Abstract
Purpose
To compare the clinical effects of the single wide-diameter bicanalicular silicone tube and the double bicanalicular silicone tube in endonasal dacryocystorhinostomy (DCR) with canalicular trephinization for canalicular obstruction.
Methods
We retrospectively reviewed the records of 121 patients with monocanalicular or common canalicular obstruction who had undergone endonasal DCR with random bicanalicular insertion of either double silicone tubes (insertion of two tubes into each canaliculus) or a single wide-diameter (0.94 mm) silicone tube. The tubes were removed at around 3 months after surgery.
Results
This study included 79 eyes of 61 patients in the double-tube intubation group and 68 eyes of 60 patients in the single wide-diameter tube intubation group. Anatomical success, evaluated by syringing, was achieved in 72 of the 79 eyes (91.1%) in the double-tube intubation group and 60 of the 68 eyes (88.2%) in the single wide-diameter tube intubation group. Functional success was achieved in 65 of the 79 eyes (82.3%) in the double-tube intubation group and 61 of the 68 (89.7%) eyes in the single wide-diameter tube intubation group. There were no significant differences in the success rates of surgery between the two groups. One patient in the double-tube intubation group underwent conjunctivodacryocystorhinostomy (CDCR) and two in the wide-diameter tube intubation group underwent CDCR or reintubation to treat recurrence.
The management of monocanalicular or common canalicular obstruction is challenging because of restenosis or sticky adhesive changes often observed during follow-up. Management strategies for canalicular obstruction include external or endonasal dacryocystorhinostomy (DCR), balloon catheter dilation, conjunctivodacryocystorhinostomy (CDCR) using a Jones tube, and insertion of bicanalicular silicone tubes. Although CDCR with Jones tube intubation is a widely-used standard procedure performed for the treatment of canalicular obstruction, the procedure may be complicated by nasal bleeding, infection, dislocation of the tube, and the need for permanent retention of the tube [1].
Many surgical techniques and instruments for stent placement have been described. The material of choice for stenting in the lacrimal system is silicone, which is generally inert within the system. Stents implanted within the nasolacrimal system prevent adherence of the mucosal lining of the ducts during healing and maintain long-term patency after removal. It has been shown that the greater is the diameter of the stent, the greater is the separation between the walls of the channel [2]. Silicone intubation methods such as the Crawford bicanalicular intubation method, Quickert-Dryden method, or silicone intubation using a Nunchaku-style tube have been introduced [345]. Bicanalicular silicone tube placement aims to maintain the anastomotic patency and stability of the epithelium of the canaliculus. However, many studies have reported that the long-term efficacy of silicone intubation for the treatment of stenotic or obstructed canaliculi is not high, especially in adults [6789]. In order to improve the success rates of silicone intubation in adults with canalicular obstruction, Demirci and Elner [6], Hwang et al. [7], and Kim and Kim [9] performed double silicone intubation and reported high final rates of success in long-term follow-up. They concluded that double silicone intubation is an effective minimally invasive technique for the treatment of partial obstruction of the lacrimal apparatus. In addition, Hurwitz [2] introduced single wide-diameter (0.94 mm) silicone intubation to treat canalicular obstruction. The procedure is inexpensive and relatively nontraumatic, as verified by Yildiz et al. [10], who reported no complications associated with the larger tube size.
In this study, we compared the clinical efficacies of double and single wide-diameter (0.94 mm) silicone tube intubations in the treatment of monocanalicular or common canalicular obstruction.
We retrospectively reviewed the medical records of 147 eyes of 121 patients (including 26 patients who had surgery on both eyes) who underwent either double or single wide-diameter (0.94 mm) silicone tube intubation for monocanalicular or common canalicular obstruction between January 2010 and December 2013. Approval from the institutional review board/ethics committee was obtained before starting the study. This study adhered to the tenets of the Declaration of Helsinki.
