Abstract
Purpose
To investigate the changes in corneal higher-order aberration (HOA) during amblyopia treatment and the correlation between HOA and astigmatism in hyperopic amblyopia children.
Methods
In this retrospective study, a total of 72 eyes from 72 patients ranging in age from 38 to 161 months were included. Patients were divided into two groups based on the degree of astigmatism. Corneal HOA was measured using a KR-1W aberrometer at the initial visit and at 3-, 6-, and 12-month follow-ups. Correlation analysis was performed to assess the association between HOA and astigmatism.
Results
A total of 72 patients were enrolled in this study, 37 of which were classified as belonging to the higher astigmatism group, while 35 were assigned to the lower astigmatism group. There was a statistically significant difference in success rate between the higher and lower astigmatism groups. In both groups, all corneal HOAs were significantly reduced during amblyopia treatment. When comparing the two groups, a significant difference in coma HOA at the 12-month follow-up was detected (p = 0.043). In the Pearson correlation test, coma HOA at the 12-month follow-up demonstrated a statistically significant correlation with astigmatism and a stronger correlation with astigmatism in the higher astigmatism group than in the lower astigmatism group (coefficient values, 0.383 and 0.284 as well as p = 0.021 and p = 0.038, respectively).
Amblyopia is defined as a unilateral or bilateral decreasein visual acuity in the absence of ocular pathology [1]. Amblyopia has been related to unequal foveal stimulation in early age due to vision deprivation, strabismus, or refractive error. Amblyopia treatment techniques exhibit diverse outcomes based on the degree of the initial cause, disease, age at the start of amblyopia treatment, and patient compliance [2]. Although the definition of success for amblyopia treatment varies, the reported success rate of amblyopia treatment approached 60% [34].
Several studies have documented the relationship between higher-order aberration (HOA) and amblyopia [56]. HOA is a known index of visual quality. Yoon and Williams [5] reported that, when ocular aberration increases during development, visual symptoms such as glare, halo, and distortion can occur, and correction of HOA using adaptive optics improved contrast sensitivity and visual acuity. Another study reported that correcting HOA significantly improved visual acuity. HOA correction using adaptive optics can induce subjectively obvious improvements to vision sharpness [6]. Therefore, HOA could affect the results of amblyopia treatment. However, little is known about the relationship between HOA and amblyopia treatment.
Prakash et al. [7] reported that a subset of "idiopathic" amblyopia might be associated with loss of symmetry in wavefront patterns of the two eyes and proposed that interocular differences in HOA explain the reduced visual acuity in cases of idiopathic amblyopia. Therefore, HOA could affect the results of amblyopia treatment. According to our previous study [8], HOA should be considered a reason for amblyopia treatment failure. HOA, particularly spherical aberration, was statistically more common in the amblyopia treatment failure group than in the rest of the group. We conducted this consecutive study to elucidate the role of HOA in hyperopic isometropic amblyopia treatment.
Regarding the measurement of HOA, Shack-Hartmann aberrometry provided the accurate, objective data needed for diagnosing abnormal optics [910]. Aberrometers present the magnitude and sign of each HOA via a string of Zernike coefficients. This instrument calculates the root mean square (RMS) wavefront error for these modes and quantifies them as a single number. The KR-1W aberrometer (Topcon Medical System, Tokyo, Japan) measures ocular aberrations using ocular aberrometry and corneal topography [11]. The advantage of this calculation is that it always uses the same reference axis, thereby avoiding errors caused by misalignment when measuring wavefront profiles.
Levy et al. [10] stated that the main risk factor of development of amblyopia is lower-order aberration, such as defocus and astigmatism. However, another study reported that HOA must also be considered [12].
Therefore, in this study, we compared differences in amblyopia treatment success rates with regard to astigmatism and investigated the relationship between astigmatism and HOA using a KR-1W aberrometer in children with hyperopic amblyopia.
