Abstract
Purpose
To investigate the long-term clinical course of intermittent exotropia after surgical treatment to determine whether and when postoperative exo-drift stabilizes, and the required postsurgery follow-up duration in cases of intermittent exotropia.
Methods
We retrospectively reviewed the medical records of patients diagnosed with intermittent exotropia who underwent surgical treatment between January 1992 and January 2006 at Yeungnam University Hospital and postoperatively performed regular follow-up examinations for up to 7 years. We also analyzed the difference in exo-drift stabilization, according to surgical procedure.
Results
A total of 101 patients were enrolled in the study. Thirty-one patients underwent lateral rectus recession and medial rectus resection (R&R) and 70 patients underwent bilateral lateral rectus recession (BLR). The postoperative angles of deviation increased significantly during the initial 36 months, but no subsequent significant changes were observed for up to 84 months. Follow-ups for 7 years revealed that more than 50% of the total amount of exo-drift was observed within the first postoperative year. In addition, the angles of deviation at 1 year correlated with those at 7 years postoperatively (Pearson correlation coefficient r = 0.517, p < 0.001). No significant exo-drift was observed after 36 months in patients who underwent BLR, whereas after 18 months in patients who underwent R&R.
Conclusions
The minimum postoperative follow-up required after surgical treatment to ensure stable results is 36 months. In particular, careful follow-up is necessary during the first postoperative year to detect rapid exo-drift. Patients who underwent BLR required a longer follow-up than those who underwent R&R to ensure stable postoperative alignment.
Intermittent exotropia is the most common type of strabismus among Asians. Surgical treatment is recommended in most cases because it results in better outcomes than non-surgical treatment, including orthoptic or occlusion therapy [1]. Many authors, however, report postoperative exo-drift and the recurrence of intermittent exotropia over time after surgery [2,3,4,5,6,7]. Therefore, regular postoperative follow-up is important for intermittent exotropia patients because of possible recurrence. Patients frequently ask about the duration of postoperative follow-up and time to decreased risk of recurrence. For some patients with good long-term ocular alignment after surgery, a continued long-term follow-up can be burdensome. However, due to possible recurrence that could potentially require a second surgery, strabismologists might be reluctant to halt follow-up. Accordingly, we examined whether there is a definitive postoperative period of exo-drift stabilization in intermittent exotropia which can be used to determine the appropriate end-point of follow-up after surgery. Therefore, we investigated the long-term clinical course of intermittent exotropia following surgical treatment for up to 7 years, to determine when the postoperative exo-drift of intermittent exotropia stabilizes and determined the optimal postoperative follow-up end-point for intermittent exotropia.
A retrospective review of the medical records of intermittent exotropia patients who underwent surgical treatment between January 1992 and January 2006 at Yeungnam University Hospital was performed. Approval for this study was obtained from the institutional review board of Yeungnam University Hospital. Inclusion in this study required a post-surgery follow-up of at least 7 years. Patients with severe unilateral amblyopia, patients with any other type of strabismus (including oblique muscle dysfunction, dissociated vertical deviation, A-V pattern, nystagmus, and previous strabismus), or intraocular surgery were excluded, as were patients with any neurologic impairment, including cerebral palsy.
At the initial visit, all of the patients underwent a full ophthalmologic examination, including visual acuity testing, ocular alignment status, slit-lamp biomicroscopy, refraction, fundus examination, and stereoacuity testing. The angle of deviation was measured by alternate prism cover testing at 6-m and 33-cm fixation in cooperative children both preoperatively and postoperatively. Best-corrected visual acuity was measured when possible. Amblyopia was defined as an interocular difference in visual acuity of two lines or more. If amblyopia was detected, occlusion therapy was performed to treat amblyopia as soon as possible before surgery. Stereoacuity was measured using the Lang I test (Lang-Stereotest AG, Küsnacht, Switzerland) and the Titmus (Stereo Fly Stereotest; Stereo Optical Co., Chicago, IL, USA) test when patients were able to cooperate and complete the test.
All surgeries were performed under general anesthesia by a single surgeon (MMK). Bilateral lateral rectus recession (BLR) or unilateral lateral rectus recession and medial rectus resection (R&R) was performed at Yeungnam University Hospital based on the patient's angle of deviation measured the day before the surgery (Table 1). The surgeon preferred BLR for exotropia with 25 prism diopters based on prior surgical experiences [8].
Patients were followed up at 1, 3, 6, and 12 months after surgery, and every 6 months thereafter. The postoperative angle of deviation was measured at each visit. Postoperative exo-drift was defined as the angle of deviation at the particular follow-up visit. Patients who missed any regular follow-up appointments over the postoperative 7 years were excluded from the study.
