleral wound were irrigated with diluted gentamicin. For those who underwent vitrectomy, standard vitrectomy utilizing a 23-gauge suture-less system (Constellation, Alcon Surgical, Fort Worth, TX, USA; Associate, DORC International, Zuidland, The Netherlands) was performed. Perfluorocarbon liquid was injected over the optic disc and flattened retina. All retinal breaks were treated with endolaser photocoagulation after fluid-air exchange. Air-gas exchange (approximately 50 mL) with perfluoropropane or sulfur hexafluoride gas was performed at the surgeon's discretion.
Demographic data including age, gender, and presence of diabetes or hypertension were collected, and complete ophthalmologic examination including best-corrected visual acuity, intraocular pressure, slit-lamp examination, fundus examination with indirect ophthalmoscopy, and imaging studies using OCT and ICGA were performed. Axial length was measured, and lens status, preoperative macular status, extent of retinal detachment in number of quadrants, and number of retinal breaks were documented.
OCT and ICGA examinations were performed before and after surgery. All patients underwent an enhanced depth imaging OCT examination using Spectralis (Heidelberg Engineering, Germany). Vertical, horizontal, and six radial OCT scans through the fovea were obtained for both eyes preoperatively and at 1 week, 1 month, 3 months, and 6 months postoperatively. In cases with peripherally located SRF outside the central 30°, peripheral OCT images were retrieved whenever possible. ICGA examinations were performed with Spectralis HRA+OCT (Heidelberg Engineering) in both eyes of each patient preoperatively and at 1 month postoperatively. Panoramic ICGA images that covered the posterior pole to the equator were produced by overlapping the printed frames.
Follow-up was repeated at 3-month intervals until complete resolution of SRF was confirmed. On postoperative fundoscopy utilizing slit lamp examination with 90 diopter lens or contact lens, careful attention was paid to detect shallow concave SRF or an SRF bleb over the entire retina.
We defined delayed absorption as the presence of concave SRF or an SRF bleb at postoperative 6 months. Forms of SRF were described as shallow concave fluid under or around the fovea, focal accumulations of fluid as SRF blebs, or peripherally located, shallow concave fluid at the posterior margin of the buckling material. None of the eyes showed an increasing amount of SRF during postoperative observation, which may suggest the presence of an unsealed or new retinal break.
Choroidal features were evaluated in both eyes on ICGA including punctate hyperfluorescent spots, venous dilatation, early phase arterial filling defects, and CVH. CVH was defined as multifocal areas of hyperfluorescence with blurred margins within the choroid, according to a report by Guyer et al. [10]. Interpretation was performed by two independent ophthalmologists (GEC and EJL) who were masked to the other clinical data. In case of any discrepancy between the two readers, a senior grader (SWK) was asked to arbitrate.
Subfoveal choroidal thickness, as defined as the vertical distance between the Bruch's membrane and the innermost chorioscleral interface, was measured manually by a masked observer using the attached measuring software in the Heidelberg Spectralis OCT [1112]. Vertical and horizontal scans were conducted and the average value of the thickness was used for analysis.
Values are given as the frequency and percentage for qualitative parameters, while the mean and standard deviation are provided for quantitative parameters. Best-corrected visual acuity was converted to logarithm of the minimal angle of resolution units before analysis. The Mann-Whitney U-test was used for comparison of continuous data between the eyes with and without delayed absorption, and the Fisher exact test was used for categorical analysis. Unweighted Cohen kappa statistics were applied to test for interobserver reliability. All of the statistical analyses were performed using SPSS ver. 22.0 (IBM Corp., Armonk, NY, USA). A p-value less than 0.05 was considered statistically significant.
There were 50 consecutive patients during the study period. Among them, four patients with previous vitreoretinal surgery, six patients with recurrence of RRD, and two patients with follow-up loss were excluded. Two patients with subretinal fibrosis and demarcation line were also excluded because of long-standing RRD (duration between symptom onset to surgery was 3 months). Finally, a total of 36 eyes of 36 patients were analyzed in the present study.
The preoperative demographic and clinical characteristics of the enrolled patients are shown in Table 1. Macular involvement was found in 20 eyes, including 12 macula-off and eight macula-threatening cases. In the other 16 eyes, retinal detachments were peripherally located, not involving the posterior pole. Among 26 patients who had undergone scleral buckling and cryotherapy, external SRF drainage was performed in two patients. The number of patients lost during follow-up was five (13.8%), six (16.7%), four (11.1%), and three (8.3%) at 1 week, 1 month, 3 months, and 6 months after surgery, respectively.