We retrospectively reviewed the medical records of hyperopic amblyopia patients treated from March 2010 to March 2015 in the Pediatric Ophthalmology Department at the Inje University Ilsan Paik Hospital. Clinical data included patient age at initial visit, gender, uncorrected visual acuity, best-corrected visual acuity (BCVA), alternate cover test, and slit-lamp and fundus examinations. We calculated spherical equivalent (SE) according to cycloplegic refraction results at the initial and follow-up visits. Hyperopic isometropic amblyopia was defined as bilateral hyperopia representing a difference in SE of 1.00 diopter (D) or less between the eyes, as well as a BCVA of 0.5 or less when the patient was younger than 6 years or 0.63 or less when the patient was 6 years or older. After finding that there were no such differences in SE between the eyes, only right eye data was presented. Patients with complete 12-month follow-up examinations and treatments were included in this study. Patients with a difference of 1.00 D or more in astigmatism between the eyes, strabismus with a prism angle more than 5.0 prism diopters, abnormalities in the anterior segment of the eye or fundus, history of ocular diseases, ocular trauma, ocular surgery, contact lens usage, and poor spectacle usage compliance for less than half of the waking hours were excluded from this study. Based on the degree of astigmatism, individuals were categorized into higher and lower astigmatism groups. Patients with astigmatism of at least 1.50 D were classified into the higher astigmatism group, and patients with astigmatism of less than 1.50 D were classified into the lower astigmatism group. Prescription spectacles were created according to cycloplegic refraction measurement values and BCVA measurements.
Conformation of spectacle usage was completed at the 1-month follow-up. Compliance with spectacle wear was assessed according to patient and parental reports at each visit. The amount of time spent wearing the spectacles was recorded (excellent, all waking hours; fair, half or more of the waking hours; poor, less than half of the waking hours). Based on BCVA monitoring after the 12-month follow-up, the results of amblyopia treatment using spectacles were determined. Successful amblyopia treatment was defined as a BCVA of 0.63 or more when the patient was younger than 6 years or 0.80 or more when the patient was 6 years or older.
HOA was measured for all patients using a KR-1W aberrometer after the initial visit and at 3-, 6-, and 12-month follow-ups. All HOA measurements were performed in a dark room, and the patient was asked to blink once while facing the scanner and then focus on the fixation target before the scan was performed. HOA measurements were repeated until the patient followed all instructions. We chose the best scans using an unbroken Placido's disk, and eye imaging was performed when the eye was open. Then, the HOAs were analyzed using RMS values. Total HOAs, trefoil, coma, and spherical aberrations were obtained from each compartment with a 6.0-mm pupil. Statistical analysis was performed with PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA). Fisher's exact test was used to compare success between groups. A paired t-test was used to compare the measurements within each group, and an independent t-test was used to compare between-group measurements. The Pearson correlation test was performed to evaluate the correlation between HOA and astigmatism. Age at initial visit, initial BCVA, value of spherical anisometropia, and RMS values for total, trefoil, coma, and spherical HOAs were used in the analysis. A p-value less than 0.05 was considered statistically significant.
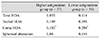
A total of 72 hyperopic amblyopia patients were included in this study. All individuals attended every follow-up, including the initial visit and the 1-, 3-, 6- and 12-month follow-ups. The mean age at the initial visit was 64.1 months (range, 38 to 161 months) (Table 1). Higher astigmatism was identified in 37 patients (51.4%) and lower astigmatism in 35 (38.6%).
The mean monochromatic aberrations of the patients are also shown in Table 1. The total HOA, coma HOA, trefoil HOA, and spherical aberration were 0.46 ± 0.13, 0.28 ± 0.13, 0.18 ± 0.37, and 0.25 ± 0.33, respectively. There were no statistically significant differences between the two groups in terms of age, BCVA, SE, or total, trefoil, coma, and spherical HOAs at the initial visit (p > 0.05).
Amblyopia treatment was successful in 20 patients in the higher astigmatism group (54.1%) and 25 patients in the lower astigmatism group (71.4%) after 12 months of treatment (Fig. 1). There was a statistically significant difference in success rate between the higher and lower astigmatism groups (Fisher's exact test, p = 0.023).