Each of the intubations was performed using either two 0.64-mm (outer diameter) silicone tubes (You-Won Meditec, Seoul, Korea) or one 0.94-mm (outer diameter) silicone tube (You-Won Meditec).
All of the patients were recruited from the outpatient clinic at Kim's Eye Hospital and were subjected to a thorough examination of the eyelid and lacrimal system, including examination of the puncta, conventional probing, syringing, and dacryocystography (DCG) with contrast. The diagnosis of canalicular obstruction and determination of the level of obstruction were based on the findings of lacrimal irrigation and probing. The patients included in this study exhibited complete canalicular obstruction, which was determined by the inability of the probe to pass beyond a soft stop as well as the inability to irrigate, which was confirmed by DCG. All of the patients were diagnosed as having monocanalicular or common canalicular obstruction. The level of canalicular obstruction was estimated in millimeters from the puncta to the end of the probe where the blockage was located. Distal canalicular obstruction was defined when the site of the obstruction was a distance ≥8 mm from the punctum. Common canalicular obstruction was confirmed by upper and lower canalicular syringing and probing. Patients with symptoms of dry eye caused by previous trauma or mass were excluded from this study. Patients who followed up for a period of less than 2 months were also excluded.
Endonasal DCR was performed under general anesthesia. Vasoconstriction of the nasal mucosa was achieved by packing gauze soaked in lidocaine mixed with a 1 : 100,000 dilution of epinephrine.
Conventional endonasal DCR with canalicular trephinization was performed once satisfactory anesthesia and nasal decongestion were achieved. Punctum dilatation was performed using a punctum dilator. A probe was inserted through the upper and lower puncta against the membrane obstructing the canaliculus. Then, a lubricated canalicular trephine with a stylet was inserted into the point of obstruction, where the stylet was removed, and the obstructed canaliculus was trephined by advancing the cutting part. Following this, the probe was reinserted to ensure that the obstruction was resolved. A 20-gauge endoilluminator probe, which allowed endonasal visualization of the location of the lacrimal sac by transillumination, was introduced through the canaliculus and advanced into the lacrimal sac. The nasal mucosa was dissected and cauterized by electrocautery, and a bony opening was created using a Kerrison punch, curette, or drill. The lacrimal sac was tented with a probe, incised using a sickle knife to create a posterior lacrimal sac, and removed using ethmoid forceps with or without diode laser. Two types of silicone tubes—0.64-mm-diameter and 0.94-mm-diameter silicone tubes (You-Won Meditec)—were used. The patients were separated into two groups, one treated with double silicone intubation and the other with single 0.94-mm silicone intubation. In the double-tube intubation group, the original silicone tube was passed through both canaliculi and retrieved through the new opening. Subsequently, a second silicone tube of the same size was inserted in an identical way. During this procedure, additional dilatation of the puncta was performed using a trephine in cases of persistent stenosis. The ends of the silicone tubes were tied off using square knots, and, after the excess tube was cut, the remaining part was left behind for retraction. The knots were tied such that they would not be retracted up to the rhinostomy site or protrude from the nostril. In the single wide-diameter tube intubation group, one large silicone tube was passed through both canaliculi and retrieved through the new opening. The ends of this large tube were tied off with square knots, and, after the excess tube was cut, the remaining part was left behind for retraction. After intubation, the nasal cavity was packed with polyurethane foam soaked in antibiotics (Nasopore; Polyganics, Groningen, the Netherlands).
Postoperatively, the patients were instructed to use antibiotics and steroid eye drops four times daily. They were also instructed to be careful when wiping or touching the corners of the affected eyes. Silicone tubes were removed during an outpatient visit approximately 3 months after surgery. However, if patients had persistent epiphora, tubes were left in place for a longer period. The silicone tubes were removed by cutting the interpunctal portions and retracting the ends from the nose. The patients were followed up for endoscopic removal of crusts as well as for monitoring the patency of the nasolacrimal duct system by syringing at 1 week and 1, 2, and 3 months after surgery as well as every 3 months thereafter.