Delayed absorption was present in 18 eyes (50%) at postoperative 6 months. Of the eyes with macula-off or threatening RRD, delayed absorption was found in 14 (70%): SRF bleb in seven, shallow concave SRF in five, and both in two. Among 16 eyes with peripheral RRD, delayed absorption was observed in four eyes (25.0%), manifesting as shallow concave SRF posterior to the elevated buckle. Demonstration of SRF with OCT, where the retina appeared flat on funduscopic examination, was noted in five cases.
Comparisons of demographic and clinical factors according to the presence or absence of delayed absorption of SRF are shown in Table 1. Preoperative macular status and best-corrected visual acuity were significantly related to delayed absorption (p = 0.001 and p = 0.034, respectively). Otherwise, no significant differences were found in clinical characteristics.
Choroidal vascular features were studied by ICGA in both affected eyes and fellow eyes before and after surgery. In preoperative ICGA, four affected eyes showed punctate hyperfluorescent spots; four showed venous dilation; and nine showed CVH. In fellow eyes, seven eyes showed punctate hyperfluorescent spots; four showed venous dilation; two showed early arterial filling defects; and four showed CVH.
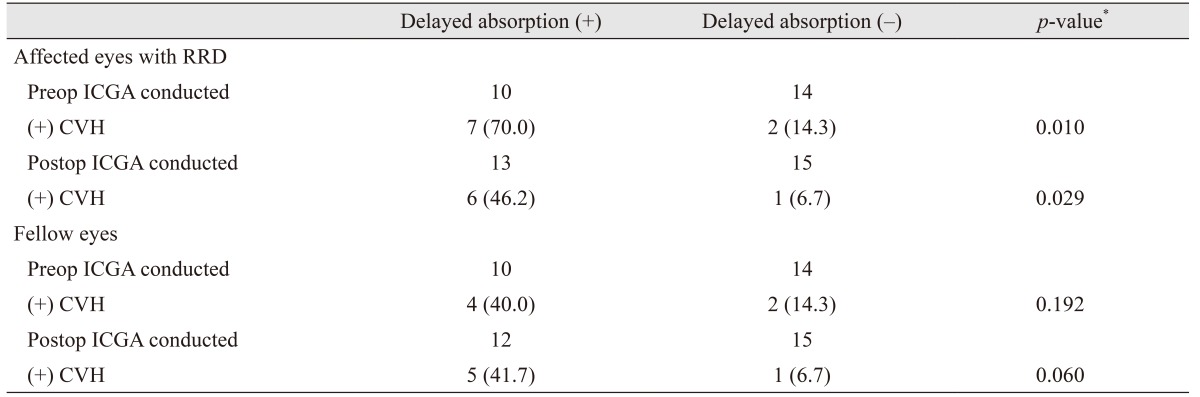
Among choroidal vascular features, preoperative CVH showed a significant relationship with delayed absorption (Table 2). Seventy percent of eyes with delayed absorption showed CVH, while only 14% of the eyes without delayed absorption showed CVH (p = 0.010). Postoperative CVH was detected in six (46.2%) of 13 eyes with delayed absorption, and only one of 15 eyes without delayed absorption exhibited CVH (p = 0.029). In fellow eyes, a similar tendency was observed but there was no statistical significance. There were no cases of postoperative CVH in the absence of preoperative CVH, and the presence of preoperative and postoperative CVH were correlated (p < 0.001). Kappa statistics showed good interobserver agreement for ICGA interpretation in CVH between two masked observers (Cohen's kappa, 0.765). The relationship between CVH and delayed absorption among the eyes, excluding those that underwent vitrectomy, are summarized in Table 3.
Preoperative subfoveal choroidal thickness tended to be higher in eyes with preoperative CVH than those without preoperative CVH; however, this was not statistically significant (p = 0.064). The same tendency was also observed in the analysis of fellow eyes (Table 4). Choroidal thickness significantly decreased at postoperative 3 months and 6 months in eyes with preoperative CVH (p = 0.036 and p = 0.011, respectively). However, choroidal thickness in eyes without preoperative CVH did not show such a tendency postoperatively.
Typical OCT and ICGA images of the eyes that underwent operation are shown in Fig. 1A, B1, C1, 1D, 2A, B2, C2, D2, E2, 2F
Complete retinal reattachment without any additional treatment was confirmed during follow-up in every case except 1, in which photodynamic therapy for persistent SRF under fovea was applied with achievement of complete resolution of SRF (Fig. 3A, B3, C3, 3D). In eyes with delayed absorption, the complete resolution of SRF was noted at 13.13 ± 4.30 months (6.3 to 20.0 months) postoperatively.
We have shown that delayed absorption of SRF after surgery for RRD is not rare, occurring in almost half of the cases in our cohort. Preoperative macular status was important for the prediction of delayed absorption, and choroidal features demonstrated a possible relationship. To the best of our knowledge, this is the first study to investigate the incidence of delayed absorption over a long-term period, as well as the relationship between choroidal features and the retinal reattachment process.
The high incidence of delayed absorption in this study could partly be explained by the high sensitivity of OCT in SRF detection. Shallow SRF with a height of less than 300 mm can easily go unnoticed on routine funduscopic examination. We carefully searched for any SRF and conducted detailed OCT scans on every patient. Although we identified a few patients with peripherally located SRF, it is possible the incidence is higher than reported because OCT scanning in the periphery is often challenging.
Twenty-six of 36 eyes had scleral buckling alone and only two had external drainage of SRF. At completion of surgery, the existence of submacular fluid was still noted in preoperative macula-off cases (nine eyes). One may speculate that this finding may also be due to the high percentage of eyes with retained SRF. However, because we can witness postoperative SRF blebs even in the preoperatively non-detached retina, the rare application of external SRF drainage does not adequately explain the high incidence of delayed absorption. Nevertheless, we speculate that adding external SRF drainage to scleral buckling can be beneficial in conditions where choroidal hyperpermeability and thickened choroid are observed before surgery, especially in macula-off RRD.
