Abstract
Purpose
To assess the effectiveness and safety of intravitreal ranibizumab compared with bevacizumab for the treatment of macular edema associated with branch retinal vein occlusion (BRVO).
Methods
This was a retrospective study of 80 eyes with macular edema associated with BRVO. Patients received either 0.5 mg of ranibizumab (n = 24) or 1.25 mg of bevacizumab (n = 56) intravitreally. Both groups received three initial monthly injections followed by as-needed injections. The best-corrected visual acuity, central subfield thickness, mean number of injections, and retreatment rate were evaluated monthly for 6 months after the initial injection.
Results
The best-corrected visual acuity significantly improved from logarithm of the minimal angle of resolution (logMAR) 0.55 ± 0.26 at baseline to 0.24 ± 0.26 at 6 months in the ranibizumab group (p < 0.001) and from logMAR 0.58 ± 0.21 at baseline to 0.29 ± 0.25 at 6 months in the bevacizumab group (p < 0.001), which is not a statistically significant difference (p = 0.770). The mean reduction in central subfield thickness at 6 months was 236 ± 164 µm in the ranibizumab group (p < 0.001) and 219 ± 161 µm in the bevacizumab group (p < 0.001), which is not also a statistically significant difference (p = 0.698). The mean numbers of ranibizumab and bevacizumab injections were 3.25 ± 0.53 and 3.30 ± 0.53, respectively (p = 0.602). In addition, after the three initial monthly injections, the retreatment rates for ranibizumab and bevacizumab injections were 20.8% and 26.7%, respectively (p = 0.573).
Branch retinal vein occlusion (BRVO) is one of the most common retinal vascular diseases after diabetic retinopathy [1]. The prevalence of BRVO is 4.42 per 1,000 [2]. BRVO is caused by focal occlusion of a retinal vein and typically occurs at an arteriovenous crossing, where, in most cases, the artery is passing superficially to the vein [3].
Macular edema is the main cause of visual impairment in BRVO [4]. The pathogenesis of macular edema associated with BRVO is not completely understood, but may result from a variety of factors, including hydrostatic effects from increased venous pressure, dysregulation of endothelial tight junctions, increases in the levels of inflammatory cytokines [5], and vascular permeability factors [6]. In more recent years, studies have demonstrated significantly elevated levels of vascular endothelial growth factor (VEGF) in eyes with BRVO and have found that it is a major contributor to macular edema. The severity of BRVO correlates with an increase in VEGF levels [7]. Given these findings, inhibiting VEGF seems to be a reasonable approach to treating macular edema associated with BRVO.
Ranibizumab (Lucentis; Genentech, South San Francisco, CA, USA), a Fab fragment that binds all isoforms of VEGF-A, has been shown to markedly reduce macular edema associated with BRVO. A large study, “Ranibizumab for the Treatment of Macular Edema following Branch Retinal Vein Occlusion: Evaluation of Efficacy and Safety (BRAVO),” demonstrated that intravitreal injections of ranibizumab resulted in significant functional and anatomical improvements in patients with BRVO over the course of 6 months [8].
Bevacizumab (Avastin, Genentech; Roche, Basil, Switzerland) is a full-length, humanized, recombinant antibody that binds all isoforms of VEGF-A and has been used extensively off-label to treat macular edema associated with BRVO. Several studies have shown that intravitreal bevacizumab injection improves visual acuity and reduces macular thickness in macular edema associated with BRVO [910].
In addition, a recently published study that compared the effects of ranibizumab and bevacizumab followed by monthly pro-re-nata for the treatment of macular edema associated with BRVO showed that there were no significant differences in the improvement of mean visual acuity, mean change in macular thickness, or total number of injections between the two treatments [11].
To the best of our knowledge, however, there is no published study comparing the effects and retreatment rates between ranibizumab and bevacizumab after three initial monthly loading doses for macular edema associated with BRVO. In this paper, we conducted a retrospective study comparing the changes in best-corrected visual acuity (BCVA), central subfield thickness (CST), mean number of injections, and retreatment rate between ranibizumab and bevacizumab in macular edema associated with BRVO over a period of 6 months.
We conducted a retrospective study of patients with macular edema associated with BRVO treated with intravitreal bevacizumab or ranibizumab injection at the Kyung Hee University Medical Center between October 2008 and December 2014. Approval for this retrospective review was obtained from the institutional review board of our institution.