The anatomical, functional, and overall success rates of both groups were determined 3 months after surgery. Anatomical success was defined as either good fluid passage with no resistance or the absence of reflux during lacrimal irrigation. Functional success rate was determined by evaluating subjective ocular symptoms, and epiphora severity was assessed using the Munk score [11]. A Munk score of 0 to 1 defined the surgery as a functional success, while a score of 2 to 5 defined the surgery as a functional failure. Additionally, the data regarding patient age, sex, mean follow-up duration, number of reoperations, and laterality of involvement were reviewed. Complications related to the DCR or the tube itself were also investigated. Statistical analyses were performed using the commercially available software SPSS ver. 12.0 for Windows (SPSS Inc., Chicago, IL, USA). Differences in the parameters between the two groups were analyzed using the independent t-test, chi-square test, and Fisher's exact test. A p-value < 0.05 was considered to indicate significance.
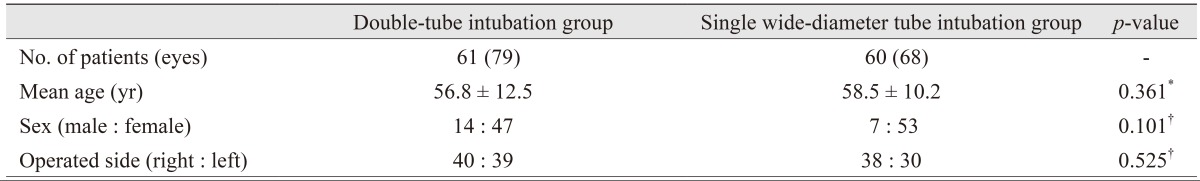
A total of 121 patients (average age, 57.0 ± 11.9 years; range, 16 to 86 years), including 21 male (17.4%) and 100 female (82.6%) patients, were evaluated in this study. There were no major intraoperative or immediate postoperative complications during endonasal DCR. Of the 121 patients, two silicone tubes were placed in 79 eyes of 61 patients, and a single wide-diameter silicone tube was placed in 68 eyes of 60 patients. There were no significant differences in the distribution of the clinical characteristics between the two groups. The mean follow-up period was 8.09 ± 5.91 months and 7.90 ± 4.59 months in the double-tube and single wide-diameter tube intubation groups, respectively. The patient demographics are summarized in Table 1.
The success rates of both methods were evaluated at 3 months after surgery to compare the efficacies of the intubation materials. Upon lacrimal irrigation, 72 of the 79 eyes (91.1%) in the double-tube intubation group showed good fluid passage without resistance or reflux. In the single wide-diameter tube intubation group, 60 of the 68 eyes (88.2%) showed good fluid passage, and there was no statistically significant difference between the anatomical success rates of the two groups. Functional success rate, as assessed by the Munk score [11], was 82.3% (65 of 79 eyes) in the double-tube group and 89.7% (61 of 68 eyes) in the single wide-diameter tube intubation group; the difference between the functional success rates of the two groups was not statistically significant (Table 2).