In previous studies, segmental scleral buckling surgery, preoperative macula-off RRD, and young age were reported as risk factors associated with delayed absorption of SRF [8131415]. The results of this study coincided with previous reports in that preoperative macula-off RRD and resultant worse preoperative vision were significant factors. There has been no concrete explanation for why macula-off status leads to delayed absorption of SRF. Different anatomic features, including choroidal blood supply to fovea, might play a role, but further studies are needed.
Choroidal vascular changes were not rare in this study. In addition to affected eyes with RRD, fellow eyes also showed abnormal features on ICGA. This could partly be due to ethnicity, as Asians have a predisposition for central serous chorioretinopathy and polypoidal choroidal vasculopathy [161718], which share a common pathological mechanism [1920]. Because preoperative and postoperative ICGA findings were correlated, we speculate that development of CVH was irrelevant to RRD or surgical manipulation. Patients may have had hyperpermeable choroids prior to the occurrence of RRD, which could explain the phenomenon of SRF blebs occurrence in areas outside the previously detached retina.
Mixed results regarding the influence of delayed absorption on final visual acuity outcome have been reported [3142122]. In this study, the resolution of SRF was confirmed in the majority of the cases in long-term follow-up, and we did not see a significant difference in final visual acuity according to the presence or absence of delayed absorption. Long-standing foveal detachment, albeit shallow, would have a deleterious effect on final visual acuity. Thus, we applied verteporfin photodynamic therapy to the area of CVH in a patient with foveal detachment persisting more than 1 year after reattachment surgery. The photodynamic therapy resulted in complete absorption of SRF and the result seems to indirectly support the role of CVH in the development of delayed absorption of SRF. The performance was logically based on demonstrated CVH, and this might serve as a beneficial treatment modality for future patients with long-standing delayed absorption involving the macula. Because additional treatments such as photodynamic therapy or laser treatment for persistent SRF have not been validated to date, further studies may be required.
Choroidal thickness is reported to be greater in eyes with CVH than eyes without CVH in polypoidal choroidal vasculopathy, as well as in areas with CVH, than areas without CVH in central serous chorioretinopathy [2324]. In this study, the choroid was marginally thicker in eyes with CVH than without CVH preoperatively. In eyes with CVH, choroidal thickness showed a tendency to decline over time. The reason for these temporal changes in subfoveal choroidal thickness remains unclear.
There are several limitations in this study. First, there was a relatively high ratio of protocol deviation and follow- up loss. Second, ICGA did not cover the 360° periphery of the retina, although we tried to include peripheral scans as much as possible. Also, ICGA images provided a limited analysis of the relationship between the extent and location of CVH. Irrespective of location, the presence of CVH would be represented in the characteristics of a patient's choroid and influence the delayed absorption of SRF after RRD surgery. Third, because peripheral OCT scans were challenging, there may have been limited detection of SRF on postoperative follow-ups. Nevertheless, in cases with preoperative CVH and no postoperative delayed absorption, half of the eyes were peripherally located RRDs. Therefore, our results could be strengthened if more peripheral OCT were possible. Fourth, the detection of CVH could be subjective, although the ICGA results of each patient were evaluated by two masked observers using the same criteria as in previous reports [102325]. Furthermore, in eyes with bullous RD, evaluation for CVH was more difficult than in fellow eyes. This may be a potential source of overestimation of CVH in RD.
In conclusion, with better detection using OCT, we found that the incidence of delayed absorption of SRF was quite high after surgeries for RRD. Macula-off status was significantly related to its incidence, and choroidal features, especially CVH, might be also associated with delayed absorption, possibly through the resultant exudative property of choroid.
References
1. Machemer R. Experimental retinal detachment in the owl monkey. IV. The reattached retina. Am J Ophthalmol. 1968; 66:1075–1091. PMID: 4973290.
2. Baba T, Hirose A, Moriyama M, Mochizuki M. Tomographic image and visual recovery of acute macula-off rhegmatogenous retinal detachment. Graefes Arch Clin Exp Ophthalmol. 2004; 242:576–581. PMID: 14997321.