Patients were included in the study if they met the following inclusion criteria: (1) foveal center-involved macular edema associated with BRVO of less than 9 months duration; (2) CST greater than 250 µm on spectral domain optical coherence tomography (SD-OCT); and (3) BCVA between 0.3 logarithm of the minimal angle of resolution (logMAR) and 1.2 logMAR. Exclusion criteria were: (1) administration of any other intravitreal drug during the study period; (2) prior anti-VEGF treatment or intraocular corticosteroid use in the study eye within 3 months; (3) a history of intraocular surgery in the study eye; (4) panretinal laser photocoagulation or macular laser photocoagulation in the study eye; and (5) presence of any other macular pathology, such as age-related macular degeneration or diabetic retinopathy affecting the macula.
A total of 80 eyes in 80 patients were included; they were divided into two groups, eyes that received ranibizumab for the treatment of macular edema (n = 24), and those that received bevacizumab (n = 56). In the ranibizumab group, patients were treated with intravitreal ranibizumab injection three times at 4-week intervals, whereas in the bevacizumab group, patients were treated with intravitreal bevacizumab injection three times at 6-week intervals. During the follow-up period, patients received additional injections when an increase in CST of at least 100 µm on OCT or a reduction of logMAR score of at least 0.2 occurred. Patients were followed up for a period of 6 months.
All patients received a complete ocular examination, including BCVA testing, CST measurements by SD-OCT (Zeiss Cirrus, Dublin, CA, USA), dilated fundus examination with slit lamp biomicroscopy, color fundus photography, and fluorescein angiography at baseline. BCVA was measured with a standard Snellen chart at 6 m and converted to logMAR visual acuity for statistical analysis.
Intravitreal ranibizumab and bevacizumab injections were performed in the operating room under sterile conditions. Topical anesthetic drops were given first and then a lid speculum was inserted. After the injection site was cleaned with 5% povidone iodine, 0.5 mg (0.05 mL) ranibizumab or 1.25 mg (0.05 mL) bevacizumab was applied via the pars plana with a 30-gauge needle. The needle was carefully removed using a sterile cotton applicator to prevent reflux. Indirect ophthalmoscopy and tonometry were performed after the procedure to detect any injection-related complications. After the injection, antibiotic eye drops were applied every 6 hours for 1 week.
The primary outcomes included the mean change from baseline of logMAR BCVA, the mean change from baseline of CST as assessed by SD-OCT, the mean number of injections, and the retreatment rate over the 6 months following the initial injection. A follow-up examination was performed every month after the three initial intravitreal injections. BCVA, fundus exam, tonometry, and CST measured with OCT were assessed at each follow-up visit. The secondary outcome measure was the incidence of ocular adverse events.
Statistical analyses were performed using SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). The Wilcoxon signed-rank test was used for statistical analysis of changes in visual acuity and CST. The Mann-Whitney U-test was used where appropriate to compare baseline characteristics, changes in visual acuity and CST, and the mean number of injections between the treatment groups. The chi-square test was used to compare the retreatment rates. A Fisher's exact test was used to compare the incidence of ocular adverse events. For all statistical tests, a p-value of less than 0.05 was considered to be statistically significant.
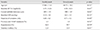
Between October 2008 and December 2014, 80 patients were included in the study and followed from baseline to 6 months. Twenty-four patients received intravitreal injections of 0.5 mg ranibizumab and 56 patients received 1.25 mg bevacizumab. There were no significant differences in the demographics or ocular characteristics of the study groups at baseline (Table 1). The average ages of the patients were 57.04 ± 11.6 and 60.73 ± 10.2 years in the ranibizumab and bevacizumab groups, respectively. The mean duration of symptoms was 4.68 ± 4.1 and 4.71 ± 5.1 weeks in the ranibizumab and bevacizumab groups, respectively. The mean visual acuities at baseline were logMAR 0.55 ± 0.26 and 0.58 ± 0.21 in the ranibizumab and the bevacizumab groups, respectively. The mean CST values at baseline were 489.0 ± 151.1 and 508.4 ± 145.6 µm in the ranibizumab and bevacizumab groups, respectively.
At 6 months, the mean BCVA significantly improved by logMAR 0.30 ± 0.17 (from logMAR 0.55 ± 0.26 to 0.24 ± 0.26) in the ranibizumab group and by logMAR 0.28 ± 0.26 (from logMAR 0.58 ± 0.21 to 0.29 ± 0.25) in the bevacizumab group (p < 0.001 and p < 0.001, respectively) (Fig. 1). There was no significant difference in the change in BCVA between the ranibizumab group and the bevacizumab group (p = 0.770) (Table 2).