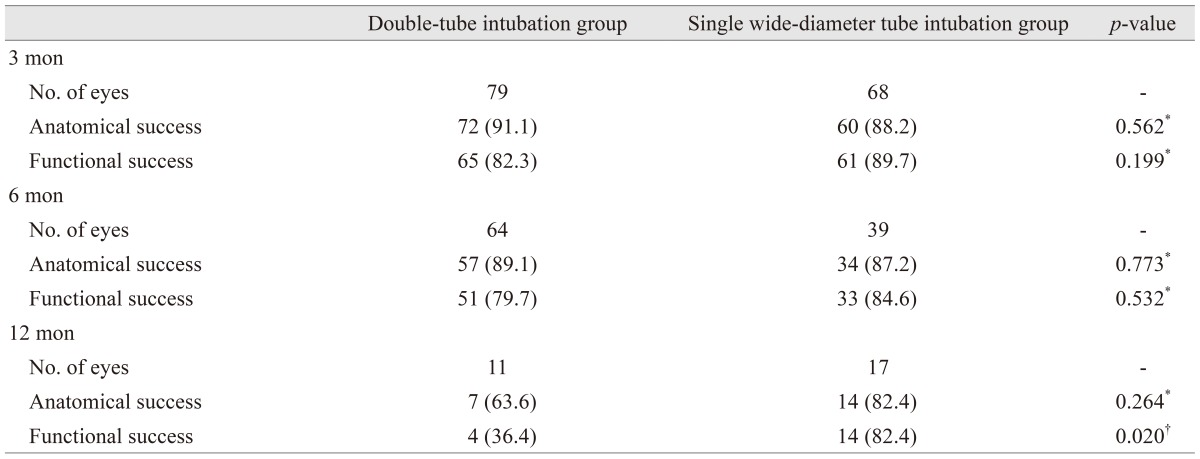
Additionally, long-term success rates for both methods were evaluated. Six months after the surgery, 64 eyes of the double-tube intubation group and 39 eyes of the single wide-diameter intubation tube group were followed. The anatomical success rate was 89.1% in the double-tube intubation group and 87.2% in the single wide-diameter tube intubation group, while the functional success rate was 79.7% in the former group and 84.6% in the latter. These slight differences in success rates were not statistically significant. Twelve months after the surgery, 11 eyes of the double-tube intubation group and 17 eyes of the single wide-diameter tube intubation group were followed. The anatomical success rate was 64.6% in the double-tube intubation group and 88.4% in the singe wide-diameter intubation group, while the functional success rate was 36.4% (4 of 11 eyes) in the former group and 82.4% (14 of 17 eyes) in the latter. This difference between groups was statistically significant (p = 0.020) (Table 3).
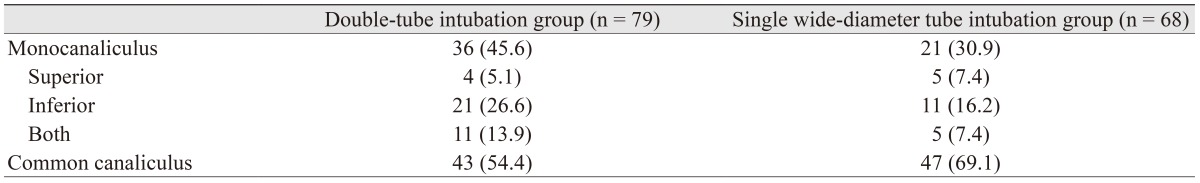
The level of obstruction was assessed as described earlier. The most common site of obstruction was the common canaliculus, which was found to be obstructed in 54.4% of the cases in the double-tube intubation group and 69.1% of the cases in the single wide-diameter tube intubation group. Although the incidence of distal canaliculus obstruction was higher in the double-tube intubation group than in the single wide-diameter tube intubation group, there was no significant difference in incidence between the two groups (p = 0.068) (Table 4).
While one patient in the double-tube intubation group underwent reoperation for epiphora by CDCR, two patients in the single wide-diameter tube intubation group underwent reoperation for recurrence, one by CDCR and the other by reintubation (Table 5).