Continuous data are presented as means ± standard deviation and categorical data as counts. Comparisons for continuous variables were performed using an independent t-test or paired t-test. The chi-square method was used to test the significance of differences between proportions and categorical variables. We compared the postoperative angles of deviation with those of previous visits throughout the follow-ups to determine the time required for stabilization. Stabilization of exo-drift was defined as no statistically significant difference between the postoperative angle of deviation and that of the previous visit. In addition, we analyzed the postoperative angle stabilization periods required for BLR and R&R. IBM SPSS statistical software ver. 20.0 (IBM Co., Armonk, NY, USA) was used for statistical analyses. A p-value less than 0.05 was considered statistically significant.
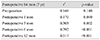
A total of 101 intermittent exotropia patients met the inclusion criteria. Of these patients, 31 patients underwent R&R and 70 patients underwent BLR. The demographic and clinical characteristics of the subjects are summarized in Table 2. The study group was comprised of 45 males and 56 females, with a mean age 6.36 ± 1.88 years (range, 3 to 12 years) at surgery, and a mean follow-up period of 8.87 ± 1.87 years (range, 7 to 14 years). All patients had basic intermittent exotropia, defined as the difference between the distance and near angle of less than 10 prism diopters. The pre- and postoperative changes in angles of deviation are presented in Table 3. The postoperative angles of deviation increased significantly over the first 36 months of follow-ups. After 36 months, however, no significant difference was detected for up to 84 months (Fig. 1).
Analysis of the differences in exo-drift between the two types of surgical procedures revealed no further significant exo-drift after 36 months following BLR, and no significant exo-drift after 18 months following R&R (Fig. 1). Therefore, the R&R procedure resulted in earlier exo-drift stabilization compared to BLR. Comparison of the exo-drift changes over 7 years indicated that more than half of the total amount of exo-drift occurred during the first postoperative year (mean angle of deviation at postoperative 1 year / mean angle of deviation at postoperative 7 years, 68.1%). Furthermore, the postoperative angles of deviation at the first postoperative year strongly correlated with those at the final 7-year follow-up (Pearson correlation coefficient r = 0.517, p < 0.001) (Table 4).
Postoperative exo-drift of intermittent exotropia is common [4,9,10,11,12]. Therefore, intermittent exotropia patients should be followed up for some time after surgical treatment to monitor postoperative exo-drift and recurrence. During the postoperative follow-up, we are frequently asked by patients or their parents whether the follow-up is required and, if so, the anticipated duration. It is not a straightforward matter for strabismologists to decide when to discontinue postoperative follow-up because of the possibility of recurrence. For patients, however, continued follow-up over an indefinite period is burdensome, and is probably the reason that some patients with good ocular alignment during the early postoperative period are lost to follow-up. Therefore, we attempted to define the stabilization period for postoperative exo-drift in intermittent exotropia to aid both the clinician and patient to determine the appropriate follow-up period. We analyzed the long-term clinical courses of an intermittent exotropia cohort to determine postoperative exo-drift stabilization.
In this study, the postoperative angles of deviation increased over time until postoperative 36 months, with no significant changes observed subsequently. This finding indicates that postoperative exo-drift stabilizes after 36 months. Therefore, the minimum postoperative follow-up duration to ensure good and stable results is 36 months following surgical treatment. Our finding is consistent with the report of Kwon et al. [12], in which the angles of deviation in intermittent exotropia were analyzed postoperatively for up to 5 years. In the present study, we analyzed the postoperative clinical course of intermittent exotropia for up to 7 years, and demonstrated a longer duration of sustained deviation after stabilization. To enhance the accuracy of the analysis, patients who missed any regular follow-up visit during the postoperative 7 years period were excluded from the present study. Furthermore, we obtained postoperative data at 1, 3, 6, and 18 months. Therefore, the present study provides more detailed results for the early postoperative period.
In terms of the amount of exo-drift, more than half of the observed exo-drift occurred during the first postoperative year. In addition, the angles of deviation in the first postoperative year were more highly correlated with those at 7 years than at any other visit. The association between preoperative exodeviation and surgical outcome of intermittent exotropia is controversial. Park and Kim [9] reported that the rate of exo-drift correlates with the size of the preoperative deviation. Two studies by Lim et al. [13,14], however, indicated that preoperative deviation is not a predictive factor for successful surgery. In the present study, preoperative deviation did not significantly correlate with postoperative deviation at 7 years. Additionally, the angles of deviation at 1 month were not significantly correlated with those at 7 years. These findings indicate that careful follow-up is necessary during the first postoperative year to detect rapid exo-drift.
Our analysis of the stabilization periods, according to surgical procedure, indicated that patients who underwent R&R exhibited greater exo-drift than those who underwent BLR after the 3-month postoperative follow-up. Nevertheless, angle stabilization was achieved in R&R within 18 months—this is 18 months earlier than BLR. Therefore, although intermittent exotropia patients who underwent BLR displayed a smaller degree of exo-drift than those who underwent R&R, they required a longer follow-up period to ensure good long-term surgical results. A possible explanation is that the initial tethering effect secondary to a medial rectus resection results in initially favorable outcomes and earlier stabilization compared to the BLR [15]. Considering that BLR and R&R are the most commonly used surgical methods to correct intermittent exotropia, our results can be applied to the majority of surgically-treated intermittent exotropia patients.