3. Benson SE, Schlottmann PG, Bunce C, et al. Optical coherence tomography analysis of the macula after vitrectomy surgery for retinal detachment. Ophthalmology. 2006; 113:1179–1183. PMID: 16647127.

4. Hagimura N, Iida T, Suto K, Kishi S. Persistent foveal retinal detachment after successful rhegmatogenous retinal detachment surgery. Am J Ophthalmol. 2002; 133:516–520. PMID: 11931785.

5. Kaga T, Fonseca RA, Dantas MA, et al. Optical coherence tomography of bleb-like subretinal lesions after retinal reattachment surgery. Am J Ophthalmol. 2001; 132:120–121. PMID: 11438071.

6. Robertson DM. Delayed absorption of subretinal fluid after scleral buckling procedures: the significance of subretinal precipitates. Trans Am Ophthalmol Soc. 1978; 76:557–583. PMID: 754382.
7. Wolfensberger TJ, Gonvers M. Optical coherence tomography in the evaluation of incomplete visual acuity recovery after macula-off retinal detachments. Graefes Arch Clin Exp Ophthalmol. 2002; 240:85–89. PMID: 11931084.

8. Wolfensberger TJ. Foveal reattachment after macula-off retinal detachment occurs faster after vitrectomy than after buckle surgery. Ophthalmology. 2004; 111:1340–1343. PMID: 15234134.

9. Kang SW, Kim JH, Shin WJ, Kim JI. Subretinal fluid bleb after successful scleral buckling and cryotherapy for retinal detachment. Am J Ophthalmol. 2008; 146:205–210. PMID: 18514609.

10. Guyer DR, Yannuzzi LA, Slakter JS, et al. Digital indocyanine green videoangiography of central serous chorioretinopathy. Arch Ophthalmol. 1994; 112:1057–1062. PMID: 8053819.

11. Chung SE, Kang SW, Lee JH, Kim YT. Choroidal thickness in polypoidal choroidal vasculopathy and exudative age-related macular degeneration. Ophthalmology. 2011; 118:840–845. PMID: 21211846.

12. Jirarattanasopa P, Ooto S, Nakata I, et al. Choroidal thickness, vascular hyperpermeability, and complement factor H in age-related macular degeneration and polypoidal choroidal vasculopathy. Invest Ophthalmol Vis Sci. 2012; 53:3663–3672. PMID: 22570352.

13. Kim YK, Woo SJ, Kim KE, Park KH. Subretinal fluid resorption. Ophthalmology. 2010; 117:1655. 1655.e1. 1655.e4. PMID: 20682381.

14. Kim YK, Woo SJ, Park KH, et al. Comparison of persistent submacular fluid in vitrectomy and scleral buckle surgery for macula-involving retinal detachment. Am J Ophthalmol. 2010; 149:623–629.e1. PMID: 20149338.

15. Kim YK, Ahn J, Woo SJ, et al. Multiple subretinal fluid blebs after successful retinal detachment surgery: incidence, risk factors, and presumed pathophysiology. Am J Ophthalmol. 2014; 157:834–841. PMID: 24447856.

16. Imamura Y, Engelbert M, Iida T, et al. Polypoidal choroidal vasculopathy: a review. Surv Ophthalmol. 2010; 55:501–515. PMID: 20850857.

17. Maruko I, Iida T, Saito M, et al. Clinical characteristics of exudative age-related macular degeneration in Japanese patients. Am J Ophthalmol. 2007; 144:15–22. PMID: 17509509.

18. Tsai DC, Chen SJ, Huang CC, et al. Epidemiology of idiopathic central serous chorioretinopathy in Taiwan, 2001-2006: a population-based study. PLoS One. 2013; 8:e66858. PMID: 23826160.

19. Iida T, Kishi S, Hagimura N, Shimizu K. Persistent and bilateral choroidal vascular abnormalities in central serous chorioretinopathy. Retina. 1999; 19:508–512. PMID: 10606450.

20. Sasahara M, Tsujikawa A, Musashi K, et al. Polypoidal choroidal vasculopathy with choroidal vascular hyperpermeability. Am J Ophthalmol. 2006; 142:601–607. PMID: 17011852.

21. Benson SE, Schlottmann PG, Bunce C, et al. Optical coherence tomography analysis of the macula after scleral buckle surgery for retinal detachment. Ophthalmology. 2007; 114:108–112. PMID: 17095091.

22. Kim YK, Kim YW, Woo SJ, et al. Persistent submacular fluid and structural and functional recovery of retina. Ophthalmology. 2014; 121:2501–2502. PMID: 25085630.

23. Koizumi H, Yamagishi T, Yamazaki T, Kinoshita S. Relationship between clinical characteristics of polypoidal choroidal vasculopathy and choroidal vascular hyperpermeability. Am J Ophthalmol. 2013; 155:305–313.e1. PMID: 23022162.