The reduction in CST at 6 months was −236.7 ± 164.9 µm (from 489.0 to 252.2 µm) in the ranibizumab group and −219.0 ± 161.7 µm (from 508.4 to 289.4 µm) in the bevacizumab group (p < 0.001 and p < 0.001, respectively) (Fig. 2). There was no significant difference between the ranibizumab group and bevacizumab group in the reduction in CST (p = 0.698) (Table 3).
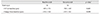
The mean number of injections administered during the 6-month treatment period was 3.25 ± 0.53 in the ranibizumab group and 3.30 ± 0.53 in the bevacizumab group. There was no significant difference between the ranibizumab group and bevacizumab groups in the mean number of injections (p = 0.602) (Table 4 and Fig. 3).
The retreatment rates in the ranibizumab and bevacizumab groups after the initial three injections were 20.8% and 26.7%, respectively. There was no significant difference in retreatment rate between the ranibizumab group and the bevacizumab group (p = 0.573) (Table 5).
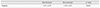
Ocular adverse events included the development of a vitreous hemorrhage in one patient (in the bevacizumab group) and increased intraocular pressure in three patients (one eye in the ranibizumab group and two eyes in the bevacizumab group) that was controlled with a topical medication. There was no significant difference in adverse events between the ranibizumab and bevacizumab groups. None of the patients in the study developed endophthalmitis, retinal detachment or tears, or injection-related cataracts (Table 6).
BRVO is caused by a blockage of the branch of the central retinal vein that carries blood away from the retina [3]. Macular edema is the most common complication of BRVO, and is the most serious in terms of causing vision loss [4]. Several treatments have already been proposed for the treatment of macular edema associated with BRVO. In the past, the Branch Vein Occlusion Study demonstrated that grid laser photocoagulation improved visual acuity in BRVO [12]. Since then, intravitreal injections have been proposed to reduce macular edema. Intravitreal triamcinolone acetonide and a dexamethasone implant (Ozurdex; Allergan, Irvine, CA, USA) improved visual acuity and reduced macular thickness in patients with macular edema associated with BRVO, but elevated intraocular pressure and cataracts occurred in the treatment group [1314].
In more recent years, studies have implicated VEGF in the development of macular edema in BRVO. Intraocular VEGF levels are well correlated with the severity of macular edema [7]. Furthermore, several studies have shown that intravitreal injections of the anti-VEGF agents ranibizumab and bevacizumab are effective in reducing macular edema associated with BRVO. The BRAVO trial assessed the efficacy of ranibizumab in patients with BRVO and found a significant improvement in visual acuity and a reduction in central foveal thickness in the ranibizumab-treated group compared to a sham group [8]. Yilmaz and Cordero-Coma [9] and Ehlers et al. [10] showed that bevacizumab brought about significant improvements in visual acuity and a reduction in CST in patients with BRVO.
Recently, the Macular Edema due to Branch Retinal Vein Occlusion (MARVEL) study attempted to compare the effects of ranibizumab and bevacizumab followed by monthly pro-re-nata injections for the treatment of macular edema associated with BRVO over the course of 6 months. At 6 months, the mean gains in BCVA were 18.1 letters in the ranibizumab group and 15.6 letters in the bevacizumab group (p = 0.48). The reduction in central retinal thickness was 177.1 µm in the ranibizumab group and 201.68 µm in the bevacizumab group (p = 0.30). Additionally, the mean numbers of ranibizumab and bevacizumab injections were 3.2 ± 1.5 and 3.0 ± 1.4, respectively (p = 0.55). Therefore, the MARVEL study showed that there was no significant difference between ranibizumab and bevacizumab in the improvement in mean visual acuity, mean change in macular thickness, or total number of injections [11].
In our study, we also compared the short-term effects of ranibizumab and bevacizumab for macular edema associated with BRVO. However, there is a key difference between the present study and prior BRVO trials: our patients received a loading dose of three monthly anti-VEGF injections, followed by an as-needed dosing schedule, while patients in the MARVEL study received anti-VEGF as monthly pro-re-nata injections from baseline. Despite the remarkable efficacy of anti-VEGF agents for BRVO, there is still no consensus on how they are used most effectively. Based on studies showing that a 3-month anti-VEGF dosing protocol is effective for the treatment of BRVO, the current study used three monthly anti-VEGF injections as the initial regimen, followed by as-needed injections [1516]. This protocol also allowed us to compare the retreatment rate between the two groups.