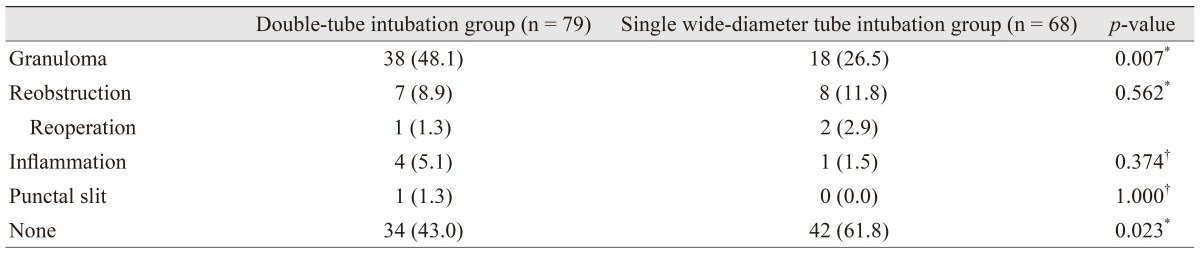
There were no significant differences in the final anatomical or functional success rates between the two groups. However, there were differences between the two groups in terms of the occurrence of minor postoperative complications such as the formation of lower punctal slit, minor inflammation near the canaliculi, reobstruction, and granulation near the bony opening in the nasal cavity. The rates of incidence of inflammation and reobstruction were similar between the two groups. However, the rates of incidence of granulation and postoperative complications were higher in the double-tube intubation group than in the single wide-diameter tube intubation group. Extrusion or malpositioning of the silicone tubes was easily corrected using a nasal endoscope and intranasal forceps. In cases of patients with granulated tissue at follow-up, endoscopic removal was performed in the outpatient clinic. Minor inflammation near the canaliculi was easily managed using antibiotic eye drops and oral antibiotics (Table 5).
Successful treatment of canalicular obstruction continues to present a therapeutic challenge. Although CDCR is the standard treatment in patients with extensive canalicular obstruction, many studies have reported relatively high rates of complications and poor patient satisfaction [12]. Owing to the development of surgical techniques and instruments, endonasal DCR, a less invasive method, is now widely used to treat canalicular obstruction. Following DCR, silicone tubes are inserted into each canaliculus in order to prevent adherence of the mucosal lining of the ducts during healing and to maintain long-term patency. Various instruments and methods have been described for achieving increased anatomical and functional success rates in lacrimal intubation [2491013]. The aim of this study was to compare the clinical efficacies of two different intubation methods—double silicone intubation and single wide-diameter tube intubation.
The efficacy of double silicone intubation has been reported by many studies. Demirci and Elner [6] assessed the results of double silicone intubation and reported that 79% of the patients included in their study experienced symptom resolution. Additionally, Hwang et al. [7] reported anatomical and functional success rates of 96.5% and 88.3%, respectively, while Paik et al. [14] reported rates of 91.4% and 82.8%. They suggested that double silicone intubation might be a more successful procedure for the treatment of canalicular obstruction than balloon catheter dilatation, at a considerably lesser cost [6]. The reasons for the higher success rates of double silicone intubation in comparison to the other techniques are the greater dilation of the lacrimal system achieved by this method and prevention of restenosis after stent removal. In double-tube bicanalicular intubation, complications such as punctal or canalicular slitting can be expected while inserting the second tube into the punctum already occupied by the first tube. However, none of the previous studies have reported any serious complications during this procedure. Moreover, enlargement of the lacrimal punctum with an incision facilitates the entrance of the second silicone tube. Additionally, these complications can be avoided by advancing the tubes gently according to the contours of the canaliculus. During double silicone intubation, patients might experience local discomfort because of the greater dilation of the canaliculus; however, most patients tolerate this discomfort well. In the present study, the surgical results of double-tube intubation after endonasal DCR showed success rates similar to those reported in the previous studies.
Yildiz et al. [10] and Hurwitz [2] introduced another intubation method employing a single wide-diameter tube. Hurwitz [2] suggested that wide-diameter stents would dilate the lacrimal system more easily and successfully. Yildiz et al. [10] reported no failures or difficulties related to the larger tube size, and Hurwitz [2] reported relief of epiphora in six of seven patients and no complications other than one case of punctal granuloma. The anatomical and functional success rates of single wide-diameter tube intubation in the present study were 88.2% and 89.7%, respectively, which are consistent with those reported in previous studies on the outcomes of wide-stent intubation.