24. Jirarattanasopa P, Ooto S, Tsujikawa A, et al. Assessment of macular choroidal thickness by optical coherence tomography and angiographic changes in central serous chorioretinopathy. Ophthalmology. 2012; 119:1666–1678. PMID: 22521082.

25. Tsujikawa A, Ojima Y, Yamashiro K, et al. Punctate hyperfluorescent spots associated with central serous chorioretinopathy as seen on indocyanine green angiography. Retina. 2010; 30:801–809. PMID: 20094008.

Fig. 1
A case with delayed absorption of subretinal fluid (case 9). (A) Preoperative infrared fundus photography and optical coherence tomography imaging. (B) Preoperative indocyanine green angiography shows choroidal vascular hyperpermeability (arrows) around the macula. (C) Postoperative indocyanine green angiography of the same patient shows areas of hyperfluorescence around subretinal fluid (arrows). (D) A concave subretinal fluid bleb, which progressively decreased in height.
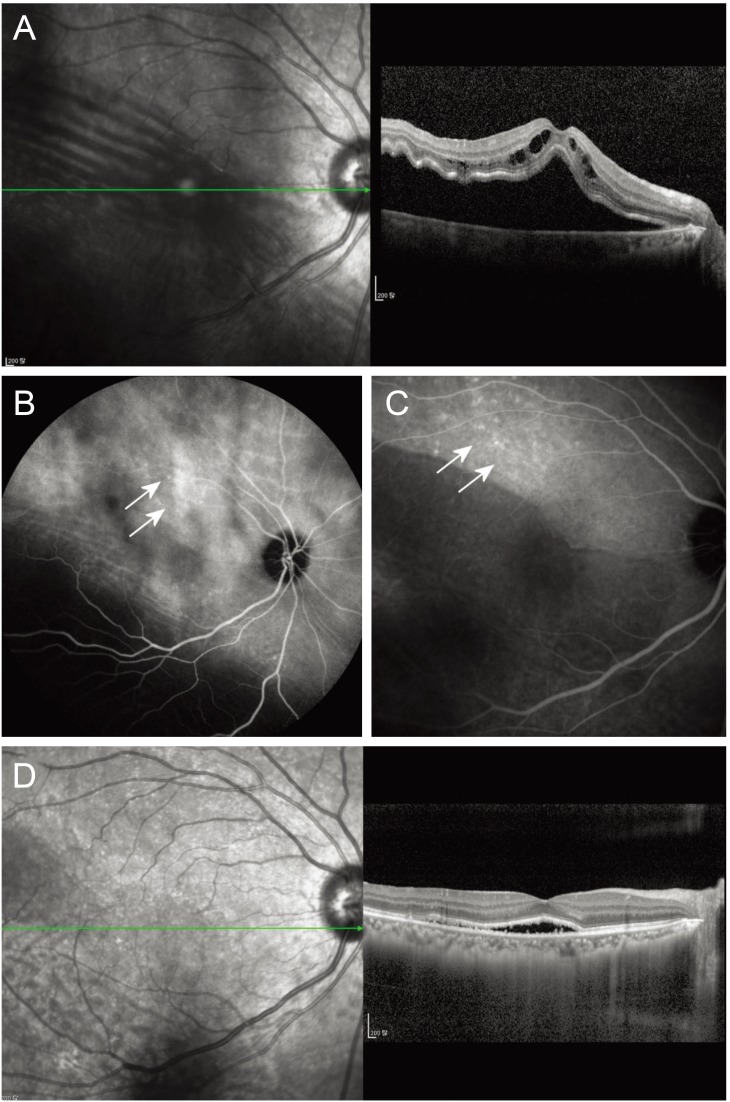
Fig. 2
A case with delayed absorption of subretinal fluid (case 16). (A) Preoperative infrared fundus photography and optical coherence tomography imaging. Preoperative indocyanine green angiography shows focal choroid vascular hyperpermeability (arrow) around the macula in the fellow eye (B) and in the affected eye with retinal detachment (C). (D) Postoperative 1-month indocyanine green angiography shows that preoperatively observed focal hyperfluorescence (arrow) remains in the fellow eye. (E) Patchy hyperfluorescence with choroidal vascular hyperpermeability are observed in the affected eye. (F) Concave subretinal fluid and a subretinal fluid bleb, which progressively decreased in height.