We found that both ranibizumab and bevacizumab led to similar functional and anatomical visual improvements. At 6 months, the mean increase in BCVA was 0.30 logMAR in the ranibizumab group and 0.28 logMAR in the bevacizumab group. CST also improved similarly in both groups. At 6 months, the mean reduction in CST was 236.7 µm in the ranibizumab group and 219.0 µm in the bevacizumab group. The mean number of injections and the retreatment rates were not also significantly different between the two groups. The mean numbers of injections administered during the 6-month period were 3.25 ± 0.53 and 3.30 ± 0.53 in the ranibizumab and bevacizumab groups, respectively. The retreatment rates after the three initial monthly injections were 20.8% and 26.7% in the ranibizumab and bevacizumab groups, respectively.
Both ranibizumab and bevacizumab are humanized monoclonal anti-VEGF antibodies; however, there are some differences in the molecular weight and structure between the two agents. Ranibizumab consists of a 49-kD Fab fragment, whereas bevacizumab is a 149-kD full-length antibody [1718]. Their differences influence their retinal penetration, half-life, and efficacy. Ranibizumab may have a greater ability to penetrate than bevacizumab does because of its smaller molecular size [1920]. Ranibizumab is also known to more potently neutralize VEGF than bevacizumab does in vitro [2122]. However, the larger size of bevacizumab may result in a longer duration of action because of its longer half-life [1718]. In our study, the two agents showed equivalent effects in the treatment of BRVO. Moreover, in another clinical study that compared the effects of ranibizumab and bevacizumab in cases of exudative AMD, the two agents had similar treatment effectiveness [2324]. These results suggest that when ranibizumab and bevacizumab are placed into the human eye, the biological effects of the two agents are more or less equivalent. Therefore, a study on the precise biological effects of anti-VEGF agents in the human eye should be carried out.
In our retrospective study comparing the short-term safety of bevacizumab and ranibizumab for macular edema associated with BRVO, there was no significant difference in the incidence of ocular adverse events. In the BRAVO study, ranibizumab was not associated with a significantly increased incidence of serious ocular adverse event, such as endophthalmitis, uveitis, retinal/choroidal detachment, retinal tear, vitreous hemorrhage, or ocular vessel embolism [8]. The same was true for a study on bevacizumab treatment for BRVO [910].
There are some limitations to this study, including its retrospective design, relatively small sample size, short follow-up time, the elimination of patients who were given fewer than three injections because they responded well to just one or two, its single-center design, and the lack of data on systemic adverse events.
In conclusion, our study showed that both ranibizumab and bevacizumab are effective for the treatment of macular edema associated with BRVO, and both result in relatively equal anatomical and functional improvements. In addition, the mean number of injections and the retreatment rate were not significantly different between the groups. Additional studies comparing anti-VEGF agents in the treatment of BRVO are necessary, including studies that compare the long-term efficacy and safety of different drugs. Also, the effects of different injection protocols should be investigated. Therefore, further research is needed to validate our findings, to provide long-term data, and to conduct comparisons in a prospective, randomized manner.
Figures and Tables
Fig. 1
Change in best-corrected visual acuity (BCVA). Mean logarithm of the minimal angle of resolution (logMAR, visual acuity) significantly improved after treatment with ranibizumab or bevacizumab from baseline to 6 months (*significantly different from baseline, p < 0.05). IVL = ranibizumab; IVA = bevacizumab.

Fig. 2
Change in central subfield thickness. Mean central subfield thickness significantly decreased after treatment with ranibizumab or bevacizumab from baseline to 6 months (*significantly different from baseline, p < 0.05). IVL = ranibizumab; IVA = bevacizumab.
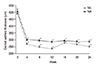
Fig. 3
Number of injections. In the ranibizumab group, 19 (79%) patients had three injections, four (17%) had four injections, and 1 (4%) received five injections. In the bevacizumab group, 41 (73%) patients had three injections, 13 (23%) had four injections, and two (4%) received five injections. IVL = ranibizumab; IVA = bevacizumab.

References
1. Klein R, Moss SE, Meuer SM, Klein BE. The 15-year cumulative incidence of retinal vein occlusion: the Beaver Dam Eye Study. Arch Ophthalmol. 2008; 126:513–518.
2. Rogers S, McIntosh RL, Cheung N, et al. The prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia, and Australia. Ophthalmology. 2010; 117:313–319.e1.