In the present study, although the mean follow-up period in the double-tube intubation group was slightly longer than that in the single wide-diameter tube intubation group, the difference between the two groups was not statistically significant (p = 0.828). We removed the silicone tubes in a routine procedure around 3 months after DCR by cutting their interpunctal portions and retracting the ends from the nose. Based on the theory that retention of a stent within the nasolacrimal system might widen the canalicular space and prevent adhesion of the mucosal lining, intubation for longer duration might help increase the success rates of this procedure. Demirci and Elner [6] reported that scarring responses reach their final configuration in approximately 1 year. However, Paik et al. [14] stated that tube stenting for a longer duration is not required to achieve effective treatment. In our study, the overall success rates of both groups after 3 months of intubation (82.3% and 80.9% in the double-tube and single wide-diameter tube intubation groups, respectively) were similar to those reported in previous studies. In this study, we examined follow-up visits that occurred more than 3 months after surgery. Six months after surgery, the success rates in both groups were similar to those observed 3 months after surgery. However, 12 months after surgery, the anatomical and functional success rates had declined in the double-tube intubation group. Further research is needed to verify these results because many patients were lost to follow up. However, the higher success rate in the single wide-diameter tube group at 12 months indicates that it may be advantageous to use single wide-diameter tube in treating canalicular stenosis and/or obstruction.
We compared the efficacies of double silicone tube intubation and single 0.94-mm silicone tube intubation in the treatment of distal or common canalicular obstruction. Both methods showed high overall success rates (82.3% and 80.9% in the double-tube and single wide-diameter tube intubation groups, respectively) consistent with those reported previously. There were no significant differences in any of the clinical characteristics between the two groups. Patients who underwent double silicone intubation were diagnosed with common canalicular obstruction in 54.4% of the cases and monocanalicular obstruction in 45.6% of the cases. In the single wide-diameter intubation group, 69.1% of the eyes showed common canalicular obstruction, and 30.9% showed monocanalicular obstruction. The proportions of each of the diagnoses were different between the two groups; however, the differences were not statistically significant (p = 0.068).
Single wide-diameter silicone intubation is advantageous since the procedure does not require additional procedures for the management of the puncta, such as dilatation or punctoplasty, and has a lower risk of inflammation compared to double silicone intubation. The presence of two tubes in a canaliculus might induce greater friction between the tubes and, consequently, greater irritation of the eye. Single wide-diameter silicone intubation exhibits as high a success rate as double silicone intubation, with fewer complications such as inflammation and ocular irritation. We, therefore, suggest that single wide-diameter silicone intubation could be a better primary choice for the treatment of monocanalicular or common canalicular stenosis/obstruction compared to double silicone intubation.
There are several limitations to the present study. First, our study was retrospective, and the two different types of surgeries were not performed simultaneously. Additionally, the mean follow-up period in our study was shorter than that in similar previous studies. After removal of the tubes, the patients included in our study did not often present for follow-up; this might largely have been due to the relief of symptoms. Finally, our study did not assess the efficacy of the 0.64-mm single-tube intubation. However, many previous studies have reported the success rates of single, double, and wide-diameter intubations.
The results of our study indicate that double silicone tube stenting and single wide-diameter tube stenting in endoscopic DCR are effective treatments for patients with distal or common canalicular obstruction.
Notes
References
1. Bartley GB, Gustafson RO. Complications of malpositioned Jones tubes. Am J Ophthalmol. 1990; 109:66–69. PMID: 2297034.

2. Hurwitz JJ. A new, wider-diameter Crawford tube for stenting in the lacrimal drainage system. Ophthal Plast Reconstr Surg. 2004; 20:40–43.

3. Crawford JS. Intubation of obstructions in the lacrimal system. Can J Ophthalmol. 1977; 12:289–292. PMID: 922571.
4. Inatani M, Yamauchi T, Fukuchi M, et al. Direct silicone intubation using Nunchaku-style tube (NST-DSI) to treat lacrimal passage obstruction. Acta Ophthalmol Scand. 2000; 78:689–693. PMID: 11167235.