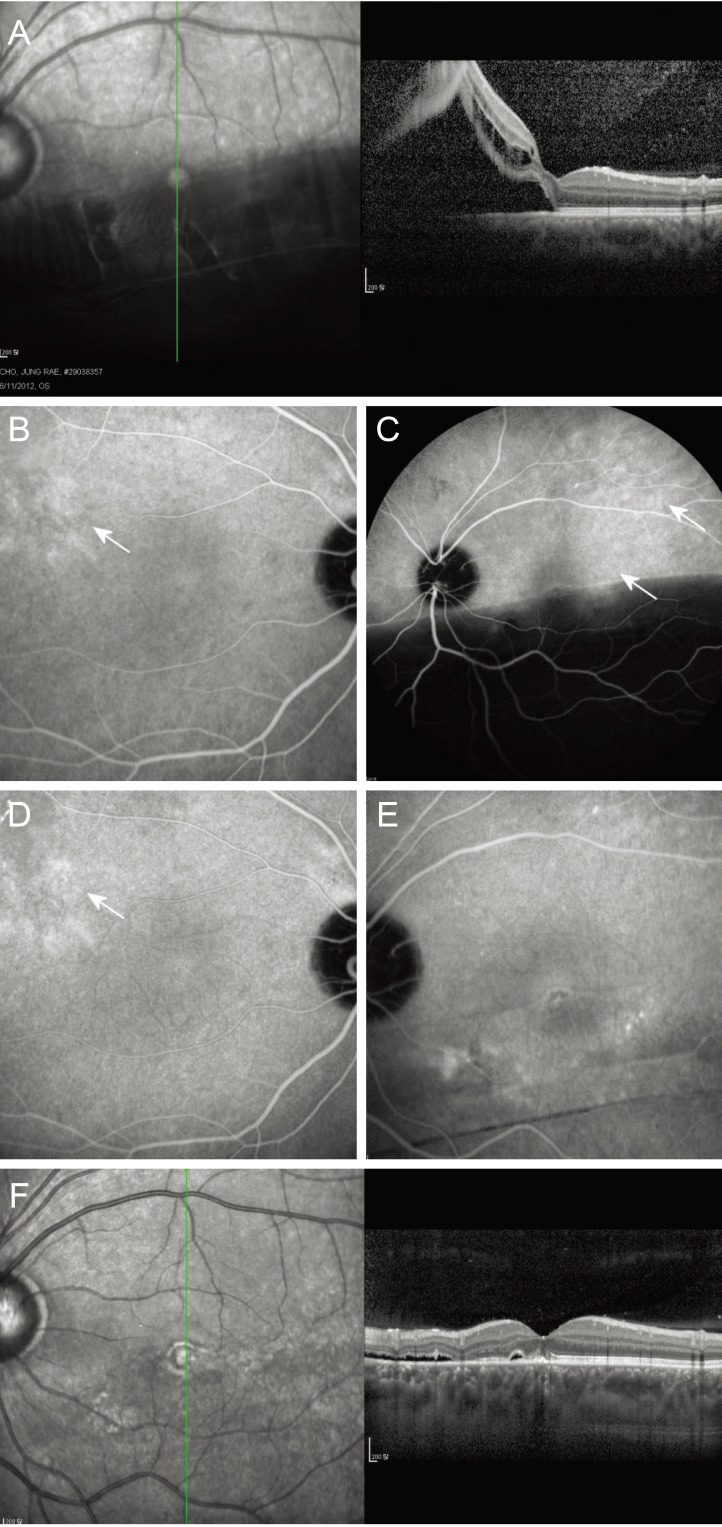
Fig. 3
Multimodal images of a case with persistent subretinal fluid (SRF) where postoperative photodynamic therapy resulted in complete resolution of SRF (case 36). (A) Preoperative infrared fundus photography and optical coherent tomography imaging show macula-off retinal detachment. (B) Indocyanine green angiography and optical coherent tomography taken 1 year postoperatively show concave SRF involving the fovea with thickened choroid. A mild degree of choroidal vascular hyperpermeability is noted from the temporal margin of the optic disk to the fovea. (C) A significant decrease in SRF was observed 3 months after photodynamic therapy. (D) Complete resolution of SRF was confirmed at 6 months after photodynamic therapy.
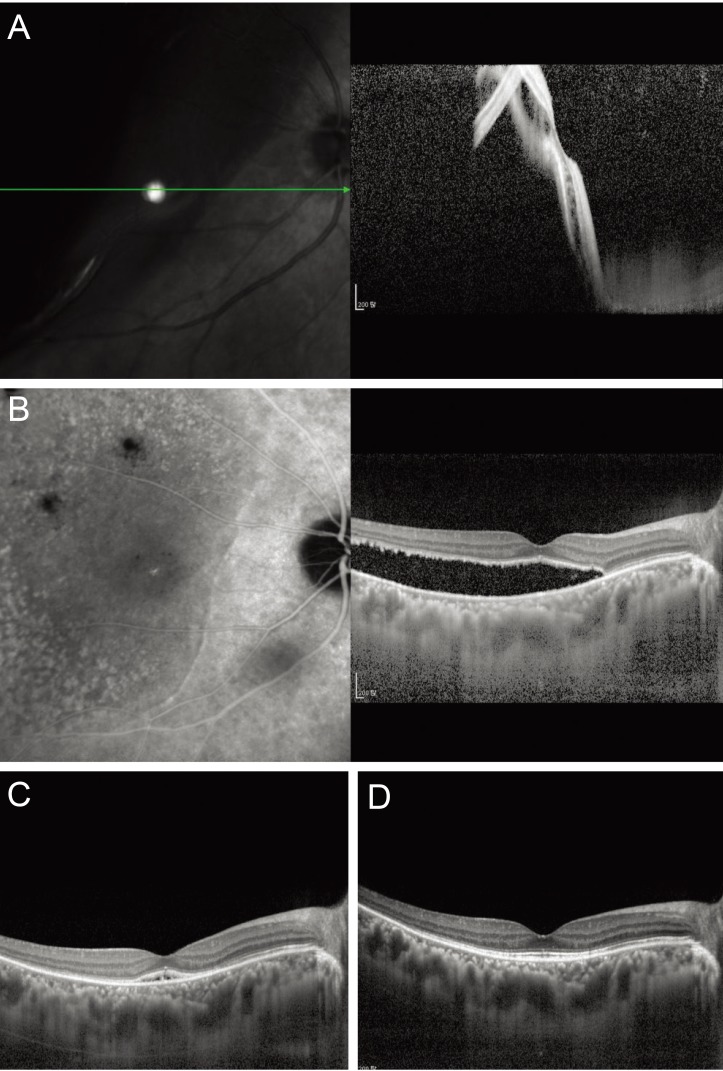
Table 1