3. Christoffersen NL, Larsen M. Pathophysiology and hemodynamics of branch retinal vein occlusion. Ophthalmology. 1999; 106:2054–2062.
4. Rehak J, Rehak M. Branch retinal vein occlusion: pathogenesis, visual prognosis, and treatment modalities. Curr Eye Res. 2008; 33:111–131.
5. Antonetti DA, Barber AJ, Khin S, et al. Vascular permeability in experimental diabetes is associated with reduced endothelial occludin content: vascular endothelial growth factor decreases occludin in retinal endothelial cells: Penn State Retina Research Group. Diabetes. 1998; 47:1953–1959.
6. Campochiaro PA, Hafiz G, Shah SM, et al. Ranibizumab for macular edema due to retinal vein occlusions: implication of VEGF as a critical stimulator. Mol Ther. 2008; 16:791–799.
7. Noma H, Funatsu H, Yamasaki M, et al. Aqueous humour levels of cytokines are correlated to vitreous levels and severity of macular oedema in branch retinal vein occlusion. Eye (Lond). 2008; 22:42–48.
8. Campochiaro PA, Heier JS, Feiner L, et al. Ranibizumab for macular edema following branch retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010; 117:1102–1112.e1.
9. Yilmaz T, Cordero-Coma M. Use of bevacizumab for macular edema secondary to branch retinal vein occlusion: a systematic review. Graefes Arch Clin Exp Ophthalmol. 2012; 250:787–793.
10. Ehlers JP, Decroos FC, Fekrat S. Intravitreal bevacizumab for macular edema secondary to branch retinal vein occlusion. Retina. 2011; 31:1856–1862.
11. Narayanan R, Panchal B, Das T, et al. A randomised, double-masked, controlled study of the efficacy and safety of intravitreal bevacizumab versus ranibizumab in the treatment of macular oedema due to branch retinal vein occlusion: MARVEL report no. 1. Br J Ophthalmol. 2015; 99:954–959.
12. Argon laser photocoagulation for macular edema in branch vein occlusion: the Branch Vein Occlusion Study Group. Am J Ophthalmol. 1984; 98:271–282.
13. Scott IU, Ip MS, VanVeldhuisen PC, et al. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with standard care to treat vision loss associated with macular Edema secondary to branch retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 6. Arch Ophthalmol. 2009; 127:1115–1128.
14. Haller JA, Bandello F, Belfort R Jr, et al. Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010; 117:1134–1146.e3.
15. Kim M, Yu SY, Kim ES, et al. Intravitreal ranibizumab for macular edema secondary to retinal vein occlusion. Ophthalmologica. 2012; 227:132–138.
16. Siegel RA, Dreznik A, Mimouni K, et al. Intravitreal bevacizumab treatment for macular edema due to branch retinal vein occlusion in a clinical setting. Curr Eye Res. 2012; 37:823–829.
17. Bakri SJ, Snyder MR, Reid JM, et al. Pharmacokinetics of intravitreal ranibizumab (Lucentis). Ophthalmology. 2007; 114:2179–2182.
18. Bakri SJ, Snyder MR, Reid JM, et al. Pharmacokinetics of intravitreal bevacizumab (Avastin). Ophthalmology. 2007; 114:855–859.
19. Mordenti J, Cuthbertson RA, Ferrara N, et al. Comparisons of the intraocular tissue distribution, pharmacokinetics, and safety of 125I-labeled full-length and Fab antibodies in rhesus monkeys following intravitreal administration. Toxicol Pathol. 1999; 27:536–544.
20. Terasaki H, Sakamoto T, Shirasawa M, et al. Penetration of bevacizumab and ranibizumab through retinal pigment epithelial layer in vitro. Retina. 2015; 35:1007–1015.
21. Papadopoulos N, Martin J, Ruan Q, et al. Binding and neutralization of vascular endothelial growth factor (VEGF) and related ligands by VEGF trap, ranibizumab and bevacizumab. Angiogenesis. 2012; 15:171–185.
22. Yu L, Liang XH, Ferrara N. Comparing protein VEGF inhibitors: in vitro biological studies. Biochem Biophys Res Commun. 2011; 408:276–281.
23. Berg K, Pedersen TR, Sandvik L, Bragadottir R. Comparison of ranibizumab and bevacizumab for neovascular age-related macular degeneration according to LUCAS treat-and-extend protocol. Ophthalmology. 2015; 122:146–152.
24. CATT Research Group. Martin DF, Maguire MG, et al. Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med. 2011; 364:1897–1908.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download