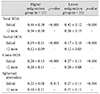
When comparing the two groups, coma HOA was significantlyhigher in the higher astigmatism group at 12months (p = 0.033) (Fig. 2A-2D). Total, trefoil, and comaHOAs, as well as spherical HOA, demonstrated statisticallysignificant decreases within the groups according to thefollow-up data (Table 2). There were no significant differencesin total HOAs, trefoil HOAs, or spherical aberrationbetween the two groups (p > 0.05).
Based on the Pearson correlation test, coma HOA at the 12-month follow-up showed a statistically significant correlation with astigmatism in the higher and lower astigmatism groups (p = 0.021 and p = 0.038; coefficient values, 0.383 and 0.284, respectively) (Table 3).
In our previous study [8], HOA was considered a reason for failed amblyopia treatment. We concluded that ocular and internal spherical aberrations in particular were statistically higher in children with failed amblyopia treatment. This finding suggests that, in amblyopic eyes of hyperopic anisometropia individuals, HOA results from higher internal spherical aberration, which is characteristic of patients experiencing failed amblyopia treatment. This previous study included children with anisometropic hyperopic amblyopia and demonstrated the effects of HOA during amblyopia treatment and further evaluated the effects of HOA depending on astigmatism level.
However, there have been conflicting results regarding the correlation between amblyopia and HOA. Dominguez-Vicent et al. [11] documented that HOA alone does not play a major role in compromising the visual performance of idiopathic amblyopic eyes. Using an adaptive optics visual simulator, the authors directly compared visual performance achieved with different ocular conditions in the same patients. However, their study included a small sample size of adult patients. In the case of normal eyes, Levy et al. [10] found no correlation between wavefront aberration and refractive error. No significant differences were found between patients with supernormal vision and those with myopia. The authors concluded that the main risk factor of development of amblyopia was lower-order aberration, such as defocus and astigmatism. However, they included adult patients with uncorrected visual acuity values higher than 20 / 15. Thus, they underestimated the effects of HOA on the visual quality of amblyopic children. Another study estimated the impact of HOA on visual quality and reported that lower-order aberration accounted for approximately 90% of retinal image quality, and the remaining 10% could be attributed to HOAs [12]. Those authors concluded that lower-order aberration is a major factor in determining the quality of the retinal image, while HOA also must be considered. Zhao et al. [12] suggested that coma HOA influences the development of vision in children with amblyopia.
However, there have been conflicting conclusions regarding the correlation between higher and lower order aberrations. Some studies have shown that RMS magnitude is not correlated with refractive error when there is a broad range of refractive errors [813]. In normal eyes, no correlation has been found between wavefront aberration and refractive error [14]. However, Rossi et al. [14] reported that even cases of emmetropia and low myopia would benefit from HOA correction. HOA and its relationship to refractive error in children with hyperopic isometropic amblyopia have yet to be studied. Ziylan et al. [13] concluded that hyperopia has great potential to induce amblyopia. In our study, there was a significant correlation between astigmatism and HOA, especially coma HOA. In the case of myopic eyes, Karimian et al. [15] documented that astigmatism and coma HOA have a statistically significant correlation.
HOAs depend on many factors and increase in magnitude with age [1617]. However, Fujikado et al. [18] documented that corneal HOA was not significantly correlated with age. In addition, Brunette et al. [19] stated that ocular aberration decreases progressively until early adulthood, reaching a minimum level in the fourth decade of life and then increasing progressively with age. If the level of corneal HOA is high during childhood, it could affect visual acuity during vision development [20]. Those authors concluded that, during childhood, the concurrent thinning and f lattening of the lens, axial elongation of the eye, and change in corneal profile are oriented toward emmetropization of the eye and influence HOA. In our study, both lower and higher astigmatism groups showed decreased HOA level during amblyopia treatment. No statistically significant correlation was found between age and HOA type. Also, as our study was conducted for a relatively short period, we could not clearly identify why HOAs decreased during amblyopia treatment. Therefore, a large-scale study with longer follow-up would be helpful to explain the correlation between age and HOA.
Kwan et al. [21] reported that coma and spherical aberration are the most common HOA components in healthy individuals. Wei et al. [22] showed that among HOAs, third-order aberrations accounted for the highest RMS values in the Chinese population. In those studies, third-order coma accounted for the greatest percentage of HOAs. In the present study, coma HOA also had the largest RMS value among HOAs, followed by spherical aberrations and trefoil HOAs.