Our findings are limited by the retrospective nature of the study. Consequently, the preoperative deviations of patients that underwent R&R were larger than those of patients that underwent BLR in the analysis of the stabilization periods, according to surgical procedure, because we selected the surgical procedure according to the preoperative deviation and preferred R&R for large angle exotropia. A future prospective study with randomly assigned surgical procedures would provide more information on the difference in exo-drift stabilization.
In conclusion, our results demonstrated that exo-drift in intermittent exotropia after surgical treatment stabilizes after 36 months postoperatively. More than half of the exo-drift that occurred in patients was during the first postoperative year. In terms of the type of surgical procedure, earlier stabilization of the postoperative angle was achieved in R&R compared with BLR. We believe the results of this study will be helpful for determining postoperative follow-up duration in individual cases.
Figures and Tables
 | Fig. 1Postoperative angles of deviation in intermittent exotropia and statistical differences between each follow-up. BLR = bilateral lateral rectus recession; R&R = lateral rectus recession and medial rectus resection. *Statistically significant, p < 0.05. |
Table 2
Demographic and clinical characteristics of the patients with intermittent exotropia

Categorical variables are reported using proportions, and continuous variables are reported using means ± standard deviation. The plus numbers represent hyperopia and the minus numbers represent myopia.
PD = prism diopters; SE = spherical equivalent; D = diopters; BLR = bilateral lateral rectus recession; R&R = lateral rectus recession and medial rectus resection; arcsec = arcsecond.
Notes
References
1. Figueira EC, Hing S. Intermittent exotropia: comparison of treatments. Clin Experiment Ophthalmol. 2006; 34:245–251.
2. Ekdawi NS, Nusz KJ, Diehl NN, Mohney BG. Postoperative outcomes in children with intermittent exotropia from a population-based cohort. J AAPOS. 2009; 13:4–7.
3. Kim WJ, Kim MM. The clinical course of recurrent intermittent exotropia following one or two surgeries over 24 months postoperatively. Eye (Lond). 2014; 28:819–824.
4. Scott WE, Keech R, Mash AJ. The postoperative results and stability of exodeviations. Arch Ophthalmol. 1981; 99:1814–1818.
5. Choi J, Chang JW, Kim SJ, Yu YS. The long-term survival analysis of bilateral lateral rectus recession versus unilateral recession-resection for intermittent exotropia. Am J Ophthalmol. 2012; 153:343–351.e1.
6. Pineles SL, Ela-Dalman N, Zvansky AG, et al. Long-term results of the surgical management of intermittent exotropia. J AAPOS. 2010; 14:298–304.
7. Maruo T, Kubota N, Sakaue T, Usui C. Intermittent exotropia surgery in children: long term outcome regarding changes in binocular alignment. A study of 666 cases. Binocul Vis Strabismus Q. 2001; 16:265–270.
8. Mun HJ, Kim MM. Comparison of surgical results between bilateral recession and unilateral recession-resection in 25 PD intermittent exotropia. J Korean Ophthalmol Soc. 2002; 43:2202–2207.
9. Park KH, Kim SY. Clinical characteristics of patients that experience different rates of exodrift after strabismus surgery for intermittent exotropia and the effect of the rate of exodrift on final ocular alignment. J AAPOS. 2013; 17:54–58.
10. Leow PL, Ko ST, Wu PK, Chan CW. Exotropic drift and ocular alignment after surgical correction for intermittent exotropia. J Pediatr Ophthalmol Strabismus. 2010; 47:12–16.
11. Kordic H, Sturm V, Landau K. Long-term follow-up after surgery for exodeviation. Klin Monbl Augenheilkd. 2009; 226:315–320.
12. Kwon J, Kim SH, Cho YA. Postoperative stabilization of the strabismic angle in intermittent exotropia. Korean J Ophthalmol. 2012; 26:446–450.
13. Lim SH, Hong JS, Kim MM. Prognostic factors for recurrence with unilateral recess-resect procedure in patients with intermittent exotropia. Eye (Lond). 2011; 25:449–454.
14. Lim SH, Hwang BS, Kim MM. Prognostic factors for recurrence after bilateral rectus recession procedure in patients with intermittent exotropia. Eye (Lond). 2012; 26:846–852.
15. Yang X, Man TT, Tian QX, et al. Long-term postoperative outcomes of bilateral lateral rectus recession vs unilateral recession-resection for intermittent exotropia. Int J Ophthalmol. 2014; 7:1043–1047.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download