Demographics and comparisons according to the presence of delayed absorption of subretinal fluid after surgery
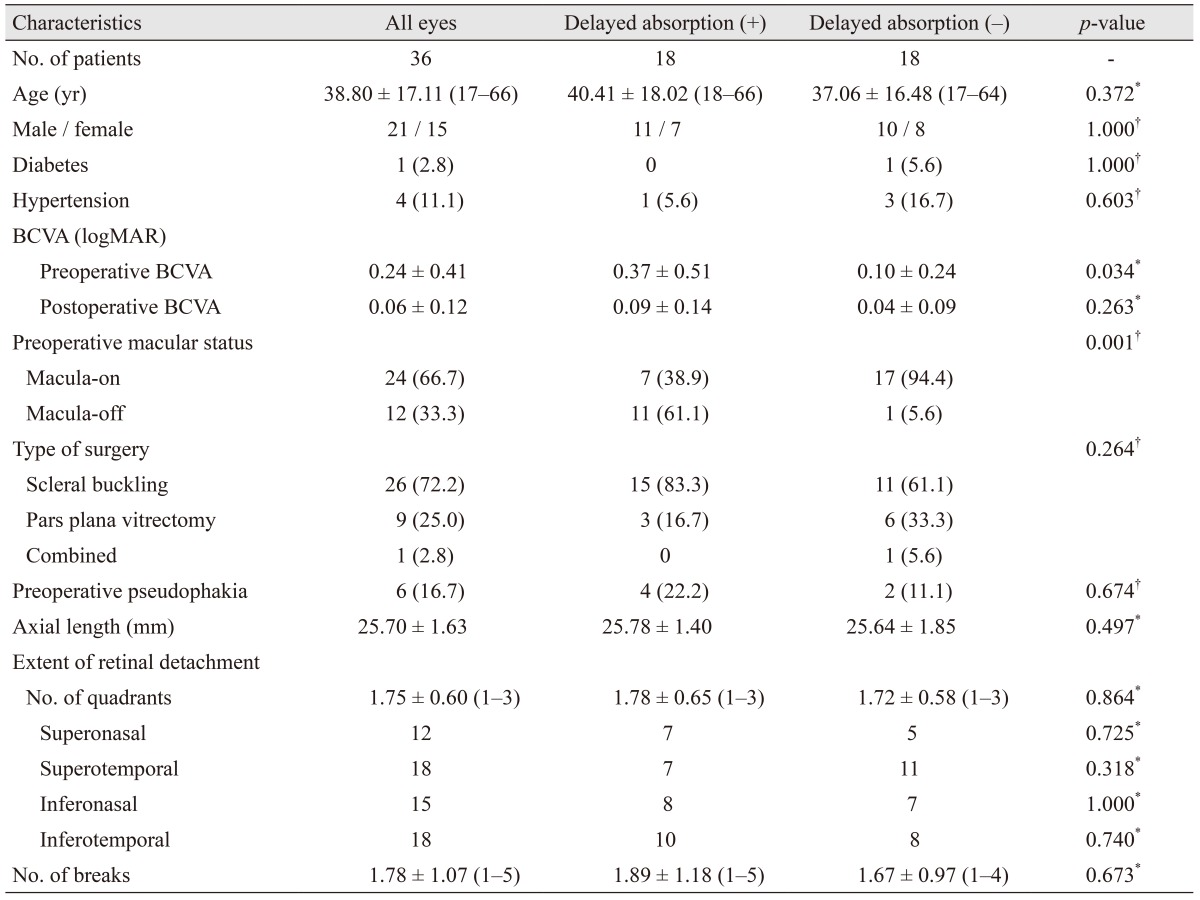
Table 3
Relationship of CVH and delayed absorption among eyes that underwent scleral buckling and cryotherapy
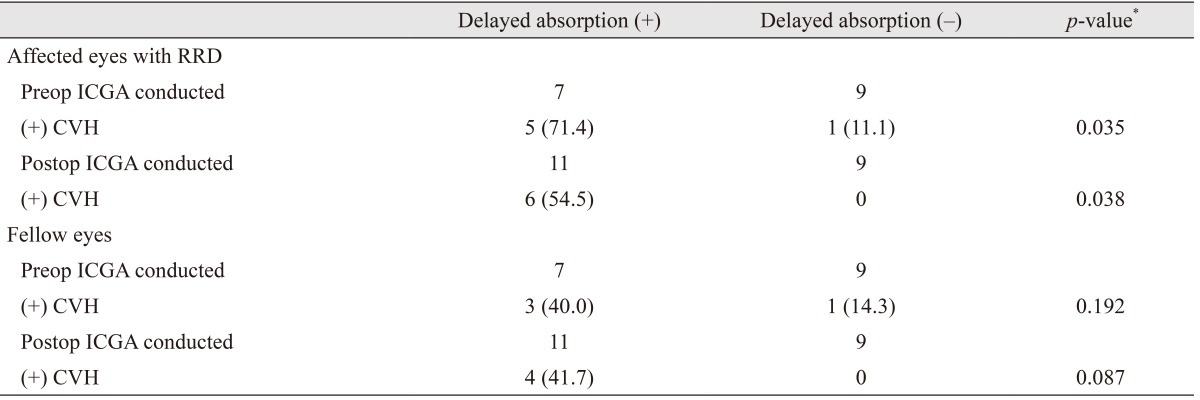
Table 4
Changes in subfoveal choroidal thickness before and after surgery for retinal detachment according to the presence of CVH
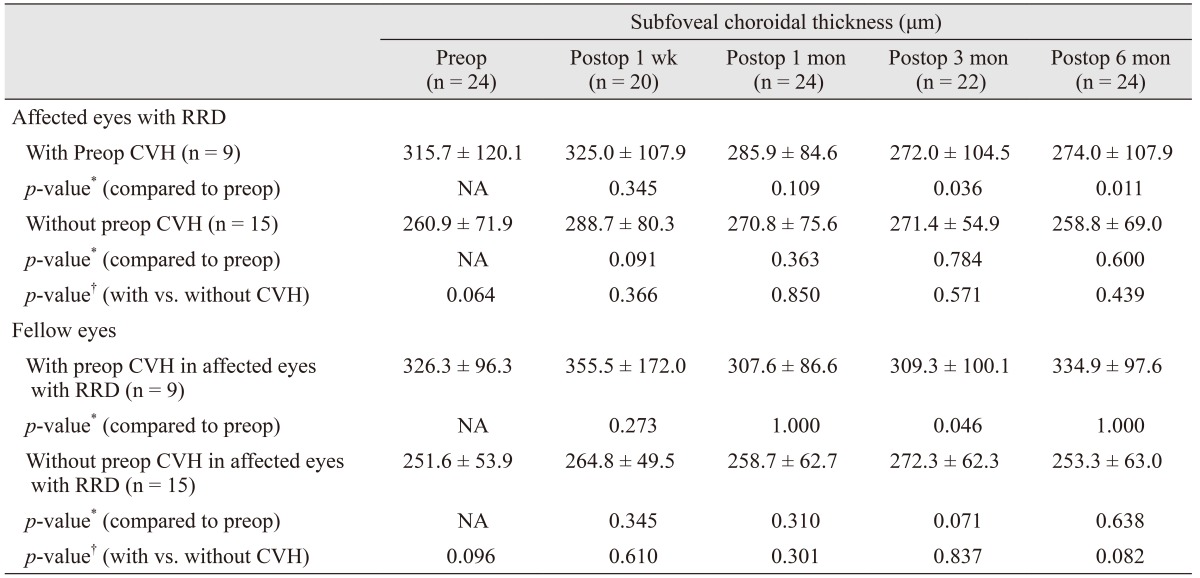
Values are presented as mean ± standard deviation.
CVH = choroidal vascular hyperpermeability; Preop = preoperative; Postop = postoperative; RRD = rhegmatogenous retinal detachment; NA = not available.
*A p-value was calculated by the Wilcoxon signed-rank test; †A p-value was calculated by the Mann-Whitney U-test.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download