Plech et al. [23] stated that there was a greater percentage of astigmatism in children with isometropic amblyopia than in those with anisometropic amblyopia. Amblyopia was defined as a BCVA of 0.8 or less, and anisometropia was defined as a difference in sphericity of 3.0 D or more, and/or a difference in astigmatism of 2.0 D or more. We defined hyperopic isometropic amblyopia as bilateral hyperopia representing a difference in SE of 1.00 D or less between the eyes and a BCVA of 0.63 or less when the patient was younger than 6 years or 0.8 or less when the patient was aged 6 years or older. There is no standard definition as to a significant level of astigmatism. Currently, the American Association for Pediatric Ophthalmology and Strabismus Vision Screening Committee guidelines recommend that, for children older than 49 months, astigmatism greater than 1.50 D should be distinguish higherand lower-order groups. Therefore, we used 1.50 D astigmatism as a boundary to differentiate higher and lower astigmatism groups.
In this study, coma HOA showed a statistically significant correlation with astigmatism. There was a high level of coma HOA in the higher astigmatism group, and this correlated with astigmatism in the Pearson correlation test. Our results are in accordance with a recent report by Prakash et al. [7], showing that HOA, especially third-order aberration, could be a cause of idiopathic amblyopia. They said that differences between the two eyes in cases of idiopathic amblyopia could have been present since early childhood. This could have led to a bifoveal pattern disruption resulting in HOA-associated amblyopia and is especially important for third-order aberrations, which include coma and trefoil HOAs.
Zhao et al. [12] suggested that HOA, such as trefoil and coma, is linked to reduced visual acuity in amblyopia. A greater number of coma HOAs were noted in the amblyopic group compared with the emmetropic group. The authors concluded that this type of HOA affects vision quality. These results are partially in accordance with our observations, e.g. coma HOA was correlated with astigmatism.
The main limitation of our study was the lack of comparison group of children who did not undergo amblyopia treatment. Our study had a retrospective design, so further prospective studies with large scale, long-term follow-up would be helpful to elucidate the relationship between HOA and amblyopia. Further study will be needed to elucidate the clear mechanism of correlation between coma HOA and astigmatism.
In conclusion, coma HOA was significantly higher in the higher astigmatism group than in the lower astigmatism group and was correlated with astigmatism. The amblyopia treatment success rate was significantly lower in the higher astigmatism group than in the lower astigmatism group. This finding suggests that lower-order aberration, such as defocus and astigmatism, is a major factor determining vision quality, and HOA should be considered in amblyopic patients.
Figures and Tables
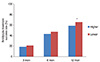 | Fig. 1Compiled patients with successful amblyopia treatment. Amblyopia treatment succeeded in 20 patients in the higher astigmatism group (56.82%) and 25 patients in the lower astigmatism group (66.79%) after 12 months of treatment. Higher = higher astigmatism group; Lower = lower astigmatism group. *There was a statistically significant difference in success rate between the higher and lower astigmatism groups at 12 months (p = 0.028). |
 | Fig. 2Comparison of total ocular higher-order aberration (HOA), ocular trefoil, ocular coma, and ocular spherical aberrations between the higher astigmatism group and the lower astigmatism group. (A) Ocular total HOA root mean square (RMS). (B) Ocular trefoil RMS. (C) Ocular coma RMS. (D) Ocular spherical RMS. Ocular coma RMS was significantly higher in the higher astigmatism group at 12 months follow-up. Higher = higher astigmatism group; Lower = lower astigmatism group. *p < 0.05, statistically significant, independent t-test. |
Table 1
Baseline characteristics of participants

Independent samples t-test. Values are presented as mean ± standard deviation (range).
D = diopter; HOA = higher-order aberration.
*Except value, Levene's test for equality of variances; †Astigmatism was significantly higher in the high astigmatism group (p < 0.05, statistically significant, independent t-test).
References
1. von Noorden GK, Campos EC, editors. Binocular vision and ocular motility: theory and management of strabismus. 6th ed. St. Louis: Mosby;2002. p. 246–251.