5. Lauring L. Silicone intubation of the lacrimal system: pitfalls, problems and complications. Ann Ophthalmol. 1976; 8:489–498. PMID: 1267321.
6. Demirci H, Elner VM. Double silicone tube intubation for the management of partial lacrimal system obstruction. Ophthalmology. 2008; 115:383–385. PMID: 18243905.

7. Hwang SW, Khwarg SI, Kim JH, et al. Bicanalicular double silicone intubation in external dacryocystorhinostomy and canaliculoplasty for distal canalicular obstruction. Acta Ophthalmol. 2009; 87:438–442. PMID: 18700890.

8. Kashkouli MB, Pakdel F, Kiavash V. Assessment and management of proximal and incomplete symptomatic obstruction of the lacrimal drainage system. Middle East Afr J Ophthalmol. 2012; 19:60–69. PMID: 22346116.

9. Kim SJ, Kim SD. The surgical results of endonasal DCR with two silicone tubes in common canalicular obstruction. J Korean Ophthalmol Soc. 2007; 48:1170–1176.

10. Yildiz M, Yazici B, Akova B, Karatas A. A new and simple silicone intubation method for dacryocystorhinostomy. Eur J Gen Med. 2011; 8:36–39.
11. Munk PL, Lin DT, Morris DC. Epiphora: treatment by means of dacryocystoplasty with balloon dilation of the nasolacrimal drainage apparatus. Radiology. 1990; 177:687–690. PMID: 2243969.

12. Liarakos VS, Boboridis KG, Mavrikakis E, Mavrikakis I. Management of canalicular obstructions. Curr Opin Ophthalmol. 2009; 20:395–400. PMID: 19587600.

13. Kurihashi K. Bicanalicular silicone intubation using three-piece silicone tubing: direct silicone intubation. Ophthalmologica. 1993; 206:57–68. PMID: 8272326.

14. Paik JS, Cho WK, Yang SW. Bicanalicular double silicone stenting in endoscopic dacryocystorhinostomy with lacrimal trephination in distal or common canalicular obstruction. Eur Arch Otorhinolaryngol. 2012; 269:1605–1611. PMID: 22130914.

Table 2
Comparison of the postoperative parameters of the two groups
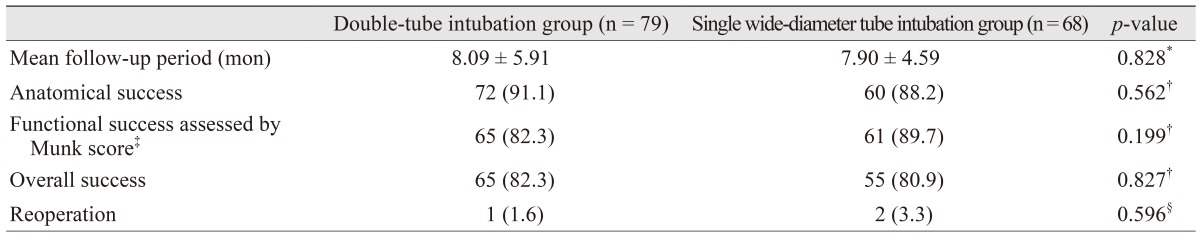
Values are presented as mean ± standard deviation or number (%).
*By independent t-test; †By Pearson's chi-square test; ‡Munk score criteria was defined as follows: grade 0, no epiphora; grade 1, occasional epiphora requiring dabbing less than twice a day; grade 2, epiphora requiring dabbing 2 to 4 times daily; grade 3, epiphora requiring dabbing 5 to 10 times daily; grade 4, epiphora requiring dabbing more than 10 times per day; grade 5, constant tearing. Munk score: 0–1, success; 2–5, failure; §By Fisher's exact test.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download