2. Flom MC, Bedell HE. Identifying amblyopia using associated conditions, acuity, and nonacuity features. Am J Optom Physiol Opt. 1985; 62:153–160.
3. Pediatric Eye Disease Investigator Group. The clinical profile of moderate amblyopia in children younger than 7 years. Arch Ophthalmol. 2002; 120:281–287.
4. Woodruff G, Hiscox F, Thompson JR, Smith LK. Factors affecting the outcome of children treated for amblyopia. Eye (Lond). 1994; 8(Pt 6):627–631.
5. Yoon GY, Williams DR. Visual performance after correcting the monochromatic and chromatic aberrations of the eye. J Opt Soc Am A Opt Image Sci Vis. 2002; 19:266–275.
6. Williams D, Yoon GY, Porter J, et al. Visual benefit of correcting higher order aberrations of the eye. J Refract Surg. 2000; 16:S554–S559.
7. Prakash G, Sharma N, Saxena R, et al. Comparison of higher order aberration profiles between normal and amblyopic eyes in children with idiopathic amblyopia. Acta Ophthalmol. 2011; 89:e257–e262.
8. Lee SH, Chang JW. The relationship between higher-order aberrations and amblyopia treatment in hyperopic anisometropic amblyopia. Korean J Ophthalmol. 2014; 28:66–75.
9. Liang J, Grimm B, Goelz S, Bille JF. Objective measurement of wave aberrations of the human eye with the use of a Hartmann-Shack wave-front sensor. J Opt Soc Am A Opt Image Sci Vis. 1994; 11:1949–1957.
10. Levy Y, Segal O, Avni I, Zadok D. Ocular higher-order aberrations in eyes with supernormal vision. Am J Ophthalmol. 2005; 139:225–228.
11. Dominguez-Vicent A, Perez-Vives C, Ferrer-Blasco T, et al. The effect of simulated normal and amblyopic higher-order aberrations on visual performance. J AAPOS. 2013; 17:269–275.
12. Zhao PF, Zhou YH, Wang NL, Zhang J. Study of the wavefront aberrations in children with amblyopia. Chin Med J (Engl). 2010; 123:1431–1435.
13. Ziylan S, Yabas O, Zorlutuna N, Serin D. Isoametropic amblyopia in highly hyperopic children. Acta Ophthalmol Scand. 2007; 85:111–113.
14. Rossi EA, Weiser P, Tarrant J, Roorda A. Visual performance in emmetropia and low myopia after correction of high-order aberrations. J Vis. 2007; 7:14.
15. Karimian F, Feizi S, Doozande A. Higher-order aberrations in myopic eyes. J Ophthalmic Vis Res. 2010; 5:3–9.
16. Oshika T, Klyce SD, Applegate RA, Howland HC. Changes in corneal wavefront aberrations with aging. Invest Ophthalmol Vis Sci. 1999; 40:1351–1355.
17. Wang L, Dai E, Koch DD, Nathoo A. Optical aberrations of the human anterior cornea. J Cataract Refract Surg. 2003; 29:1514–1521.
18. Fujikado T, Kuroda T, Ninomiya S, et al. Age-related changes in ocular and corneal aberrations. Am J Ophthalmol. 2004; 138:143–146.
19. Brunette I, Bueno JM, Parent M, et al. Monochromatic aberrations as a function of age, from childhood to advanced age. Invest Ophthalmol Vis Sci. 2003; 44:5438–5446.
20. Wu C, Hunter DG. Amblyopia: diagnostic and therapeutic options. Am J Ophthalmol. 2006; 141:175–184.
21. Kwan WC, Yip SP, Yap MK. Monochromatic aberrations of the human eye and myopia. Clin Exp Optom. 2009; 92:304–312.
22. Wei RH, Lim L, Chan WK, Tan DT. Higher order ocular aberrations in eyes with myopia in a Chinese population. J Refract Surg. 2006; 22:695–702.
23. Plech AR, Pinero DP, Laria C, et al. Corneal higher-order aberrations in amblyopia. Eur J Ophthalmol. 2010; 20:12–20.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download